Interviewees: Vallerie McLaughlin,1 Sean Gaine2
1. Division of Cardiovascular Medicine, University of Michigan, Ann Arbor, Michigan, USA
2. National Pulmonary Hypertension Unit, The Mater Hospital, Dublin, Republic of Ireland
Disclosure: Dr McLaughlin has received research support/grants from Acceleron Pharma, Inc., Actelion Pharmaceuticals US, Inc., Reata Pharmaceuticals, Inc., Sonvie, and United Therapeutics; and served as a consultant for Acceleron Pharma, Inc., Actelion, Bayer, Caremark, and United Therapeutics Corporation. Prof Gaine has received honoraria for advisory board and drug safety board work; and has been a speaker for many companies involved in pulmonary hypertension including Actelion, Bayer and United Therapeutics.
Support: The publication of this article was funded by Actelion Pharmaceuticals Ltd., a Janssen Pharmaceutical Company of Johnson & Johnson. The opinions expressed in this article belong solely to the named interviewees.
Acknowledgements: Medical writing assistance was provided by Kara McNair, KMG Medical Communications, Glasgow, UK.
Interview Summary
EMJ conducted interviews with Dr Vallerie McLaughlin and Prof Sean Gaine, world experts in cardiology and respiratory medicine, respectively. Dr McLaughlin and Prof Gaine are two members of the 19 pulmonary arterial hypertension (PAH) specialists who were part of the Prostacyclin International Expert Panel (PIXEL), involved in the construction and publication of an expert consensus survey on the treatment of PAH with oral prostacyclin pathway agents (PPA). They shared with us their personal clinical experience in treating patients with PAH with oral PPA and provided an insight into the impact they hope this publication may have on the treatment of patients with PAH.
BACKGROUND
PAH is a rare, progressive disorder with a number of aetiologies. Approximately 15–60 patients per million of the global population are affected, impacting significantly on patients’ physical, psychological, and emotional wellbeing. The median survival is only 6 years, despite an increase in treatment options over the past 25 years.1-3 The World Health Organization (WHO) has assigned four functional classes (FC[I–IV]) to define the severity of a patient’s symptoms, with FCIV symptoms being the most severe.4
In PAH, proliferation of each layer of the wall of the small pulmonary arterioles results in a narrowing of the arteries and increased resistance to pulmonary blood flow. This increased resistance augments right ventricular (RV) workload, which can result in heart failure and, ultimately, death. However, there have been significant advances in elucidating the pathophysiology of PAH, improving patients’ prognosis in both the short term (i.e., improved exercise tolerance) and long term (delayed disease progression). Indeed, survival rates have increased in recent years.5 An imbalance of vasoactive mediators, including endothelin and nitric oxide, is key to the development and progression of the disease; hence, the standard of care for adult patients with PAH and FCII or FCIII symptoms is initial double upfront therapy with an endothelin receptor antagonist (ERA) and a phosphodiesterase-5 inhibitor (PDE5i). However, it is also known that the prostacyclin pathway plays a pivotal role in the pathogenesis of PAH. The first PPA approved for use by the U.S. Food and Drug Administration (FDA), epoprostenol, was highly effective, but required intravenous (IV) administration, which is often associated with adverse events including catheter infections, diarrhoea, and headaches.6 However, recent years have seen the emergence of novel oral and inhaled PPA, increasingly popular because of their efficacy, route of administration, and potentially favourable side-effect profile.
Alongside initial upfront combination therapy, comprehensive risk assessment is also critical for optimal individualised treatment. Indeed, the 2015 European Society of Cardiology (ESC)/European Respiratory Society (ERS) guidelines recommend frequent, regular assessment of a patient’s risk of disease progression or death. This risk assessment has become an essential component of PAH disease management. Patients are classified as being at low- (<5%), intermediate- (5–10%), or high- (>10%) risk of 1-year mortality, depending on a composite of variables including clinical and functional assessments, exercise tolerance, biochemical markers, and imaging and haemodynamic parameters.7 The ultimate goal for clinicians is to achieve or maintain a ‘low-risk’ status, as individuals at low risk demonstrate improved long-term outcomes.
