Abstract
Psoriasis is a common, chronic inflammatory dermatosis, and patients with psoriasis often develop nail involvement. It is estimated that up to 90% of patients experience nail lesions at least once in their lifetime. Nail psoriasis (NP) occurs when psoriatic inflammation affects the nail matrix, nail bed, or both. The clinical manifestations of NP vary depending on the location and severity of the inflammation. Common signs include pitting, splinter hemorrhages, salmon patches, and distal onycholysis. Although cutaneous psoriasis is considered more severe in individuals with nail involvement, there is no clear relationship between the duration, severity, and clinical presentations of cutaneous psoriasis and NP patterns. NP is notable for an increased prevalence of arthritis among patients and is considered a significant clinical burden due to its association with arthritis and its slow or poor response to many therapeutic agents. Effective reassurance and patient education are essential components of NP management. This review summarizes clinical manifestations and diagnostic and therapeutic strategies for NP.
Key Points
1. Nail involvement is common in psoriasis. It is estimated that up to 90% of patients with psoriasis experience nail lesions at least once in their lifetime. Nail psoriasis (NP) poses a considerable burden, not only because it may cause functional impairment and pain but also it has been identified as a risk factor for the development of psoriatic arthritis.
2. NP has diverse clinical manifestations. It has been demonstrated that some features of NP are seen more commonly in patients with psoriatic arthritis. Detection of these features is crucial for proper patient management, since it may lead to complete change in the treatment strategies to prevent joint damage.
3. This review summarizes clinical manifestations and diagnostic and therapeutic strategies for NP.
INTRODUCTION
Psoriasis is a chronic inflammatory dermatosis affecting 1–2% of the global population.1 Nearly half of psoriasis patients experience nail involvement, with a lifetime risk of developing nail psoriasis (NP) reaching up to 90%.1,2 NP presents a significant clinical burden, not only because of its cosmetic impact but also due to its association with psoriatic arthritis (PsA).3 The increased prevalence of NP among patients with PsA4 indicates that NP may predict PsA development.5 Early detection of nail involvement in psoriasis is critical as it may lead to the timely diagnosis and management of PsA, preventing irreversible joint damage.5 Dermatologists play an important role in the multidisciplinary management of NP. Diagnosing NP in cases with isolated nail involvement without cutaneous psoriasis, which occur in about 5% of patients, can be challenging.1,6 This review explores the clinical manifestations, diagnosis, and treatment of NP, offering insights into diagnostic and therapeutic strategies for complex cases.
CLINICAL MANIFESTATIONS OF NAIL PSORIASIS
NP presents with various clinical manifestations. While cutaneous psoriasis is often considered more severe in individuals with nail involvement, there is no clear relationship between NP patterns and the clinical presentations of psoriasis.1 Psoriasis can manifest in four primary clinical variants: plaque psoriasis, guttate psoriasis, erythrodermic psoriasis, and pustular psoriasis. For example, erythrodermic psoriasis, a potentially life-threatening condition, may present with distal onycholysis on a few fingernails; whereas acral pustular psoriasis, a subtype affecting the hands and feet, may result in onychodystrophy affecting all nails. A rare variant of acral pustular psoriasis, acrodermatitis continua of Hallopeau (ACH),7 is characterized by vesiculopustular lesions on the distal phalanges and is a nail disease.8 The European Rare and Severe Psoriasis Expert Network (ERASPEN) classifies ACH as a localized pustular psoriasis, characterized by persistent (>3 months) sterile pustules affecting the nail apparatus.9 Palmoplantar pustulosis, the other variant of acral pustular psoriasis, can cause nail lesions in a mild or severe pattern. Nails are always affected in ACH but not in palmoplantar pustulosis.9
The most common NP findings include pitting, distal onycholysis, splinter hemorrhages, and salmon patches. Nail lesions arise when psoriatic inflammation affects the nail bed, nail matrix, or both. Damage to the nail matrix leads to clinical signs such as pitting, Beau’s lines, leukonychia, trachyonychia, red spots on the lunula, thick nail plates, and nail plate crumbling. Conversely, involvement of the nail bed results in distal onycholysis, splinter hemorrhages, salmon patches, and subungual hyperkeratosis.1,10 Pustular psoriasis causes pustules within the nail bed in ACH, which results in nail plate destruction.8
Findings of NP vary among patients, and patients generally manifest with both nail bed- and matrix-related findings. However, in some patients, nail bed-related findings typically appear together, whereas in others, matrix-related findings cooccur. One of the most common NP patterns involves distal onycholysis, splinter hemorrhages, and salmon patches coinciding with pitting, the most common matrix-related finding (Figure 1). Pitting, being the most common matrix-related finding, can occur alone or alongside other lesions. It can be diffusely scattered or localized in a few areas.11,12 Pitting can also occur in other nail diseases, such as alopecia areata, lichen planus, and dermatitis. Psoriatic pits are deeper and irregular and give the nail a rough appearance when compared with pits caused by other nail diseases. Alopecia areata is a common disease, in which pitting is frequently observed. Pits in alopecia areata are generally evenly distributed and superficial and give a shiny appearance.13,14 Ten pits in one nail or more than 50 pits on all nails have been considered evidence of psoriasis.1 Although pitting is not a pathognomonic lesion for NP, it may be a diagnostic finding if these criteria are met.

