Abstract
Coarctation of the aorta is a congenital disease involving the cardiovascular system. It has a varied presentation and is often under-diagnosed in clinical practice. The authors report a case of an unusual presentation of coarctation of the aorta with a series of events leading to the final diagnosis. A 28-year-old man presented with complaints of backache and pain in both lower limbs with tingling and numbness for 8 months. He was provisionally diagnosed with spinal arteriovenous malformation based on investigations done elsewhere and was referred to the authors’ hospital for further management. On angiography, the transfemoral catheter and guide wire could not be negotiated beyond the descending thoracic aorta distal to the origin of the left subclavian artery. Transradial access demonstrated the coarctation of the aorta. Coarctation presenting as a spinal pathology is rare and has been described only in few of the literatures, so it is important to recognise it. This article also describes the pathophysiology and radiological features of coarctation.
Key Points
1. Coarctation of the aorta is a congenital cardiovascular disease with variable presentations, ranging from asymptomatic cases to acute emergencies, and can mimic other conditions.
2. This case report describes multiple tortuous flow voids in the spine on an MRI, which were initially misdiagnosed elsewhere as a spinal arteriovenous malformation. Later on, the patient underwent a digital subtraction angiography at the authors’ institute, where the patient was diagnosed with coarctation of the aorta. This was also confirmed on a CT aortogram.
3. Coarctation of the aorta can have a multitude of presentations, as illustrated by the authors’ case of a young man who was initially misdiagnosed with spinal arteriovenous malformation elsewhere. Due to its varied and sometimes atypical presentations, early and accurate diagnosis can be achieved with a proper understanding of the pathophysiology and the use of radiological investigations like CT and MRI, which are crucial for surgical planning and follow-up.
INTRODUCTION
Coarctation of the aorta is a congenital disease involving the cardiovascular system.1 The presentation can range from being asymptomatic to acute clinical emergencies. When symptomatic, the patients present with a myriad of symptoms like congestive heart failure in children, neurological deficits, lower limb claudication, hypertensive crisis, and intracranial haemorrhage. Knowing that the disease can present in many forms is important to avoid misdiagnosis. The authors report a case of a young man provisionally diagnosed with spinal arteriovenous malformation and was later found to have coarctation of the aorta. The pathophysiology and the radiological features of coarctation of the aorta have been discussed in this article.
CLINICAL CASE
A 28-year-old man presented with complaints of backache and pain in both lower limbs with tingling and numbness for 8 months. He had no significant medical history in the past. He was investigated with an MRI of the spine in a different hospital. On the MRI, there were multiple tortuous flow voids in the spine (Figure 1).

Figure 1: MRI of the spine.
Sagittal T1 (A) and T2 (B) weighted sequences of the MRI spine show multiple tortuous flow voids in the paraspinal, anterior subarachnoid space, and scapular regions (arrows).
Based on the history of backache and pain in both lower limbs, along with the findings from the MRI, a provisional diagnosis of spinal arteriovenous malformation was made. Since there was no facility for angiography in that particular hospital, the patient was referred to the authors’ hospital (tertiary care centre) for a spinal digital subtraction angiography. On digital subtraction angiography, the transfemoral catheter and guide wire could not be negotiated beyond the descending thoracic aorta distal to the origin of the left subclavian artery with non-opacification of the arch, suggesting coarctation of the aorta. A transradial access was obtained, and subsequent imaging confirmed the diagnosis. Extensive tortuous collaterals were noted (Figure 2), which were responsible for the tortuous flow voids seen on MRI.
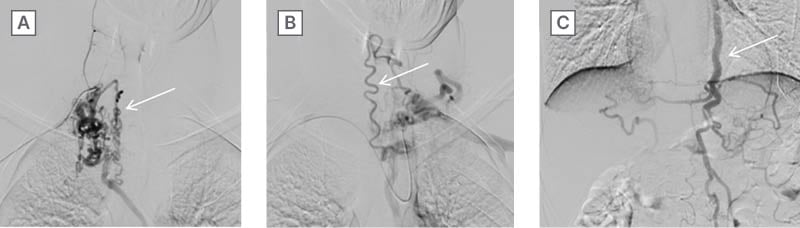
Figure 2: Digital subtraction angiography demonstrating coarctation of aorta.
