Meeting Summary
This CSL Behring-supported symposium took place during the European Society of Cardiology (ESC) 2021 Congress. Experts P. Gabriel Steg Cardiology Department, Hôpital Bichat-Claude-Bernard, Paris, France, and the Université de Paris, France; and Kausik Ray, Imperial Centre for Cardiovascular Disease Prevention, Imperial College London, UK; Imperial Clinical Trials Unit, Imperial College London, UK; and Commercial Trials, Imperial College London, UK, discussed the clinical significance of the early post-acute myocardial infarction
(AMI) period and the risk of recurrent events despite optimal recommended standard of care.
Steg highlighted data from a retrospective registry study as well as several randomised controlled trials, suggesting that recurrent cardiovascular (CV) events appeared to accrue quickly in the early post-AMI period. He proposed that this may be an important timeframe for additional therapeutic interventions and warrants further investigation.
Ray highlighted guideline recommendations for secondary prevention, currently focused on lipid-lowering and antiplatelet therapies. Ray presented data from several randomised controlled trials of lipid-lowering therapies, demonstrating that despite therapeutic advances and guideline-recommended treatments, there is a residual risk of recurrent CV events post-AMI. Ray suggested that additional therapeutic targets should be explored to further reduce the incidence of recurrent CV events post-AMI.
Significance of the 90-Day High-Risk Post-Acute Myocardial Infarction Period
P. Gabriel Steg
Steg opened the symposium by calling attention to the ongoing global healthcare issue posed by cardiovascular disease (CVD). He noted that, despite therapeutic advances, atherosclerotic CVD is still the number one cause of death worldwide, and more than 4 million Europeans die from CVD each year.1 Most atherosclerotic CVD-related deaths are preventable, with around one-quarter of all AMIs being recurrent.2-4 Steg highlighted data from a study by Norgaard et al.,5 which assessed all-cause mortality, CV mortality, and AMI in over 3 million Danish residents aged ≥30 years. The data demonstrated that there is an elevated risk of a recurrent event in individuals who survive AMI, particularly in the short term. In the first year following an AMI, the relative risk (RR) of a recurrent event is increased 20- to 43-fold (21.7 [95% confidence interval (CI): 21.1–22.4] in males and 43.3 [95% CI: 41.8–44.9] in females) and remains elevated in the longer term (RR 1–3 years: 2.99 [95% CI: 2.80–3.18] in males and 5.67 [95% CI: 5.25–6.11] in females; RR 3–5 years: 2.67 [95% CI: 2.48–2.87] in males and 4.33 [95% CI: 3.93–4.78] in females).5 It is estimated that life expectancy is approximately halved in patients who experience an AMI compared with the general population.6
Steg discussed data from the HELICON study, a retrospective cohort analysis of Swedish national registries, in which risk of CVD was investigated in patients post-AMI. The primary composite endpoint of non-fatal AMI, non-fatal stroke, or CV death was assessed in patients with a primary diagnosis of AMI, who were alive one week after discharge (N=97,254).The cumulative rate of the primary composite endpoint was 13.3% and 18.3% during the first 6 and 12 months, respectively.7 During his presentation, Steg drew attention to the shape of the composite events curve, highlighting the rapid accrual of events in the immediate 90-day post-AMI period.
Steg noted that a similar trend is also observed in data from several randomised controlled trials. In the TRITON–TIMI 38,8 PLATO,9 ATLAS ACS 2-TIMI 51,10 and MIRACL11 trials, CV outcomes were investigated in patients post-acute coronary syndrome (ACS) or post-AMI, who were treated with various interventions (Table 1). Steg suggested that, across all four trials, CV events appeared to accrue quickly in both treatment arms in the early post-ACS/post-AMI period and became more stable in the long term.
More recently, a similar trend was observed in the BETonMACE study of 2,425 patients post-ACS (7–90 days) with diabetes and low levels of high-density lipoprotein cholesterol (Table 1).12 Although the primary endpoint was not reached in the BETonMACE study, Steg suggested that for patients receiving either placebo or apabetalone, the highest risk of non-fatal AMI, non-fatal stroke, or CV death (primary outcomes) is during the early post-ACS period.
The PARADISE-MI trial was another large, randomised study that enrolled patients (N=5,669) post-AMI (0.5–7.0 days; Table 1).13,14 Patients had either left ventricular ejection fraction ≤40% and/or pulmonary congestion, plus additional risk factors such as age ≥70 years, diabetes, or atrial fibrillation. Steg noted that, similar to the BETonMACE and PARADISE-MI studies, the cumulative incidence of the primary outcome of CV death, heart failure, hospitalisation, or outpatient heart failure increased early before becoming almost linear thereafter in both treatment arms.