Figure 1: Clinical image of a patient with psoriasis.
Note sharply demarcated, silvery scaly, erythematous plaques and typical lesions of nail psoriasis, including distal onycholysis with erythematous border, salmon patches, pitting, and Beau’s lines.
Salmon patches are NP-pathognomonic lesions representing psoriatic plaques on the nail bed. When they are seen, clinicians can make an accurate diagnosis of NP. They are translucent, amber-colored, yellowish-red to yellowish-brown spots on the nail bed that resemble oil droplets. In general, they have an erythematous rim, which is a very characteristic finding for NP. Distal onycholysis in NP also has the typical erythematous border. Salmon patches and distal onycholysis are related lesions in NP. When a salmon patch reaches the hyponychium, the parakeratosis that causes it breaks out, and distal onycholysis develops.1,11,12 This erythematous border distinguishes psoriatic onycholysis from distal onycholysis seen in other diseases, such as onychomycosis and traumatic onycholysis.1,11,12,15,16
Dermoscopic features of NP include distal onycholysis with erythematous border, salmon patches, splinter hemorrhages, nail bed red spots, red spots on the lunula, longitudinal erythema of the nail bed, mottled lunula, fuzzy lunula, pitting, multiple white dots, dilated nail bed capillaries, dilated hyponychial capillaries, subungual hyperkeratosis, nail plate crumbling, and pseudopitting.11,12,17 Pseudopitting is a recently described feature of NP, which is characterized by pits seen above salmon patches.17 However, there are nonspecific NP lesions that are matrix-related and visible to the naked eye. Trachyonychia, longitudinal ridging, leukonychia, Beau’s lines, and nail plate thickening are among them, and they can be seen in other diseases, such as onychomycosis, lichen planus, and idiopathic trachyonychia.1,10,14,15,18,19 Differentiation of NP from these diseases is mainly based on the detection of characteristic NP lesions, such as salmon patches or distal onycholysis with erythematous border.11
DIAGNOSING NAIL PSORIASIS
NP is generally easy to diagnose when typical skin and nail lesions are present. Psoriasis has distinctive skin lesions that are mostly sharply demarcated, silvery scaly, erythematous papules and plaques on the scalp, lumbosacral region, and extensor surfaces of the elbows and knees.7 However, in isolated NP cases or atypical presentations, dermoscopy or a nail biopsy may be required. While histopathology remains the gold standard for NP diagnosis, nail biopsy is rarely used due to its invasiveness. Several characteristic and common dermoscopic features of NP have been described (Figure 2), allowing clinicians to make an accurate diagnosis of NP without the delay and discomfort associated with the nail biopsy procedure. Furthermore, nail biopsy requires expertise. Unless the tissue specimen is taken from a specific area, nail biopsy in NP is usually associated with diagnostic errors.1,11,12
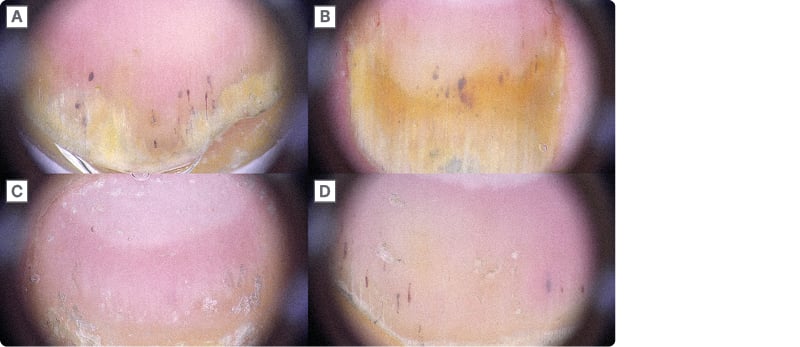
Figure 2: Dermoscopic features of nail psoriasis.
A) Distal onycholysis with erythematous border, splinter hemorrhages, and dilated nail bed capillaries. B) A large salmon patch. C) Diffuse pitting. D) A typical combination of features; nail bed-related findings cooccur with pitting.