Guidelines on the use of oral PPA in the treatment of PAH have been associated with a degree of uncertainty. Currently, administration of ERA and PDE5i in adult patients with FCII and FCIII symptoms is recommended as double upfront therapy. However, in patients with an intermediate risk status, ESC/ERS guidelines and the 6th World Symposium on Pulmonary Hypertension (WSPH) proceedings advise escalation to triple therapy by the addition of an oral or parenteral PPA.7, 8 The American College of Chest Physicians (CHEST) guidelines differ, however, in that they found no evidence to support the use of the oral PPA treprostinil, and gave no recommendation on when to introduce the oral PPA selexipag, resulting in ambiguity for prescribing physicians.9 In order to address this ambiguity, 19 expert clinicians from around the world took part in an expert consensus survey, with the intention of developing consensus opinions on the clinical scenarios to be considered when initiating oral PPA therapy.10 Two of these expert clinicians, lead author Dr McLaughlin and Prof Gaine, discussed their role in the publication of the PIXEL consensus statements, and their own ‘real-world’ experience of oral PPA use in the treatment of PAH.
THE PIXEL CONSENSUS: RATIONALE
As a physician with almost 25 years’ experience, Dr McLaughlin embarked on her career the year the first IV PPA, epoprostenol, was approved for use in patients with PAH. With limited treatment options at the time, decisions were easier to make. “PAH was actually quite easy to treat: no discussion, no choices to be made as there was only one option,” said Dr McLaughlin. Today, physicians are armed with more treatment options, including oral PPA. However, as Dr McLaughlin explained: “The most recent CHEST guidelines make no recommendation on what to do with these oral PPA, so you have these therapies on the market and you have a guideline not giving any recommendations.”
So, what impact does this have on patient care? “In some countries, such as the USA where insurance companies may look at CHEST guidelines, patients might be denied an oral PPA when it could be very useful for that patient,” explained Dr McLaughlin. Furthermore, according to Prof Gaine: “Many physicians stick very strictly to guidelines, and if you don’t properly risk-stratify a patient, they may remain on inadequate treatment for too long. Furthermore, if a physician equates oral prostacyclin agonist therapy to IV therapy, then they will put patients at risk.”
Discussing the PIXEL process itself, Prof Gaine explained one of the key drivers in its development: “Communicating that, just because therapies were of the same class, where you position them in treatment was one of the most important things.” The RAND-UCLA process was used to develop the PIXEL consensus statements in two groups of patients: idiopathic, heritable, repaired congenital heart defect, and drug- or toxin-induced PAH (IPAH+) or connective tissue disease-associated PAH (CTD-PAH). Findings from five randomised oral PPA (treprostinil and selexipag) studies were considered,11-14 in addition to the experts’ clinical experience in a broader patient population than that defined by the strict inclusion and exclusion criteria of clinical trials.
The PIXEL process was based on aspects of patient care that were deemed most important to the experts. Whilst most clinicians employ a multiparameter approach when risk stratifying patients, RV function became an important area of discussion. “You can measure many things, but if you have a right ventricle that is very dysfunctional, then alarm bells should be ringing despite other parameters looking OK,” explained Prof Gaine. Discussing PAH-induced hospitalisations, Prof Gaine added: “We agreed that hospitalisation added to our decision making, even though it was not yet on the risk algorithm in Europe. For example, if everything looks okay when a patient is reviewed in the clinic but [the patient has] had recent and frequent hospitalisations, the experts took a far grimmer view about that patient’s prognosis.” Prof Gaine pointed out that the weight the experts placed on these two parameters, RV function and hospitalisations, might not necessarily stand out to the clinician solely looking at the guidelines and the risk profile of that individual.
