Abstract
The use of dermoscopy in general dermatological practice has recently increased. Its non-invasive nature means it is being practiced frequently by dermatologists to diagnose various skin conditions. Dermoscopy, also known as dermatoscopy, allows dermatologists to quickly visualise skin structures up to the papillary dermis level. The skin patterns seen under dermoscopy are usually due to pigment and vascular structures; melanin and haemoglobin play major roles and give different patterns depending on the skin condition and pathological changes. Many inflammatory diseases are encountered by clinicians in daily practice; at times they are indistinguishable to the naked eye and a biopsy is required to confirm the diagnosis. Dermoscopy is a useful tool in the diagnosis and differentiation of inflammatory skin conditions and is aptly termed inflammoscopy when used in these situations. Inflammoscopy demonstrates the distinct characteristic patterns of many conditions and aids accurate diagnoses. In this article, the importance of dermoscopy in the diagnosis of relatively common inflammatory conditions, such as eczema, psoriasis, lichen planus, pityriasis rosea, pityriasis lichenoides et varioliformis acuta, pityriasis lichenoides chronica, and discoid lupus erythematosus, is highlighted. Here, an overview of dermoscopic patterns in each of these conditions is emphasised.
INTRODUCTION
Dermoscopy is a non-invasive diagnostic method that aids in the visualisation of surface and subsurface skin structures, leading to accurate diagnoses. In the past, it was used for pigmented lesions to differentiate melanoma from benign melanocytic lesions.1 Recently, awareness and knowledge of dermoscopy have increased tremendously in many countries. Dermoscopy has expanded its applications not only to inflammatory but also to infectious conditions, with inflammoscopy being the term used for dermoscopic examination of inflammatory conditions.2 Different names are given to dermoscopy based on the site as well as disease condition; trichoscopy is used for scalp and hair disorders, inflammoscopy for inflammatory conditions, and entomodermoscopy when infestation and infectious conditions are examined under dermoscopy.3
Dermoscopy demonstrates the characteristic and often specific patterns of a skin condition, enabling physicians to diagnose the skin disease accurately. All patterns visualised using dermoscopy depend on the location and distribution of melanin and haemoglobin pigment in the skin layers.4 This paper emphasises the utility of dermoscopy in the diagnosis of inflammatory conditions. In this review, the dermoscopic patterns of psoriasis, lichen planus (LP), pityriasis rosea (PR), prurigo nodularis (PN), eczema, pityriasis lichenoides et varioliformis acuta (PLEVA), pityriasis lichenoides chronica (PLC), and discoid lupus erythematosus (DLE) are described and their importance is highlighted. In inflammoscopy, accurate diagnosis can be made by considering criteria such as scale, lesion colour, type of vessels, and vessel arrangement and background colour.5
STUDY AND DATA SELECTION
Articles and chapters were screened in journals and textbooks, respectively, for information on dermoscopy of inflammatory conditions. Both original and review articles were included. Articles describing the dermoscopic patterns of inflammatory skin conditions were selected. MEDLINE, PUBMED, and EMBASE were screened up to 2017.
DISCUSSION
The Basics of Dermoscopy
Normally, unaided eyes cannot visualise subsurface structures because incident light is reflected and some of this light gets absorbed. This is due to the differences in the refractive indices of the stratum corneum (1.55) and air (1.00), a phenomenon known as specular reflectance or glare. This is prevented by using an interface medium, which is applied onto the skin before a dermoscopic examination. Isopropyl alcohol, water, liquid paraffin, and ultrasound gel are all used as interface media fluids. This type of dermoscopy, wherein the dermoscope comes into contact with skin lesions, is known as non-polarised dermoscopy. Many authors state that contact with the skin surface results in nosocomial infections; this is avoided by using non-contact dermoscopy with polarised lights. The non-polarised method of dermoscopy assists in the recognition of superficial structures such as scales, milia-like cysts, and comedo-like openings, whereas the polarised mode helps in the visualisation of vessels and their arrangement, pigmentation, and dermal collagenous elements. Newer, hand-held dermoscopes have an inbuilt mode that changes from the polarised to the non-polarised technique with a click of a button. This is referred to as a blink sign.4,6
Psoriasis
Psoriasis is a common, chronic, disfiguring, inflammatory, and proliferative condition of the skin, characterised by red, scaly, sharply demarcated, indurated plaques, present particularly over extensor surfaces and the scalp.7 Lallas et al.8 studied dermoscopy of psoriasis and described dotted or coiled (glomerular) vessels arranged regularly. Though dotted vessels can be seen in other inflammatory dermatosis, the uniformity and homogenous distribution is characteristic of psoriasis (Figure 1). In histopathology studies, the presence of red dots corresponds with the loops of vertically arranged vessels within the elongated dermal papillae.8 Errichetti et al.9 differentiated PLC from guttate psoriasis dermoscopically and stated that orange-yellow structureless areas and dotted and no-dotted vessels are characteristic in PLC, whereas diffuse dotted vessels are specific to psoriasis.