Transradial angiography shows multiple collaterals. Right (A) and left (B) subclavian shoots show multiple dilated and tortuous spinal collaterals (arrow). Left subclavian shoot at the thoracodorsal level (C) shows prominent left internal thoracic artery (arrow).
The patient was referred to the Department of Cardiovascular Thoracic Surgery and was advised a CT aortogram, which showed a post-ductal coarctation with multiple intercostal, spinal, scapular, and paravertebral collaterals (Figure 3A, 3B, 3C).
A preoperative chest radiograph showed notching along the inferior aspects of the ribs with a “figure of 3” appearance (pre- and post-stenotic dilatation leading to the abnormal contour of the left mediastinal border, characteristic of coarctation; Figure 3D, 3E).
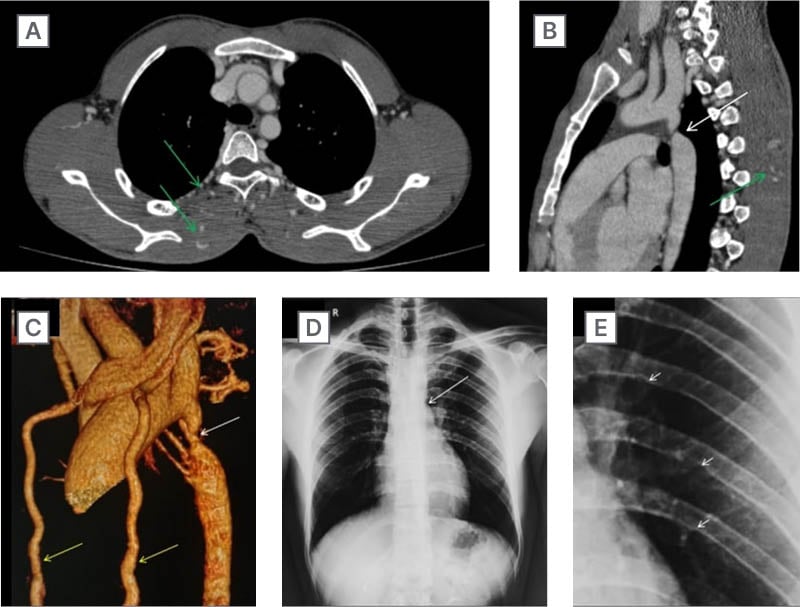
Figure 3: CT and radiographic findings in coarctation of aorta.
A) Contrast enhanced CT scan of the thorax shows multiple collaterals (green arrows) in the intercostal and scapular regions. B) Sagittal section shows post ductal coarctation (white arrow) with scapular collaterals (green arrow). C) 3D reconstructed CT image of the aorta shows severe narrowing (white arrow) in the aorta distal to the origin of the left subclavian artery. Both the internal thoracic arteries are prominent (yellow arrows). D) Frontal chest radiograph shows pre and post stenotic dilatation with “figure of 3” appearance (long arrow). E) There is notching (short arrows) of the inferior aspect of the third to ninth ribs on both sides; magnified.
A 2D echocardiogram was done, which showed turbulence at the site of coarctation with mild left ventricular hypertrophy.
The patient was offered surgical management in the form of coarctoplasty. However, due to financial constraints, the patient was managed conservatively on an outpatient basis and was lost to follow-up.
