Andrew R.J. Mitchell | Consultant Cardiologist at Jersey General Hospital, Saint Helier, Jersey; Honorary Consultant Cardiologist at Oxford University Hospitals NHS Foundation Trust, UK
Citation: EMJ Cardiol. 2023; DOI/10.33590/emjcardiol/10300800. https://doi.org/10.33590/emjcardiol/10300800.
![]()
Please could you outline the primary duties you undertook while serving as Chief Clinical Information Officer for the Island of Jersey?
As well as being a full-time Cardiologist in Jersey and Honorary Cardiologist in Oxford, UK, I was appointed as Chief Clinical Information Officer for the Island of Jersey in Summer 2019. My mission was to set out a programme of work to transform the way that health data were stored, shared, and managed on Jersey. We developed a vision to create one of the most technologically advanced digital health systems in Europe, an ambitious target but potentially an achievable one. Jersey has some of the fastest internet connections in the planet, with fibre network to every habitable building as well as a connected mobile telecommunication services. We are also rated as one of the most advanced and regulated finance centres in the world, so we have a group of professionals who have a vested interest in accessing high quality, secure patient data. Alongside this, Jersey is the perfect place to test and innovate new digital health solutions. Our team has a dedicated digital health research laboratory called The Allan Lab, which is regularly approached by novel start-ups as well as established technology companies, looking to gain proof of concept and early-stage development data and funding. Many of these technologies have since been incorporated early into our clinical practice in Jersey.
Our programme of work changed with the onset of the COVID-19 pandemic. We accelerated some technology components and delivered new ways of remote working for our clinicians. We had to develop ways to communicate COVID-19 tests to and from the UK using multiple providers, wrote our own Jersey COVID-19 Alert application, and used digital health technologies to become one of the only paperless Nightingale hospitals in the British Isles.
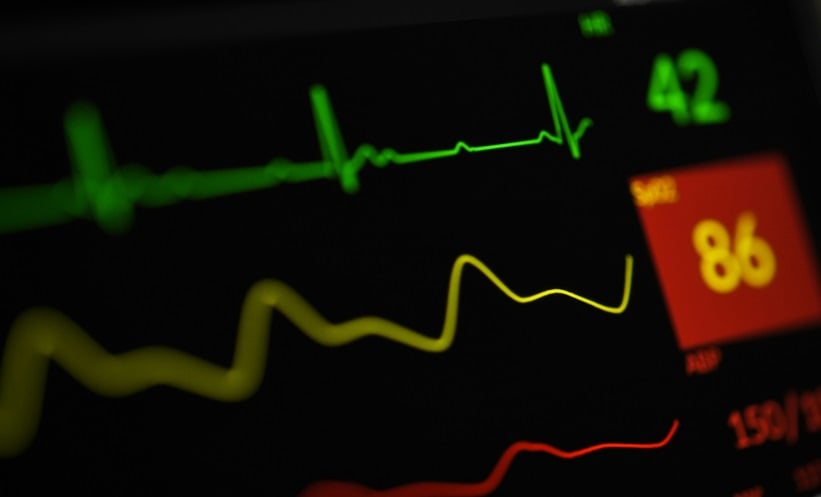
As we exit the pandemic, we have a new hospital being designed for Jersey over the coming years, so we have an amazing opportunity to incorporate and integrate some of the most innovative health technologies. Meanwhile The Allan Lab, led by director Austin Gibbs and supported by innovation fellow Chris Brown, continues to work in the field of immersive health technologies, ECG signal improvement, and is currently focusing on integrating clinical artificial intelligence (AI) solutions into our clinical practice.
Please could you explain the rationale and background of the Heart for Life programme, which you set up in Jersey in 2010 with your wife, Claire Mitchell?
Every week in the UK, at least 12 young children and adults die from sudden cardiac death. Many of these people had no idea that there was potentially something wrong with them. Heart screening using simple techniques such as a 12 lead ECG and an echocardiogram can pick up many of the cardiac abnormalities that increase the risk of death. As many of the conditions are hereditary, such as hypertrophic cardiomyopathy and long QT syndrome, cascade screening of first-degree relatives picks up even more cases allowing targeted interventions in those at highest risk.
In 2010 Claire and I launched Heart for Life to provide Islanders access to high quality heart screening. The website allows users to choose the package of heart tests that they want, as well as providing information about some of the common and less common heart conditions. We then set up and published a community heart screening research project to see if we could change the screening model and take our equipment to the students rather than bringing them to a clinic. We have subsequently been involved in screening the Jersey’s top football, rugby, and cricket teams. The service is currently provided as a user-pays model, but we have an aim to fund raise and develop a business model that allows us to provide heart screening free for all Islanders.
You have helped establish several charities in Jersey. Please could you describe the notable projects undertaken by these organisations and summarise their greatest achievements to date?
One of the biggest challenges I faced on moving to Jersey was accessing rapid government funding to appoint our Heart Team. Over the last decade, I have raised over 1.5 million GBP of charitable monies, which has allowed us to build the Jersey Heart Team and secure agreement for permanent government funding. Fundraising is hard and time-consuming but also emotionally rewarding. To support this work, and to develop new initiatives in Jersey, I helped establish the Jersey Heart Support Group in 2011. One of our first projects was to fund the provision of an automated external defibrillator to all schools in Jersey, making Jersey a place with one of the highest numbers of automated external defibrillators per capita in the British Isles.
Alongside this, I became a committee member of the new Jersey branch of the British Heart Foundation (BHF). We organised annual fund-raising events including Heart Hero awards and generated considerable monies for the charity. Our work in Jersey was recognised by the BHF in 2016 at an awards ceremony at the Houses of Parliament in London, UK.