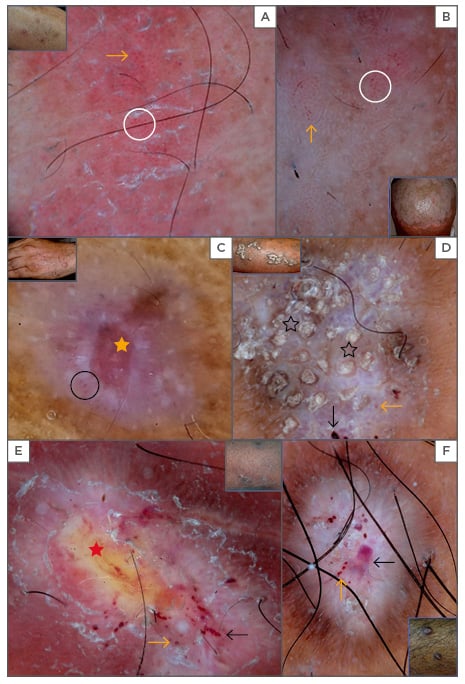
Figure 1: Dermoscopy of psoriasis shows scaling and regular red dots (orange arrows), which are regular and uniform on the dull red background. Few glomerular vessels (white circle) are noted (A). A red background is not prominent on the scalp (B). Lichen planus reveals annular white ring (Wickham striae); red areas (orange star), and linear vessels (black circle) are present at the periphery (C). Corn pearls (black stars), blue-grey areas, red globules, and peripheral brownish striations are present in hypertrophic lichen planus (D). In prurigo nodularis yellowish areas (red star), white areas, red dots, and clods (black arrows) are present in excoriated lesions (E) as well as bright white areas in a starburst pattern with red dots and clods in late lesions. Note the peripheral brownish striations (F).
Vázquez-López and Manjón-Haces7 described the dermoscopic subpatterns of psoriasis as round capillaries (red globules) arranged in irregular circles or rings with a beaded, lacelike capillary appearance, termed red globular rings. These patterns are infrequently observed in a minimal number of cases of plaque psoriasis and are considered diagnostic. Two important additional findings, along with vascular pattern, are the presence of white scales and a light red background. Kibar et al.10 observed two new dermoscopic signs that are specific to scalp psoriasis, namely signet ring vessels and hidden hairs. Apart from diagnosis, dermoscopy plays an important role in monitoring the disease. The number of twisted vessels visualised using high magnification represents the activity of the disease and the number of these vessels reduces in response to treatment.11 Errichetti et al.12 described the dermoscopic patterns in erythrodermic psoriasis, which revealed a monomorphous pattern, with diffusely distributed white-coloured scales and regularly arranged dotted/glomerular vessels on a fairly homogeneous red-coloured background. Although dermoscopy of psoriasis shows dotted vessels, in palmar psoriasis only diffuse scales are visible due to the thickness of these scales. Scales should be scraped in order to see the dotted vessels.13 Clinical diagnosis of psoriasis is straightforward if the presentation is typical, consisting of silvery-white scales on an erythematous background. Atypical clinical presentations require a biopsy, which is invasive. However, this limitation is overcome by using dermoscopy, because of its non-invasive nature; the role of dermoscopy in the diagnosis of psoriasis is well established.
Lichen Planus
LP is an inflammatory dermatosis of the mucocutaneous surfaces that can present with a variety of clinical manifestations. Classical lesions of LP present as polygonal, flat-topped, violaceous papules and plaques, superimposed with reticulated white scale, termed Wickham striae (WS). Visualisation of this subtle but specific finding in LP can be enhanced by the application of water or oil to the affected area. Dermoscopy enables the visualisation of WS, which has been assessed as a highly sensitive and specific criterion for the diagnosis of LP (Figure 1). WS correspond to compact orthokeratosis above zones of wedge-shaped hypergranulosis and acanthosis, centred on acrosyringia and acrotrichia.8,14 WS is classically seen as white crossing lines on dermoscopic evaluation and defined as ‘reticular pattern WS’. Güngör et al.15 described various other patterns of WS, including leaf veination, circular, radial streaming, linear, globular, annular, perpendicular, veil-like structureless, and a combination of these patterns. Reticular pattern is the most common pattern of WS.
