Abstract
Hidradenitis suppurativa (HS) is a chronic inflammatory disease believed to be a risk factor for cardiovascular events. Traditional cardiovascular risk factors, such as metabolic syndrome, often coexist with HS. Chronic inflammatory conditions may underlie cardiovascular events in young patients or those with few traditional risk factors. A 34-year-old female was admitted to the authors’ tertiary care hospital with acute anterior ST-segment elevation myocardial infarction, and underwent a successful primary percutaneous coronary intervention to their left anterior descending artery. They were a smoker, had a high BMI, and had a positive family history of premature coronary artery disease. During their admission, the patient disclosed that they had discharging lesions under their left breast. The patient had a long-standing history of multiple discharging lesions alternating with disfiguring scars that had started in their late childhood; however, despite this leading to self-dissatisfaction, they did not seek medical advice.
Examination revealed plaques and scarring in both axillae and a chronic abscess under the left breast, the swabs from which were sterile, as is consistent with HS. The laboratory results showed a raised troponin and white cell count with mildly elevated levels of C-reactive protein. The patient was managed with standard acute coronary syndrome treatment and a course of oral doxycycline, and awaits further treatment by dermatology and plastic surgery. The morbidity of HS is grossly underestimated. This case study highlights that HS has significant cardiovascular implications, in addition to psychological impacts, and that underlying systemic inflammation may promote rapid atherosclerosis. Further research into pathogenesis and strategies to prevent adverse cardiovascular events are needed.
INTRODUCTION
Hidradenitis suppurativa (HS) is a chronic inflammatory disease involving the pilosebaceous unit of the skin. It is characterised by abscesses, the development of sinus tracts, and scarring, and primarily affects the axillary, perineal, and inframammary regions.1 The reported prevalence of HS varies from 0.03% to 4.00%, depending on geographical location.2 HS disproportionately affects young female African Americans and male Asians.2
Coronary artery disease is the leading cause of death worldwide. Myocardial infarction still has a 20% mortality rate, and together with stroke contributes a significant morbidity and health cost burden.3 Risk factor reduction has led to a reduction in the incidence of adverse cardiovascular events and associated mortality over the past 25 years.3 Recognising the interaction of traditional risk factors with systemic inflammation in the pathogenesis of atherosclerosis is important. Cardiovascular risk factors, including obesity, metabolic syndrome, diabetes, and smoking, are prevalent in patients with HS.1,4,5 The odds ratio of patients with HS having metabolic syndrome and central obesity is approximately 2.4,5 Obesity causes intertriginous surface friction and increased sweat production, which are also associated with HS.6 It is believed that nicotine may also cause increased follicular plugging; however, HS may start long before smoking.6 Insulin resistance, relative androgen excess, and excess inflammatory markers are linked with both metabolic syndrome and HS.6,7
CASE PRESENTATION
A 34-year-old Black female of African descent presented to the emergency department after experiencing severe central chest pain with sweating and nausea for 2 hours. They had risk factors such as smoking, obesity, and a positive family history of premature ischaemic heart disease. There was also history of temporal lobe epilepsy controlled on anti-epileptics. An ECG showed ST-segment elevation in anterolateral chest leads and inferior limb leads (Figure 1). The patient was taken to the catheterisation lab with the intent of performing primary percutaneous coronary intervention. An emergency coronary angiogram showed a 99% occlusive thrombotic lesion in the mid-left anterior descending artery, with thrombolysis in myocardial infarction (TIMI) Grade II flow and minor plaque in right coronary artery (Figure 2). Coronary angioplasty was performed with successful restoration of TIMI Grade III epicardial flow and good myocardial blush, and ST-segment resolution was achieved.
