Polymorphic eruption of pregnancy (PEP), also known as pruritic urticarial papules and plaques of pregnancy, is a self-limiting inflammatory dermatosis that usually affects primiparous women in the last few weeks of pregnancy. PEP follows a benign course with spontaneous resolution, typically within 2 weeks postpartum, posing no increased risk of fetal or maternal morbidity other than maternal pruritus.1–3 When confronted with a pruritic skin eruption associated with pregnancy or the immediate postpartum period, prompt evaluation and diagnosis is vital because more aggressive eruptions, such as gestational pemphigoid (GP), need to be excluded. At the 27th Congress of the European Academy of Dermatology and Venereology (EADV) in Paris, France, we presented an unusual case of PEP with postpartum onset.
A 33-year-old woman presented with a widespread, intensely pruritic eruption within abdominal striae, spreading to the inferior extremities and buttocks, with no periumbilical involvement (Figure 1). The eruption had appeared 3 weeks postpartum. Due to the uncommon postpartum onset and anxiety of the patient, a skin biopsy was performed. Histopathology showed mild epidermal hyperplasia, spongiosis and parakeratosis with dermal oedema, and perivascular and interstitial lymphocytic infiltrate containing eosinophils. Direct immunofluorescence demonstrated nonspecific granular deposits of C3 and IgM. No other laboratory abnormalities were present. The clinical and histologic pictures were diagnostic for PEP. The eruption subsided following a 2-week course of topical methylprednisolone aceponate, tapered to one application daily for another week.
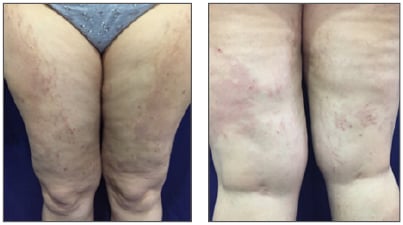
Figure 1: Antero-posterior view of inferior extremities involvement of a widespread, intensely pruritic eruption presented by a 33-year-old woman at 3 weeks postpartum. Note the distribution of lesions within striae distensae.
The diagnosis of PEP is mostly clinical, based on the patient’s history and physical examination. Although a skin biopsy is not usually necessary for diagnosis, it may be performed in cases of diagnostic uncertainty, especially to rule out more aggressive eruptions associated with pregnancy, such as GP, which can mimic PEP in the early urticarial phases. Direct immunofluorescence helped distinguish these two entities. Nonspecific granular deposits of C3 and IgM or IgA at the dermal–epidermal junction or surrounding blood vessels can be seen in approximately 30% of PEP cases,4 whereas in GP these deposits are linear. Indirect immunofluorescence is always negative in PEP. Other conditions that can mimic PEP include drug reactions, scabies, and viral syndromes.2,4 Differentiation among these entities is made by clinical history, routine histology, and serology. There are no related laboratory abnormalities to PEP.3
PEP prognosis is excellent, with spontaneous resolution within a few weeks and no tendency to recur with subsequent pregnancies. There is no increased risk of fetal or maternal morbidity, other than the maternal pruritus.2,3 The goal of treatment is relief of symptoms, which can usually be achieved following short-term use of topical corticosteroids and oral antihistamines.