The evolution of LP lesions can be monitored using dermoscopy. Early active lesions show WS arranged in a starburst pattern with a central thick white structure that expands into radial striations towards the periphery. The WS border shows projections of varying sizes, from thin spikes (comb-like appearance) to broad arboriform ramifications that may come together in networks. Prominent linear vessels are usually intermingled with the WS border projections (radial capillaries).16
In matured lesions of LP, the arrangement of WS is usually seen as a reticular pattern and vascular structures are well established, appearing as red globules, dots, and linear striations. The pigment pattern appears at this stage as pigmented dots or globules scattered in the lesion.15 In regressing lesions of LP, WS disappears and the pigmented network becomes more prominent. The pigment pattern at this stage appears as radiating streaks at the periphery of the lesion, grey-black structureless areas, grey-black linear streaks, or grey-black pigment dots. The distribution pattern of grey-black streaks and dots suggests that they represent a previous location of WS.15 In hypertrophic LP (HLP), corn pearls or comedo-like openings and yellow areas are observed in addition to the aforementioned patterns.17 Dermoscopy of LP gives many characteristic patterns that differentiate LP from other conditions, and it is particularly helpful in visualising unusual manifestations and LP coexisting with other conditions.
Prurigo Nodularis
PN is a chronic neurodermatitis that presents with intensely pruritic nodules that are secondary to an intense itch-scratch cycle.18 Errichetti et al.19 have noted pearly white areas in the centre, extending peripherally in a starburst pattern in PN. The patterns differ with respect to duration and type of lesion. Early and excoriated lesions show white areas, white scale, yellow erosion/crust, dotted or glomerular vessels, and haemorrhagic spots. Late and hyperkeratotic lesions demonstrate similar patterns in variable frequencies except for yellow erosion (Figure 1).19 Follicular plugging is an additional feature present in late lesions of PN.19
Dermoscopically, nodular scabies, multiple keratoacanthoma, and HLP can be differentiated. Nodules in scabies that indicate mites or burrows appear as a hang glider sign, or show a jet with contrails.20 Keratoacanthoma presents with a central white crust with peripheral hair pin and linear vessels.21 HLP shows pearly white areas in the centre that differ from the white area seen in PN. In HLP, white areas do not cover the entire lesion; instead, they extend peripherally and are less prominent. Comedo-like openings are characteristically seen in HLP irrespective of the duration of lesions. Grey-blue globules that correspond to melanin in the dermis are seen in HLP but not in PN.17
Peripheral brownish striations extending from white areas are also described as characteristic features of PN. These represent melanin deposited in elongated rete ridges as a result of inflammation. White areas correspond to dermal fibrosis. In the author’s experience, yellowish areas (representing discharge), brown and black dots, and globules (representing post inflammatory pigmentation) are new dermoscopic observations in PN. Hence, patterns of dermoscopy in PN vary according to the duration and evolutionary stage of the lesions. Early lesions demonstrate erosion, yellow areas, and ‘crusts’ and in late lesions, black or brown dots and follicular plugs are visualised. The white, starburst pattern is seen in all lesions irrespective of the lesion duration.
Discoid Lupus Erythematosus
DLE presents as erythematous patches and plaques with adherent scale and hyperpigmented borders. Photo-exposed areas are most commonly affected, but shaded sites such as the trunk and back are involved in generalised DLE.22 The patterns of dermoscopy in DLE vary according to the stage of disease. Erythema, perifollicular whitish halo, follicular keratotic plugs, red dots, branching telangiectasia, and white scaling are the most characteristic features of early lesions (Figure 2). These patterns correspond to inflammation, follicular pathology, and vessel involvement.23 Late lesions demonstrate white-coloured structureless areas, hyperpigmentation in the form of a honeycomb network, perifollicular pigmentation, and a sprinkled pattern with blurred telangiectasias. The white areas represent fibrosis and the pigmentation is due to melanophages.24 Diffuse hyperkeratosis, dilated follicles, and yellowish scales are examples of less commonly encountered dermoscopic patterns.25
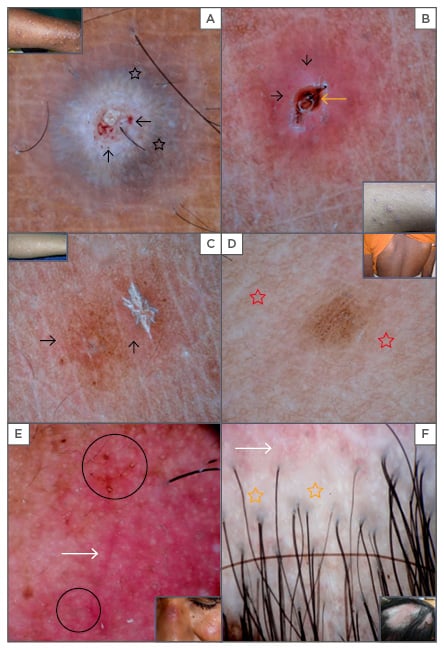
Figure 2: Dermoscopy of pityriasis lichenoides et varioliformis acuta shows white-yellow, structureless areas with crust, grey-blue radiating strands (black stars), red dots, and globules (black arrows) (A). Amorphous brownish area (orange arrow) and red dots (black arrows) at the periphery are noted (B). Pityriasis lichenoides chronica shows brownish structureless areas and red dots with a micaceous scale (C) and white-coloured areas (red stars) surrounding brown areas are noted (D). Discoid lupus erythematosus shows erythema, dilated follicles (black circles), telangiectasia (white arrows), and scaling (E), as well as the loss of follicular ostia, white areas (orange stars), and telangiectasia (white arrows) (F).