During the process, the panel agreed that there was a lack of evidence in PAH for the use of oral treprostinil in addition to double combination therapy with ERA and PDE5i. As a result, the 14 consensus statements to emerge from the PIXEL publication related solely to the use of selexipag in patients with PAH. Dr McLaughlin pointed out that such an outcome would perhaps be different following the subsequent publication of the data from the FREEDOM-EV clinical trial.15
THE PIXEL CONSENSUS: RECOMMENDATIONS
A diverse group of 13 patient subtypes with IPAH+ or CTD-PAH were identified as appropriate candidates for the use of oral selexipag by the expert panel (Table 1). Discussing these 13 clinical scenarios, Dr McLaughlin explained: “This paper helps exemplify which patients are appropriate for oral PPA based on risk assessment, and I think it goes into some granular detail of even patients at lower risk that might be appropriate candidates for oral PPA.”
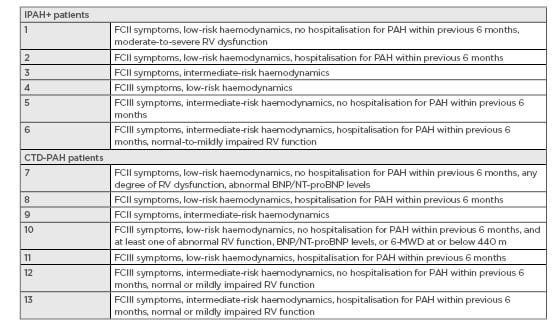
Table 1: Patient subtypes considered appropriate for oral selexipag use.
BNP: B-type natriuretic peptide; CTD-PAH: connective tissue disease-associated pulmonary arterial hypertension; FC: functional class; IPAH+: induced pulmonary arterial hypertension; NT-proBNP: N-terminal pro B-type natriuretic peptide; PAH: pulmonary arterial hypertension; RV: right ventricular; 6-MWD: 6-minute walk distance.
“There are a lot of patients who, despite [upfront] dual oral therapy, which I think is very effective and is the standard of care for newly diagnosed patients, still don’t reach other low-risk features and should be treated with more aggressive therapy,” explained Dr McLaughlin, confirming that for many such patients the use of selexipag may be entirely appropriate. Prof Gaine agreed that the idea of earlier treatment was supported by this expert committee. Indeed, he pointed out that it is a small minority of patients, potentially as low as 20%, that reach a low-risk profile following double upfront therapy at 3-month follow-up. Discussing these recently diagnosed patients, Prof Gaine imparted: “You have a chance to decide on how they [patients] have done on double upfront combination and following risk assessment you have the opportunity to decide on whether you think this patient should be on triple therapy.” Furthermore, Prof Gaine stated that it is also not uncommon to have a situation whereby you have a patient who has had the disease for longer and remains on double combination therapy with a degree of stability, but still exhibits FCIII symptoms alongside an intermediate-risk profile. “For those patients I would certainly consider them for oral PPA as it targets the very important third therapeutic pathway, prostacyclin,” explained Prof Gaine. Dr McLaughlin also emphasised the importance of continuously monitoring patients throughout the course of their treatment, because patients in one risk category at any one time may not be of a similar status 6 months later.
Dr McLaughlin describes the risk stratification of clinical scenarios in terms of a decision tree to illustrate the different spectrums of disease severity, with branches to the extreme left and right representing patients for whom treatment with oral PPA is not appropriate. “I think one thing that became very clear is that there are people who are very sick, [in whom] we should not consider using an oral PPA,” explained Dr McLaughlin. “The standard of care should just be going straight to a parenteral prostacyclin.”
Prof Gaine agreed: “If you were seeing somebody who had significant RV dysfunction, FCIII/IV symptoms, and walk distances that were poor then it was asking a lot of an oral agent in that class of drug to rescue that patient’s failing right ventricle.” He added that: “We were nervous that people who are not as experienced in the area might end up by asking too much of selexipag in that setting and then patients would be deprived of IV therapy.” At the other end of the spectrum of disease severity, Dr McLaughlin noted that low-risk profile patients probably do not need oral PPA, with all the associated potential side effects and costs. Both experts, however, emphasised the importance of ongoing risk stratification, not just at baseline, but at subsequent visits: “I think that at every visit we need to risk stratify patients and try to drive them into the low-risk category.”