Dermoscopy, a non-invasive imaging technique, has proven effective in diagnosing NP and differentiating it from other nail disorders, such as onychomycosis, lichen planus, trachyonychia, and nail trauma.1 Onychomycosis has typical dermoscopic features such as longitudinal streaks and patches, a jagged proximal edge with spikes of the onycholytic area, subungual hyperkeratosis, brown-black pigmentation, multicolored pigmentation, and leukonychia. Onychomycosis is distinguished from other nail diseases by its whitish-yellow longitudinal streaks and patches.15 However, the most significant difference between onychomycosis and NP is distal onycholysis. Onychomycosis has a jagged proximal edge, whereas NP has a round linear proximal edge and an erythematous border.1,11,12,15
Nail lichen planus is another nail disorder frequently mistaken for NP. Typical clinical features include pterygium unguis, longitudinal ridging, fissuring, distal splitting, subungual hyperkeratosis, onycholysis, trachyonychia, red lunula, and onychoatrophy. Pterygium, a typical sign of lichen planus, is easily visible to the naked eye. However, dermoscopy is particularly useful for detecting subtle changes, such as red lunula.18,20
Common nail lesions associated with traumatic nail dystrophy include thickened nail plates, yellowish discoloration, leukonychia, splinter hemorrhages, and distal onycholysis. Although the patient’s history often reveals the diagnosis, distinguishing nail trauma from NP can be challenging. One of the most significant differences is the presentation of distal onycholysis. Nail trauma typically causes distal onycholysis with a proximal linear edge, surrounded by a typical pale pink bed. In contrast, NP presents with an erythematous border around distal onycholysis. Dermoscopy in nail trauma often reveals hemorrhagic spots and streaks, the primary indicators of subungual hemorrhage. Although splinter hemorrhages are common in NP, they do not follow a globular pattern. Nail trauma, however, is characterized by peripheral fading and satellite globules associated with subungual hemorrhage.16
TREATMENT OF NAIL PSORIASIS
Treating NP is often challenging. Compared with cutaneous lesions, nail lesions improve slowly due to the slow growth rate of the nail plate. Topical treatments are less effective because of limited drug penetration through the nail plate. Systemic treatments are recommended for cases with widespread cutaneous involvement and PsA. In isolated NP or cases with limited cutaneous involvement, treatment decisions require careful consideration of the safety and economic implications of systemic treatments. The best approach to treating NP involves a patient-centric strategy, as the disease causes pain, functional impairment, and a significant reduction in quality of life. General prophylactic measures, such as avoiding minor trauma, are recommended for all patients. Physician–patient shared decision-making is crucial, particularly in challenging cases like isolated NP.1,21-24
All patients should be advised to follow general prophylactic measures. For instance, patients should avoid behaviors that trigger Koebnerization, such as nail biting, manicures, and wearing tight-fitting shoes. Gloves should be worn during wet or dirty work, and frequent contact with water should be avoided. Hands and feet must remain dry, and nails should be kept short. Emollients should be applied liberally to all nail surfaces.22
Systemic agents are recommended for patients with moderate-to-severe cutaneous psoriasis. However, patients with mild skin disease or no cutaneous involvement may receive either topical or systemic treatment, depending on individual cases. Patients with PsA should receive systemic treatments regardless of nail and skin severity. According to expert consensus, for patients with no or mild cutaneous involvement, the number of nails affected can determine whether topical or systemic therapy should be used. For instance, patients without cutaneous involvement or with mild skin disease who have NP in up to three nails should receive topical therapy, whereas those with NP in more than three nails may receive either topical or systemic therapy.1,22
Topical treatments include corticosteroids, vitamin D analogs, retinoids, calcineurin inhibitors, and keratolytic agents. Topical corticosteroids are the cornerstone of treatment. Potent and superpotent topical corticosteroids are typically preferred due to limited drug penetration through the nail plate. They can be applied once or twice daily, with or without occlusion, for 4–6 months. Intermittent therapy is usually preferred over continuous therapy to minimize side effects such as skin atrophy, telangiectasias, and tachyphylaxis.1,21-24
Patients with PsA or moderate-to-severe cutaneous psoriasis should receive systemic treatment, as nail lesions improve in tandem with cutaneous lesions. Several systemic therapeutic agents are available for NP, including conventional antipsoriatics such as methotrexate, cyclosporin A, and acitretin, which vary in effectiveness. Additionally, small molecules like apremilast and biologics have expanded treatment options for NP. Biologics, TNF-α inhibitors (etanercept, adalimumab, certolizumab, infliximab), IL-17 inhibitors (secukinumab, bimekuzumab, brodalumab, ixekizumab), IL-12/23 inhibitor (ustekinumab), and IL-23 inhibitors (tildrakizumab, guselkumab, risankizumab) are highly effective in treating psoriasis because they inhibit specific immune pathways. However, they are more expensive. They have a favorable safety profile compared to conventional systemic therapies, yet they can be associated with severe side effects. TNF-α inhibitors should be avoided in patients with congestive heart failure, a personal or family history of demyelinating disease, and a malignancy history. IL-17 inhibitors should be avoided in patients with inflammatory bowel disease. Suicidal ideation has been shown in patients receiving brodalumab and bimekizumab, thus they should be avoided in patients with a history of mental health disorder. Detailed examination is vital in patients with a history of malignancy or hepatitis B and C infections when prescribing IL-23 inhibitors. 1,21-25 New therapeutic options are being sought in the management of NP, including lasers.26 All NP treatments require a long time to show their effects, and treatment success depends not only on the therapeutic agent’s type and effectiveness but also on patient-related factors.1,21-24