Pityriasis Lichenoides et Varioliformis Acuta
PLEVA is an acute inflammatory condition characterised by follicle-oriented pustules and crusts.26 PLEVA can mimic various skin conditions such as chicken pox, lymphomatoid papulosis, guttate psoriasis, LP, and PR. Dermoscopic patterns give clues to the diagnosis: white-coloured, structureless areas, a central crust, red globules, blue-grey areas, yellow globules, and scaling are described in the literature as features of PLEVA (Figure 2).27 Authors described dermoscopic patterns in PLEVA that differ between early and late lesions. In the former, an amorphous brownish area around the hair follicles, within a rim of white scale and dotted vessels at the periphery, are noted; white-coloured, structureless areas and a central crust-plug surrounded by a rim of white scale, red dots and haemorrhages are observed in late phase lesions.26 Vascular patterns vary from dots, to linear, to haemorrhages and are arranged either in a targetoid or dotted pattern.26,27 Ankadand Beergouder26 described new findings that correlated with histopathological changes, including focal blue-grey areas and yellow globules that represent melanin in the dermis and spongiosis and basal cell degeneration, respectively. Dermoscopic patterns correlate well with histopathological changes. Hence, by recognising clinical features and using dermoscopy, the diagnosis of PLEVA can be assumed.
Pityriasis Lichenoides Chronica
PLC clinically presents as purpuric macules and papules with micaceous scales on the surface that are adherent. Lesions heal with hypopigmented areas especially in skin Type 4, 5, and 6. PLC can be confused with guttate psoriasis and therefore dermoscopy plays an important supportive role in the diagnosis of PLC. The most peculiar dermoscopic findings in PLC include orange-yellowish structureless areas, focally distributed dotted vessels and milky-red globules, and linear irregular and branching vessels (Figure 2).3 Errichetti et al.9 described dermoscopic differentiation of guttate psoriasis and PLC. Guttate psoriasis demonstrates regularly arranged red dots on a dull red background, whereas an orange-yellowish background with linear and dotted vessels is characteristic of PLC.
However, in the authors’ experience, brown structureless areas and white scaling in the centre, with dotted vessels and hypopigmented areas in the periphery are common, characteristic findings in PLC of melanin-rich skin. Linear vessels are not usually seen. We believe that differences in skin colour are contributing to the different background colours seen in PLC. A brownish background is likely due to haemosiderin deposition (due to extravasated erythrocytes), melanophages (focal basal cell degeneration), and lymphocytic infiltration.