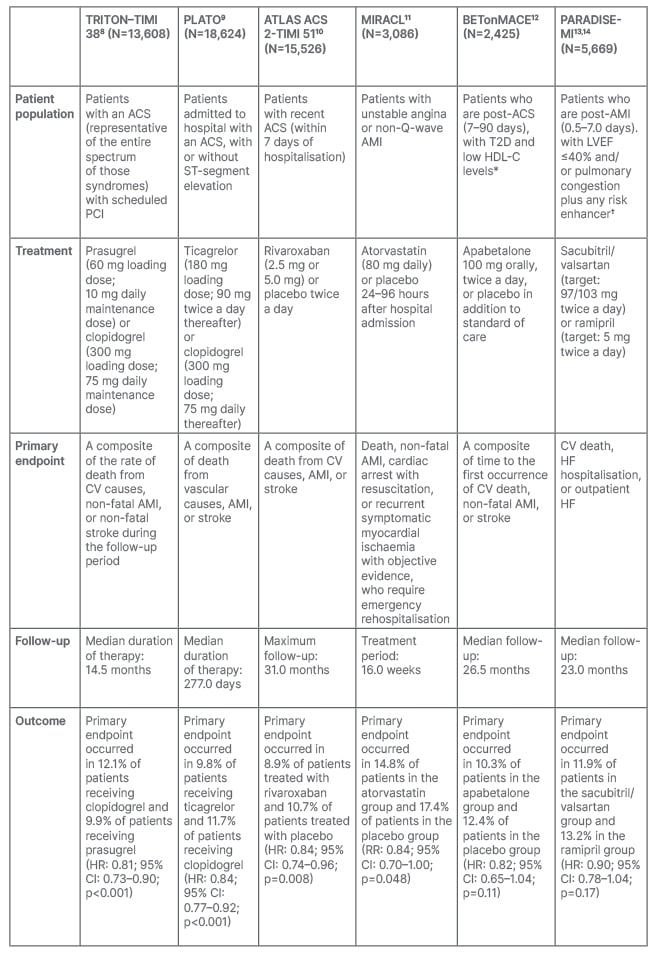
Table 1: Patient population, treatment, and primary endpoint outcomes across various trials in patients who are post-acute coronary syndrome and post-acute myocardial infarction.
This table is intended as a summary only and should not be used to compare trials.
*Males <40 mg/dL; females <45 mg/dL.
†≥70 years, eGFR <60 mL/min/1.73 m2, diabetes, prior AMI, atrial fibrillation, LVEF <30%, Killip class ≥III, and STEMI without reperfusion.
ACS: acute coronary syndrome; AMI: acute myocardial infarction; CI: confidence interval; CV: cardiovascular; eGFR: estimated glomerular filtration rate; HDL-C: high-density lipoprotein cholesterol; HF: heart failure; HR: hazard ratio; LVEF: left ventricular ejection fraction; PCI: percutaneous coronary intervention; RR: relative risk; STEMI: ST-segment elevation myocardial infarction; T2D: Type 2 diabetes.
Steg concluded that the early 90-day post-AMI period may be an important timeframe for additional therapeutic interventions. Currently, it remains to be shown whether this period of early risk can be modified to address the continuing risk of recurrent CV events in patients who have experienced AMI.
Risk of Recurrent Cardiovascular Events with the Current Standard of Care
Kausik Ray
Ray began his presentation by outlining the current ESC and the European Atherosclerosis Society (EAS) recommendations for the secondary prevention of recurrent CV events, which include a combination of lifestyle and pharmacological interventions.15 Reflecting on these guidelines, Ray suggested that, despite the recommended clinical standard of care, there is still an ongoing risk of recurrent CV events in patients post-AMI. Low-density lipoprotein cholesterol (LDL-C) is the primary focus of lipid-modification treatments and therapies include statins, ezetimibe, and the proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitor. Icosapent ethyl may also be considered in patients with high triglyceride (TG) levels (135–499 mg/dL), in addition to statin treatment.15
Ray highlighted data from several randomised controlled trials with LDL-lowering or TG-lowering therapies.16-19 He suggested that even intensive lipid-lowering therapies do not abolish the risk of a recurrent CV event post-ACS or an initial event in patients with established CVD or diabetes (Table 2). In the PROVE IT–TIMI 22 study, patients (N=4,162) were randomised to daily high-dose atorvastatin (80 mg) or low-/moderate-dose pravastatin (40 mg). There was a 16% reduced risk of death in patients treated with high-dose atorvastatin compared with low-/moderate-dose pravastatin (95% CI: 5–26%; p=0.005).16 In the IMPROVE-IT trial, patients hospitalised for an ACS (N=18,144) received either simvastatin plus ezetimibe (40 mg/10 mg) or simvastatin (40 mg) plus placebo daily. Similar to PROVE IT–TIMI 22, intensive lipid-lowering treatment with simvastatin plus ezetimibe was effective in reducing CV events compared with simvastatin monotherapy (hazard ratio [HR]: 0.94; 95% CI: 0.89–0.99; p=0.016).17 Ray commented that, in light of the positive primary endpoint outcomes in these studies, a high risk of recurrent events remains in both the interventional and control arms, particularly in the early post-ACS period.
Ray also highlighted a similar trend in studies with PCSK9-inhibitor and TG-lowering therapies (Table 2). In the ODYSSEY OUTCOMES trial, patients with an ACS and LDL-C level ≥70 mg/dL, who were already receiving high-intensity statin therapy (N=18,924), were randomised to receive alirocumab (75 mg) or placebo every 2 weeks.18 There was a 15% reduction in risk of death from CV-related causes in patients treated with alirocumab compared with placebo (HR: 0.85; 95% CI: 0.78–0.93; p<0.001); however, even with a marked reduction in LDL-C, Ray suggested that the early risk of a recurrent CV event post-ACS is not completely eliminated.