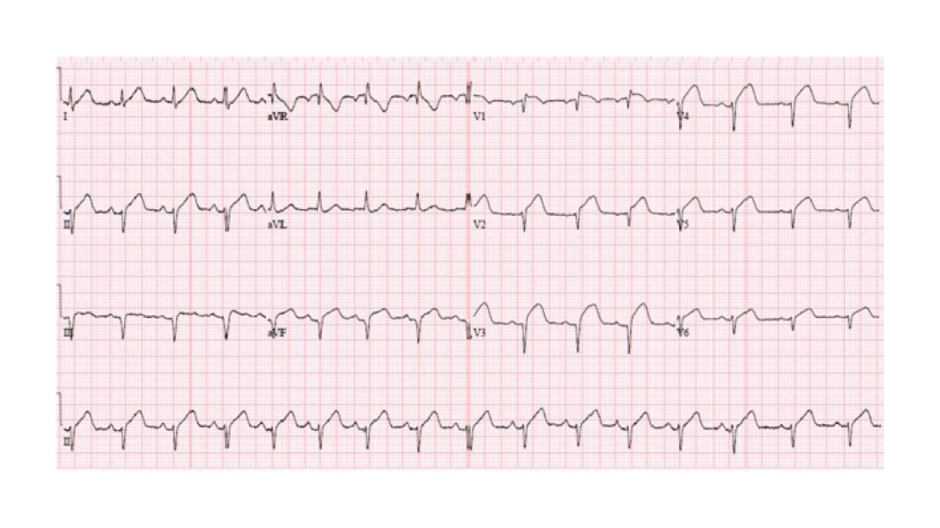
Figure 1: An ECG presentation showing ST-segment elevation in anterolateral and inferior leads.
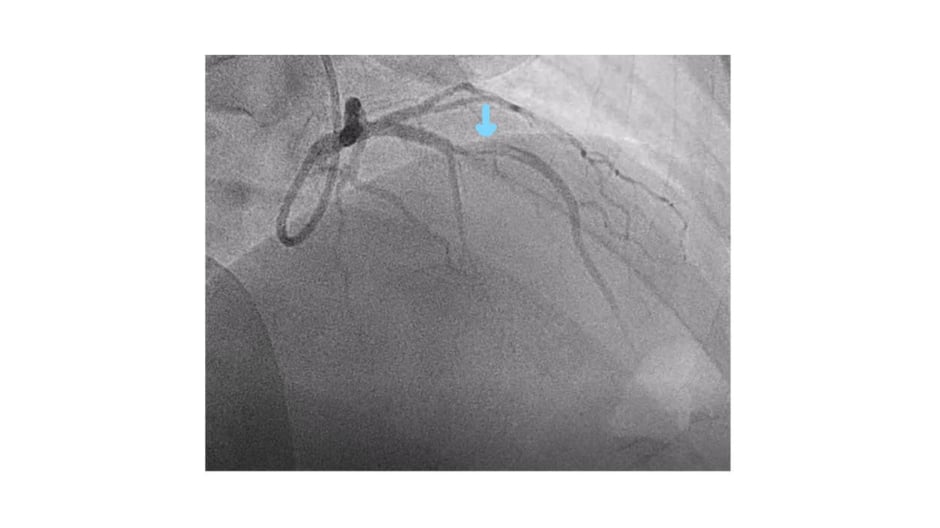
Figure 2: An angiogram from the right anterior oblique cranial projection showing a thrombotic occlusion
On return to the coronary care unit, they complained of pain under their left breast, and examination revealed a discharging lesion there. On further inquiry, they declared similar lesions in both axillae for several months. They had a long history of discharging lesions beginning in their childhood, initially involving their buttocks and later their armpits, which healed with unsightly scars. The location of the lesions kept her from seeking medical attention, despite causing emotional distress and self-dissatisfaction. On examination, there was a discharging abscess under the left breast and a partially healed sub-centimetric pustule under the right breast (Figure 3). Additionally, there were scars, plaques, and sinus formation under the armpits (Figure 3). There were no signs of systemic infection, drug abuse, or diffuse skin or mucosal involvement. Swabs taken from the draining pustule did not show any bacterial growth. The opinion of dermatologists was then taken and the patient was formally diagnosed with Stage II HS.