I am currently working on a new and larger charitable project which is called the Jersey Research Foundation. This charity is designed to stimulate the concepts of research, innovation, questioning and entrepreneurship in Islanders. Grants will be offered to individuals across all industry in Jersey, including health, with the expectation that this will create new businesses and research opportunities in the Island.
You lead the Jersey Heart Team, which was selected as a ‘Syncope Pioneer’ by Syncope Trust and Reflex Anoxic Seizures (STARS) in 2021. Please highlight the work that resulted in this achievement.
Blackouts (syncope) are a common cause of hospital admission and as many as half the population will pass out in their life. This can often lead to hospital admission and investigations, which can be time-consuming and often unrewarding. We appointed a specialist nurse Kelly-Anne Kinsella to set up a dedicated Transient Loss of Consciousness Clinic (TLoC) to see and assess patients within a few days of presentation to hospital. We also trained up one of our clinical physiologists to implant loop recorders, increasing access to this valuable procedure. This reduced hospital admissions and bed stays as well as leading to more appropriate use of investigations and a more rapid clinical diagnosis. For this work, the team were included in the 2021 Syncope Pioneers report and Jersey General Hospital became recognised internationally as a centre of excellence.
In addition to being recognised as an international centre of excellence by STARS, the Jersey Heart Team has been shortlisted for several other prestigious national awards. Please could you tell us about these?
Jersey is a wonderful place to innovate and develop new health services. As Jersey is not part of the English National Health Service (NHS), we can extract components of healthcare guidelines from the UK, Europe, and North America and tailor our services to provide a unique way of managing heart (and other) conditions. In addition, we established a fellowship training programme attracting doctors who want to train in cardiology to get a year of high intensity clinical experience and teaching, launching them into successful UK cardiology rotations. Consequently, the Jersey Heart Team has been awarded numerous local and national awards for its innovative approach to healthcare management and training. Perhaps the most prestigious of these were to be shortlisted to the top four cardiology units in the 2016 Cardiology Team of the Year by the British Medical Journal. In addition, arrhythmia nurse specialist Angela Hall was selected by the Royal College of Nursing as Nurse of the Year in 2018. An amazing achievement when you consider there are over 700,000 nurses working across the British Isles. Personally, my work has been recognised by other organisations including the Arrhythmia Alliance, the Government of Jersey as well as the Institute of Directors, receiving a highly commended award in 2015 as UK Public Sector Director of the Year.
Could you provide an overview of your 2017 EMJ Cardiology article, entitled ‘Ectopic Beats: How Many Count?’
Ectopic beats are extra heat beats which usually come from the top (atrium) or the bottom (ventricle) of the heart. They are incredibly common, and most people will have a handful each day. In some people, however, ectopic beats can be associated with heart symptoms such as palpitation, as well as being linked with underlying heart conditions such as heart failure. For this reason, many patients seek medical advice when they notice an abnormal heart rhythm, or if they are alerted to it by a medical device such as a smart watch or a blood pressure machine. Our article reviews the current literature on ectopic beats and provides the treating physician with an understanding of when they should be deemed significant and when treatment may be appropriate.
How important do you believe digital health interventions are for the prevention of cardiovascular disease? Further, how can associations such as the European Society of Cardiology (ESC) and American College of Cardiology (ACC) ensure that digital healthcare remains a key priority for the cardiology community?
Most European healthcare services are established to look after people when they are ill or need an operation, but with current growth and demand, systems struggle to get adequate health staff and resource to deliver this efficiently. Digital health technologies are the enabler for a modern health service and will help move the focus away from care to prevention. One of the terms I use is that we need to start to ’de-doctorfy medicine’. We should give the patient access and control over their health data, as well as the digital tools and knowledge to monitor their own health condition so that they are less reliant on health staff. We can then move away from the current position where a patient asks the doctor what is wrong, to a point where the patient has a deep understanding of their health conditions as well as treatment options. By enabling these types of technologies patients can ‘take charge’ of their own health management. They can also start to access health care globally rather than locally, creating opportunities for health professionals in other countries as well as increasing capacity in the local network.
Coronary heart disease remains one of the leading causes of death yet many heart attacks are preventable. Digital machine learning technologies such as the assessment of fat-attenuation index in heart scans by Caristo Diagnostics (Oxford, UK) and AI technologies for assessing echocardiograms by Ultromics (Oxford, UK), offer an insight into how cloud-based software can, as a service, help to accurately predict patient’s risk and allow early risk reducing interventions. Novel AI systems such as from Google (Menlo Park, California, USA) and the ChatGPT service from OpenAPI (San Francisco, California, USA) are just the start of new augmented intelligence support systems.
Please could you share the key take-home messages from your 2020 EMJ Innovations article, entitled ‘The Era of Immersive Health Technology’?
Immersive health technologies are revolutionising the delivery of healthcare, therapeutic techniques, rapid knowledge access, and research. Our review paper summarises some of the current developments and describes the four main types of immersive health technology: augmented reality, virtual reality (VR), machine learning, and AI. VR systems are quickly developing and in clinical practice we now routinely offer clinical VR to patients undergoing invasive or uncomfortable procedures such as pacemaker implantation or pericardiocentesis. VR also offers great potential to improve the training of healthcare professionals through reality-simulation training, now available in a multi-user environment. In the paper, we described examples of the use of other immersive technologies in healthcare, their opportunities and pitfalls, and how the use of these technologies could be improved further in the future are highlighted. Systems such as AI and machine learning are providing clinicians with clinical support services, which are augmenting the knowledge based of health workers and, with the speed of development, it is probably one of the most exciting times to be involved in healthcare.