BACKGROUND AND AIMS
Onychomatricoma is an infrequent, benign fibroepithelial tumour originating from the nail matrix. While the exact cause of onychomatricoma remains uncertain, the tumour has been associated with trauma and onychomycosis. The thumb, particularly on the dominant hand, is commonly affected.1 A single, painless subungual mass in an adult patient who also has onychodystrophy, splinter haemorrhages, and a yellowed nail is the typical clinical presentation.2 Characteristic MRI findings include the nail plate’s proximal section having a Y-shape, along with transverse perforations.3 The following dermatoscopic aspects are encountered: multiple cavities, parallel white lines, parallel lesion edges, splinter haemorrhages, dark dots, nail pitting, and thickening of the free edge. The ultrasonographic appearance is of a hypoechoic tumour that affects the nail matrix, with hyperechoic areas corresponding to the finger-like projections.4
Histopathological examination reveals a biphasic growth pattern. The superficial tumour appearance is of multiple digitised projections, with a fibrous core and a thin epithelial covering. The base of the tumour is composed of epithelium with ‘V-shaped’ keratinous zones, similar to the normal nail matrix. The standard recommendation for treatment and recurrence prevention is complete excision, which includes the normal nail matrix close to the lesion.5
This report aims to describe the clinical, dermatoscopic, and sonographic features of a case involving onychomatricoma.
MATERIALS AND METHODS
The authors present the case of a 58-year-old male who presented with a 2-year history of gradual nail dystrophy, and painless symptoms on his right index finger. Initially misdiagnosed as a wart, the patient had received cryotherapy treatment without improvement. Physical examination revealed asymmetrical, longitudinal, thick yellow bands, and over-curvature of the nail plate in the right index finger. There was no history of nail trauma or personal/family history of skin cancer or dermatological disorders. The nail was assessed using dermatoscopy and skin ultrasound.
RESULTS
Dermoscopy revealed perforations in the distal portion of the nail plate, along with white longitudinal grooves. Ultrasound imaging (longitudinal view) demonstrated a hypoechogenic tumour affecting the nail matrix, finger-like projections represented by hyperechogenic areas, and reduced blood flow (Figure 1).
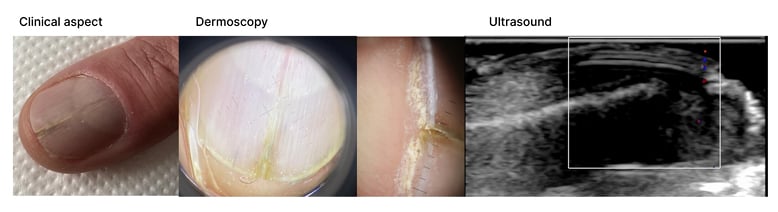
Figure 1: Clinical, dermoscopic, and ultrasound findings.
CONCLUSION
The diagnosis of onychomatricoma is frequently delayed, as patients often delay seeking medical attention due to the tumour’s slow growth, and lack of pain in most cases.6
Moreover, the unfamiliarity of dermatologists with the clinical features of onychomatricoma contributes to under-recognition of this uncommon nail matrix tumour. Therefore, this report presents a typical case of onychomatricoma, to aid dermatologists in recognising its clinical features, and promoting early detection of this rare condition.






