The differential diagnosis of pigmented macules on sun-damaged facial skin is one of the most challenging procedures in daily dermatological practice. The differential diagnosis involves distinguishing between melanocytic skin neoplasms, such as lentigo maligna (LM) and LM melanoma (LMM), and nonmelanocytic skin neoplasms, including pigmented actinic keratosis (PAK), solar lentigo (SL), and lichen planus-like keratosis. A correct differential diagnosis between melanocytic and nonmelanocytic lesions is important to ensure the patient receives the appropriate therapy.
Dermoscopy is a noninvasive technique used in routine diagnostic procedures of pigmented lesions. LM, an in situ facial melanoma, has very different dermoscopic features to LMM and shares unspecific dermoscopic criteria with flat nonmelanocytic skin neoplasms. In differentiating between SL and LM, noting the overall colour of the lesion can help in the correct diagnosis: SL is brown-black on dermoscopy whereas LM is characterised by a blue-grey colour.1
LM also shares many features with PAK, including an asymmetric hyperpigmented rim around the follicles and peripheral grey dots and rhomboidal structures. The peripheral grey dots and rhomboidal structures have been found to vary according to colour: on dermoscopy, PAK is lighter in colour compared to LM.1 These guidelines can be helpful in the differential diagnosis of pigmented macules of the face, but a differential diagnosis between PAK and LM remains difficult due to the presence of many common patterns.1
Recently, an important dermoscopic scoring scheme was described that can aid in the differential diagnosis between PAK and early LM.2 This novel procedure may improve the early detection of LM, while reducing unnecessary biopsies for PAK.2 In this instance, white and evident follicles, scales, and a red colour represent significant diagnostic clues for PAK, while intense pigmentation and grey rhomboidal lines are highly suggestive of LM (Figure 1).2
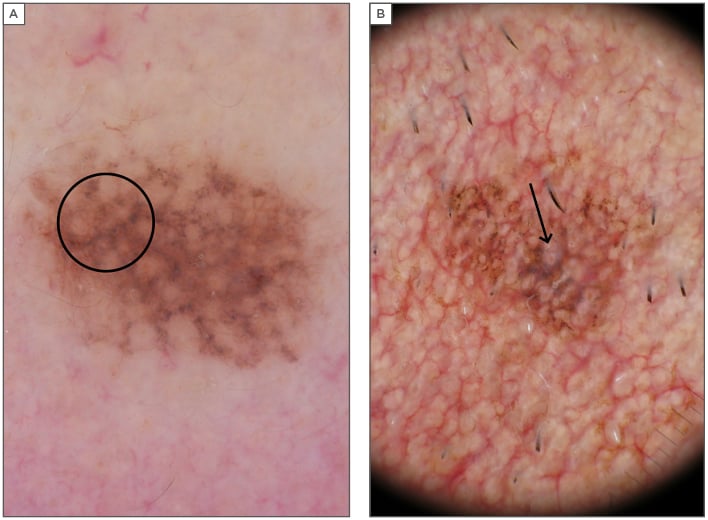
Figure 1: A) Dermoscopic image of lentigo maligna showing the presence of grey rhomboidal lines around follicles (black circle). B) Dermoscopic image of pigmented actinic keratosis showing the presence of white and evident follicles with a white border (black arrow).
Distinguishing LM and PAK, however, still remains challenging in some cases. Reflectance confocal microscopy may help diagnose difficult cases when the normal dermoscopic criteria are not suitable for making a correct diagnosis. For example, many confocal laser microscopy patterns have been found that correlate with the diagnosis of LM. One such pattern is the presence of dendritic cells around the follicles, with the disposition ‘bulging’ inside the follicular opening and a characteristic arrangement around the follicles’ ‘medusa-like structures’ that is typical of the dermal– epidermal junction.3,4







