Neutrophilic dermatosis may have various clinical presentations, but these all share common histopathological manifestations with an aseptic infiltrate of polymorphonuclear neutrophils. Neutrophilic dermatosis of the hands (NDH) is a recently described disorder of which we present two cases and discuss the aetiopathogenic link to Sweet’s syndrome (SS).
Patient 1 was a 60-year-old woman, with no relevant medical history, who presented with an acute and painful eruption of both hands with fever preceded by an upper respiratory tract infection. Clinical examination showed erythematous oedematous lesions surmounted by pustules that covered the thenar eminences of both palms (Figure 1A). Histological findings were predominantly neutrophilic infiltration in the dermis with leukocytoclastic vasculitis. A diagnosis of NDH was made and all the lesions disappeared rapidly without relapse under oral prednisone.
Patient 2 was a 52-year-old woman who presented with very painful, well-defined erythematous, markedly oedematous plaques and pustular bullae over the thenar eminence of the left hand (Figure 1B). These lesions had gradually progressed for 4 weeks, following percutaneous trauma while handling fish, and failed to respond to several antibiotics. Laboratory investigations showed neutrophil leukocytosis in peripheral blood. A biopsy was taken from a section of the lesion which revealed diffuse and dense neutrophilic infiltrate in the dermis (Figure 2). Based on clinical and histopathological findings, a final diagnosis of NDH was made. The patient responded promptly to treatment with oral prednisone.
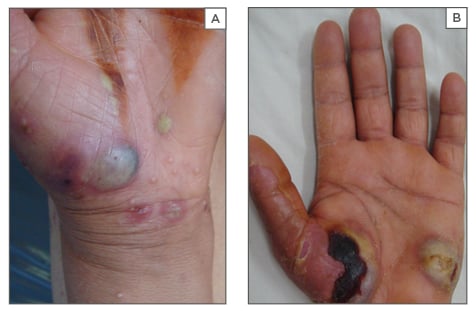
Figure 1: Erythematous oedematous lesions surmounted by pustular and haemorrhagic bullae over the thenar eminences of both patients.
A: Patient 1; B: Patient 2
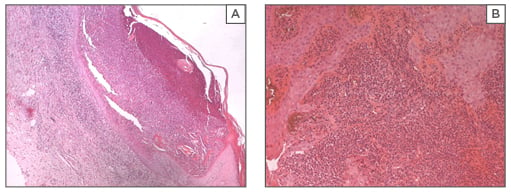
Figure 2: Diffuse and dense neutrophilic infiltrate in the dermis (haematoxylin and eosin X100).
A: Patient 1; B: Patient 2.
NDH is a rare entity that was first described in 1996 by Strutton et al.1 The eruption observed in our two patients was clinically and histologically suggestive of neutrophilic dermatosis with several similarities to SS: pyrexia, preceding upper respiratory tract infection, cutaneous pathergy, abnormal laboratory values, dense neutrophilic infiltrate, and prompt response to steroids culminating in support that this disease is a localised atypical form of SS.2 Similar to SS, NDH has also been associated with other conditions including malignancies.3 However, many findings and observations, both in the literature and in the two presented cases, support that NDH is a distinct entity rather than an acral variant of SS. The most important observation is that many of the reported cases, including the original six described by Strutton et al.,1 showed marked leukocytoclastic vasculitis. This contradicts one of the two major criteria necessary for a diagnosis of SS, namely dense neutrophilic infiltrate without leukocytoclastic vasculitis.4 Several other authors5 have opposed this conclusion, claiming that a secondary leukocytoclastic vasculitis might occur in NDH, and therefore it does not suffice to exclude NDH from the criteria of SS. In addition, cases of NDH usually present with pustular plaques, haemorrhagic bullae, and/or ulcerating lesions, which are uncommon clinical presentations in SS.5 Our observation was also remarkable through unilateral presentation, which is rarely encountered.6 The main difference between NDH and SS is the location of lesions, with a remarkable acral distribution in NDH. We also believe that the term NDH is misleading, as it gives the false impression that the disease is confined to the dorsal hands, whereas it also occurs at other sites, such as the palms and soles.
The exact nature of this acute neutrophilic disorder as a variant of SS, pustular vasculitis, an overlap of both these conditions, or a distinct entity remains unclear. This raises questions about the definitive classification of neutrophilic dermatosis and the need for a designation that can include its different clinical and histopathological presentations.