Pityriasis Rosea
PR is a papulosquamous disease characterised by erythematous papules and plaques with peripheral scaling that is classically described as collarette scaling. Clinical differentiation of PR from dermatophytosis and psoriasis is difficult in unusual presentations.28 Dermoscopy of PR is well established and both herald and daughter patches demonstrate typical patterns under dermoscopy. It shows diffuse and structureless yellow-orange areas, and characteristic focal white-coloured peripheral scaling (Figure 3). Red dots, different from those seen in psoriasis, may be seen at the periphery but are less evident.8,28
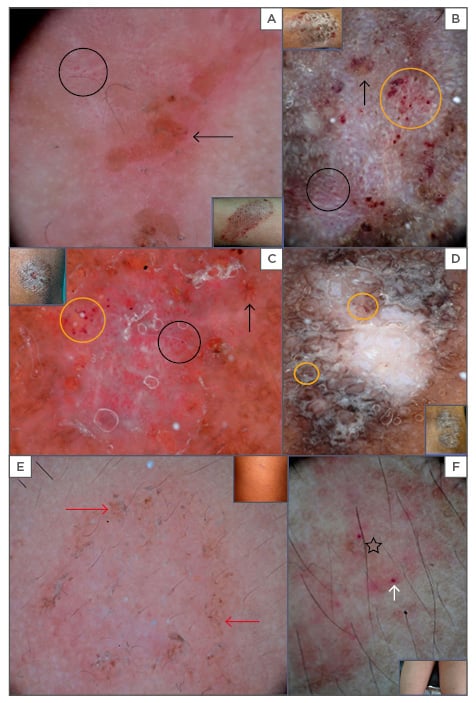
Figure 3: Dermoscopy of eczema reveals a yellow-orange crust, (A: asteatotic), yellow serocrusts (black arrow), and curvilinear white globules on a white background (B: subacute). Red dots are arranged in a regular (black circle) and cluster pattern (orange circle) (A, B, C, D). Nummular eczema shows focal white scales, a yellow-orange crust, red dots (C), diffuse white areas, and patchily arranged red dots (D: lichen simplex chronicus). Pityriasis rosea is shown by brown dots (red arrows), collarette scales on a yellow-brown background (E: late lesion), scale, and a brown globule (black star); milky pink dots and globules (white arrow) are noted in early lesions (F: early lesion).
These findings ensure dermoscopic differentiation of PR from other papulosquamous conditions. In psoriasis, red dots in regular patterns and scales are seen on a red background. A yellow or brown colour under dermoscopy is a negative factor for psoriasis;29 however, the authors have observed brownish yellow backgrounds and brown dots in these patients, corresponding to the spongiotic tissue reaction plus haemosiderin deposits from extravasated red blood cells and lymphocytic infiltrate. A pronounced brownish hue on the background is related to the colour of the skin. This peculiar finding is frequently seen in late lesions of PR. Similarly, in early lesions, where pathological changes are not well formed, dermoscopy shows milky-red globules, indicating extravasated red blood cell in the dermis. Brown areas are very minimal suggesting early deposition of haemosiderin in the dermis. It is proven beyond doubt that dermoscopy demonstrates characteristic patterns in PR. Thus, patterns of PR seen under dermoscopy are accurate.
Eczema
Eczema presents with patches and plaques on the extremities. Clinically, it mimics psoriasis, dermatophytic infection, and LP. Dermoscopy of eczema shows a yellow coloured serocrust and clusters of red dots and white scales (Figure 3). Lallas et al.8 evaluated the dermoscopic patterns of eczema and opined that patterns may change depending on the stage of the eczema. In the acute stage, yellowish crusts, dotted vessels in a patchy distribution, and focal white scales are seen. In the chronic and lichenification stages, white scales and clusters of red dots are noted.8
In one study, dermoscopic patterns of hand eczema and palmar psoriasis were studied extensively. Eczema showed clusters of red dots, whereas psoriasis was characterised by diffusely arranged red dots. Yellow findings were specific to eczema.13 In all types of eczema, vascular patterns are repetitive and the patchy distribution of red dots is very specific. However, focal white scales, yellowish serocrusts, and white areas are predominantly seen in acute and chronic stages of eczema, respectively.13 Yellowish serocrusts correspond to spongiosis and serous discharge and white areas correspond to hyperkeratosis and acanthosis. A yellowish hue is characteristic of acute eczema and is referred to as ‘yellow clod’ sign.30
However, with 10x magnification, the authors have noticed a presence of red dots and globules, especially in asteatotic and subacute eczema, in the same way as that of psoriasis. They are of different sizes and shapes, unlike in psoriasis where they are the same size, both uniform and regular. This dermoscopic finding is explained by the fact that chronic scratching and rubbing result in psoriasiform hyperplasia. This results in diffusely arranged red dots over the entire lesion. This is a preliminary finding; further elucidation is required for this observation. Dermoscopy of erythrodermic atopic dermatitis consists of
yellowish scales/serocrusts and clusters of dotted vessels on a pinkish background. Non-specific,
sparse white-coloured scales may be observed.12 These findings help clinicians to differentiate inflammatory conditions that present with erythroderma.
CONCLUSION
Dermoscopy is an in vivo method of diagnostic technique that enables the clinician to visualise the skin structures not seen by the naked eye. By supplying higher magnification of a lesion, dermoscopy provides a detailed analysis of the lesion, allowing the accurate diagnosis and treatment. Hence, dermoscopy is considered the stethoscope of dermatologists. Thus, the authors recommend dermoscopic examination of skin lesions in daily practice.