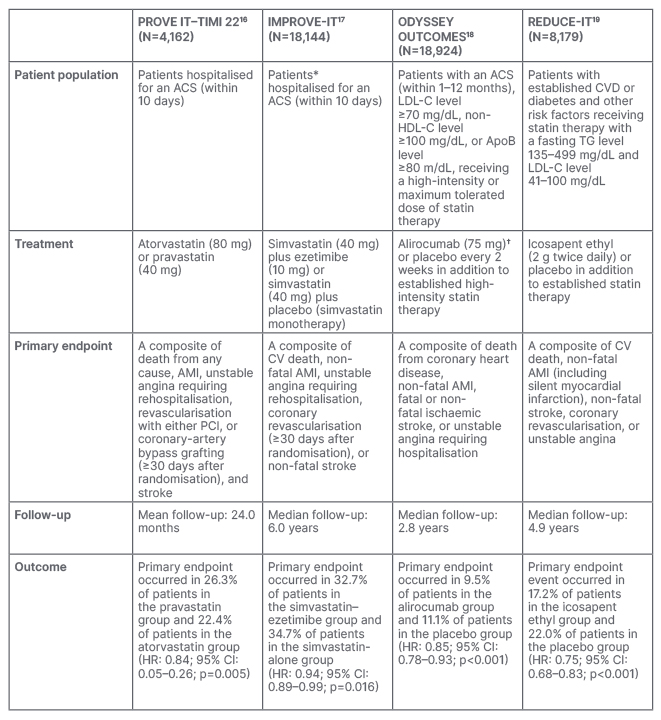
Table 2: Patient population, treatment, and primary endpoint outcomes across trials in patients post-acute coronary syndrome or with stable cardiovascular disease treated with intensive low-density lipid-lowering or triglyceride-lowering therapies.
*Patients with LDL-C levels 50–100 mg/dL on lipid-lowering therapy or 50–125 mg/dL without lipid-lowering therapy.
†Dose was adjusted to target an LDL-C level of 25–50 mg/dL.
ACS: acute coronary syndrome; AMI: acute myocardial infarction; ApoB, apolipoprotein B; CI: confidence interval; CV: cardiovascular; CVD: cardiovascular disease; HDL-C: high-density lipoprotein cholesterol; HR: hazard ratio; LDL-C: low-density lipoprotein cholesterol; PCI: percutaneous coronary intervention; TG: triglyceride.
In the REDUCE-IT trial, patients (N=8,179) with established CVD or at high-risk of a first CV event, who had elevated TG levels and were established on statin therapy, received either icosapent ethyl or placebo. In patients with elevated TG and controlled LDL-C levels, there was a 25% reduction in the risk of CV events when treated with icosapent ethyl compared with placebo (HR: 0.75; 95% CI: 0.68–0.83; p<0.001).19 However, over a 5-year period, approximately one-quarter of all patients in the icosapent ethyl group experienced a recurrent CV event.20 Ray suggested that, even with the risk reduction achieved by PCSK9 inhibitors or TG-lowering therapies, the risk of a recurrent CV event remains and alternative molecular pathways need to be explored to identify additional preventative treatments.
Consistent with observations from lipid-lowering studies, Ray presented data from the COMPLETE trial that suggest that the risk of recurrent AMI remains despite advances in surgical interventions. In the COMPLETE trial, patients with ST-segment elevation myocardial infarction and multivessel coronary artery disease (N=4,041) were randomised to receive complete revascularisation with percutaneous coronary intervention or no further revascularisation. The data demonstrated that a complete revascularisation approach (including non-culprit lesions) reduced the primary endpoint composite of CV death and recurrent AMI by 26% compared with culprit lesion percutaneous coronary intervention alone (HR: 0.74; 95% CI: 0.60–0.91; p=0.004).21 The benefit from complete revascularisation was doubled (8.9% versus 16.7% for revascularisation versus non-revascularisation, respectively) when the endpoint also included ischaemia (HR: 0.51; 95% CI: 0.43–0.61; p<0.001).21 However, Ray highlighted that, despite complete revascularisation and evidence-based treatment, the results showed that there was still a clinically relevant risk of recurrent events, suggesting that there is an unmet need in the post-ACS period.
Ray highlighted that there are multiple pathways contributing to the risk of recurrent events in patients post-AMI, affirming the need for a multifactorial approach to treatment. Beyond lifestyle interventions and the guideline-recommended standard of care, there are a number of potential early-risk targets, including coagulation, platelets, metabolism, inflammation, and lipoproteins.22
To conclude the symposium, Ray reiterated that, despite therapeutic advances in the recommended standard of care, data from multiple randomised controlled trials have demonstrated that recurrent CV events are still observed in some patients post-AMI and additional therapeutic targets should be explored to further reduce the incidence of recurrent CV events in the future.