THE BENEFITS OF USING ORAL PROSTACYCLIN PATHWAY AGENTS: WHO AND WHAT?
The PIXEL publication highlighted 13 patient subtypes, in terms of risk profiles, who might be considered most appropriate for oral PPA therapy, but are these the only patients who could see a benefit? “First of all, we looked at two different PAH groups here, we looked at IPAH+ and we looked at CTD,” explained Dr McLaughlin. She continued: “There may be patients who don’t fall into those categories,” highlighting that there are patients with other comorbidities beyond the realm of what is included in randomised controlled trials. Other possibilities include patients not on double upfront therapy, because of side-effect profiles of either ERA or PDE5i, for example. As a result, patients who would benefit from selexipag are certainly not limited to the 13 patient subtypes detailed in the publication, confirmed Dr McLaughlin. “There may very well be other patients,” Prof Gaine agreed. “We take each patient individually, make decisions based on their risk assessment, and sometimes they don’t fit neatly into defined groups, so we do make decisions sometimes that are unique to that particular patient.”
Concerning what patients and clinicians could expect to see, both experts highlighted long-term outcomes as a key promise of oral PPA treatment. “I would say that we have very important data from the largest clinical trial ever done in PAH, the GRIPHON trial, that demonstrate improvement in long-term outcomes [with selexipag],”16 explained Dr McLaughlin. Such substantial long-term benefits could be more difficult to see in clinical practice, both experts conceded, with the lack of a controlled scientific setting that a clinical trial offers. However, Dr McLaughlin observed: “I certainly would say that patients are living longer these days, that patients continue to do better.” Dr McLaughlin is a “big believer in long-term outcomes,” especially in patients where the overall prognosis is favourable, allowing more aggressive therapy strategies to be employed. Prof Gaine agreed with Dr McLaughlin that long-term benefits can be difficult to look at in the clinic. “You have to go with the data in trials rather than anecdotal clinical experience when it comes to the effect of a therapy on long-term outcome.” He continued to say that patients using oral PPA do not often get the same immediate ‘vasodilator benefit’ often seen when patients are given an ERA or PDE5i, adding that: “They may actually come back and discuss the side effects, rather than their perceived improvement.” He added: “It’s helpful to focus on the long-term benefits a patient will have, based on the data we have from a large clinical trial rather than to focus and look for potentially short-term symptomatic improvements.”
CONCLUSION
When asked if going through the PIXEL process made her reconsider her own practice, Dr McLaughlin replied: “In general, these statements are the way that I practise,” adding, “I think I’m pretty aggressive with therapy.” Prof Gaine added: “It was interesting to see the [findings from a] big outcomes trial like GRIPHON translating into experts [on the PIXEL panel] deciding to take things like hospitalisation into consideration in a way they wouldn’t have before. I too will be including it more prominently in the way I assess patients in future.”
Dr McLaughlin agrees that the PIXEL data helped set a framework for determining which patients could potentially benefit from additional therapy with an oral PPA, adding: “I would say that we have very important data from the largest clinical trial ever done in PAH, the GRIPHON trial, that demonstrate improvement in long-term outcomes.” She continued: “I also think at this point we’re thinking not just about short-term outcomes such as improving symptoms, we’re thinking about long-term outcomes in improving morbidity and mortality in these patients.”
So, what could your PAH colleagues expect to see if they were to start using oral PPA to treat patients with PAH? Dr McLaughlin answered: “I think there are some shorter-term symptomatic improvements that may be seen in some patients, but the whole goal of the GRIPHON study was to assess longer-term outcomes. I think that’s really what we can most solidly say about this therapy, and that’s what they could expect to see.”
This was corroborated by Prof Gaine: “You don’t expect to see anything enormously different in your patient [in the short-term], but you hope they’re tolerating the drug well, and based on information from the literature, that you’re delaying disease progression.” “In the GRIPHON trial the dramatic changes we saw were in the long-term outcomes, the morbidity events, and that’s what I’m looking for in my patients,” concluded Prof Gaine.