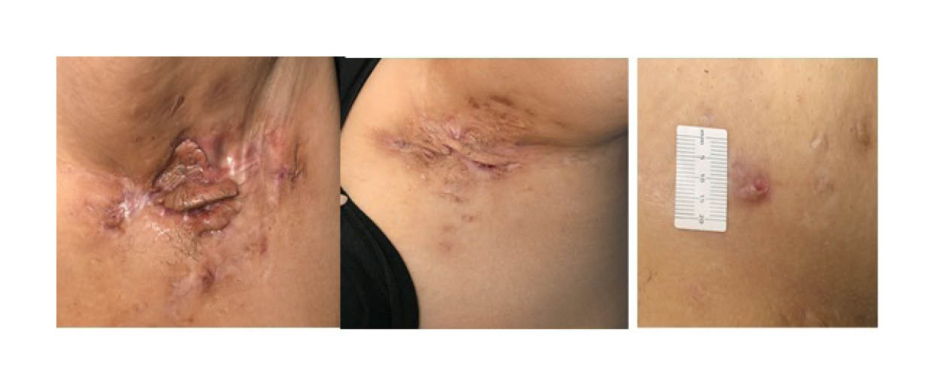
Figure 3: Chronic abscesses with tract formation and scarring lesions in both axillae
A transthoracic echocardiogram revealed moderate left ventricular systolic impairment with regional wall motion abnormalities in the left anterior descending artery territory. The laboratory results showed a raised troponin level (9,196 ng/L), a raised white cell count of 18×109 /L with neutrophilia, an elevated platelet count of 817×109 /L, and an elevated high-sensitivity C-reactive protein level of 15 mg/L (normal range: 0–4 mg/L). The neutrophil-to-lymphocyte ratio was 3.9, the neutrophil-to-high-density lipoprotein (HDL) cholesterol ratio was 15.6, and the platelet-to-lymphocyte ratio was 227, all of which were suggestive of inflammation. The lipid profile was abnormal, with total cholesterol of 5.5 mmol/L, non-HDL cholesterol of 4.6 mmol/L, and HDL cholesterol of 0.9 mmol/L. The patient fulfilled the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) criteria for metabolic syndrome. They were managed using guideline-directed treatment, counselled for smoking cessation and weight loss, and provided with psychological support and cardiac rehabilitation. A course of oral doxycycline was prescribed by dermatologists and a follow-up was planned for the consideration of more advanced medication as needed. They were referred to plastic surgeons for possible future excision and reconstruction once active inflammation had subsided.
DISCUSSION
HS is associated with an increased risk of major adverse cardiovascular events (MACE) and related mortality.1,4 There is a 23% increase in risk of myocardial infarction or stroke in patients with HS, which is independent and incremental of the risk from traditional cardiovascular risk factors.1 The MACE risk is higher in younger patients with HS, andHS has also been shown to impose a higher cardiovascular risk compared with severe psoriasis.1,4
The inflammatory basis of HS is evidenced by the presence of inflammatory cytokines in the lesions.6 Chronic skin inflammation in HS may be associated with systemic inflammation, as shown by elevated C-reactive protein, reactive thrombocytosis, and an increased neutrophil-to-lymphocyte ratio.1 These inflammatory markers are related to the severity and activity of HS.6 The accompanied vascular inflammation predisposes the body to oxidative stress, endothelial dysfunction, and thrombus formation, thus promoting the chronic progression of atherosclerosis and acute plaque change.1,7 The most common cause of ST-segment elevation myocardial infarction is plaque rupture, and the pro-inflammatory states also increase the vulnerability of plaque to rupture.1,8 Elevated levels of circulating inflammatory markers are associated with atherosclerosis.1,8,9 Other inflammatory skin or systemic diseases have been independently associated with cardiovascular adverse events. As a result, inflammation appears to be paramount to the pathogenesis of HS and associated cardiovascular events. Emerging treatments targeting specific inflammatory mediators may therefore be important.8
The cardiovascular consequences of HS warrant taking specific steps in order to mitigate these events. Firstly, patients with HS should be informed of their increased risk of MACE, screened at an earlier stage for cardiovascular risk factors, and counselled for risk factor modification, including smoking cessation and weight loss. Secondly, a low threshold should be kept for investigating young patients with HS presenting with cardiac symptoms. Thirdly, many patients with HS suffer as a result of a considerable diagnostic delay, and increased awareness about the morbidity of HS may promote an earlier approach of patients to healthcare and an increased vigilance for diagnosis.