DISCUSSION
Coarctation of the aorta is a congenital anomaly of the cardiovascular system. It is a narrowing in the calibre of the aorta most commonly found adjacent to the attachment of the ligamentum arteriosum.1 The ductus arteriosus allows communication between the aorta and the left pulmonary artery, which is an important component of fetal circulation and is obliterated in post-natal life. Postnatally, the ductus forms the ligamentum arteriosum, which is a fibromuscular tissue with varying amounts of ductal tissue extending into the aorta. This leads to the development of coarctation of the aorta and explains the location of the narrowing in relation to the ligamentum arteriosum. Coarctation of the aorta is commonly associated with other congenital heart diseases, the most common being a bicuspid aortic valve. It is also commonly associated with Turner’s syndrome.2 Berry aneurysms are found in the intracranial vasculature in a few patients with coarctation. Coarctation can be preductal (common in children) or post-ductal (common in adults).2
Due to the narrowing of the descending thoracic aorta, there is hypoperfusion of the visceral organs and the lower extremities. To maintain adequate perfusion, there is a development of collateral circulation through various anastomotic channels. The extent of the collaterals varies depending on the severity of the narrowing. The common sites of collateral formation are the intercostal, scapular, and paraspinal regions, which were seen in the authors’ case in the form of flow voids on the MRI of the spine. The anterior intercostal arteries are a branch of the internal thoracic artery that arises from the subclavian artery. There are 11 paired posterior intercostal arteries, wherein the first two arise from the superior intercostal artery, which is the branch of the costocervical trunk of the subclavian artery. The rest arise from the descending thoracic aorta. The scapular anastomosis has its supply from the intercostal arteries apart from the branches of the subclavian and axillary arteries. The internal thoracic artery divides into the musculophrenic and superior epigastric arteries. The superior epigastric artery anastomoses with the inferior epigastric artery, which is a branch of the external iliac artery. The anterior spinal artery is a branch of the vertebral arteries that anastomoses with the branches of the descending thoracic aorta. These are the common pathways for rerouting the blood in cases of coarctation.3,4
The presentation of coarctation of the aorta varies from asymptomatic to acute emergencies. Clinical manifestation depends on the severity of the narrowing, the amount of collateral formation, and the presence of associated congenital diseases.2 In neonates, there may be changes in congestive heart failure due to increased afterload. Differential cyanosis or clubbing occurs due to hypoperfusion in the lower extremities. In a newborn, differential cyanosis indicates persistent pulmonary hypertension and left heart anomalies (aortic arch hypoplasia, interrupted arch, critical coarctation, and critical aortic stenosis). Reversed differential cyanosis may be seen in patients with transposition of great arteries and coexistent coarctation.4 In adults, the most common presentation is systemic hypertension. The proposed mechanism is renal hypoperfusion, which leads to the secretion of renin, which causes a rise in blood pressure. Other mechanisms include endothelial dysfunction, reduced arterial compliance, and blunted baroreceptor sensitivity.4 Other patterns of presentation include lower limb claudication, intracranial haemorrhage (due to aneurysmal rupture), backache, and lower limb weakness due to the mass effect of the spinal collaterals.7-9 Clinical examination findings include changes in the body habitus where the lower limbs appear atrophic due to hypoperfusion, radio-femoral delay, and differences in the systolic blood pressures between the upper and lower limbs. On auscultation, there may be a systolic murmur over the scapula.1
Transthoracic echocardiography is used for diagnosis as well as during the follow-up of patients with coarctation. The suprasternal notch acoustic window demonstrates the site of narrowing along with the Doppler-based gradients. A ‘diastolic run-off’ or ‘tail’ in the descending aorta is characteristic. The left ventricular mass and function can be assessed along with the presence of associated congenital anomalies.10
Radiology plays an important role in the diagnosis as well as management of the coarctation of the aorta. On a plain chest radiograph, there are subtle findings that may provide a hint about the diagnosis. The heart shadow is enlarged. There is prestenotic and poststenotic dilatation of the aorta resulting in the “figure of 3” sign.2 There is notching of the inferior aspects of the third to ninth ribs on both sides due to the extensive intercostal collaterals (Roesler’s sign). The first two spaces are spared as they arise from the subclavian system and are therefore preductal. The tenth and the eleventh posterior intercostal arteries do not anastomose with the anterior branch of the internal thoracic arteries. Rib notching is commonly bilateral. Unilateral rib notching may be seen if the narrowing is proximal to the origin of the left subclavian artery or if proximal to the origin of the aberrant right subclavian artery.11 CT has evolved to be one of the most important modalities in the diagnosis of coarctation. The properties of CT such as multiplanar reconstructions, the use of maximum intensity projection, and 3D reconstruction provide input on multiple factors such as the severity of coarctation, status of the collateral circulation, and associated other congenital anomalies.12-14 MRI has a promising role given its lack of ionising radiation, superior contrast resolution, and multiplanar imaging.15 MRI angiography can be done either with or without the use of intravenous contrast.16 Time-of-flight angiography can be used in cases where contrast agents are contraindicated in patients. The use of phase contrast imaging can provide the pressure gradient across the stenosis.2,17,18 Catheter angiography, although an invasive procedure, is considered a gold standard for the haemodynamic assessment in coarctation of the aorta.19,20 On angiography, it is possible to gauge the pressure gradient across the stenotic segment.
The differential diagnoses for rib notching on a chest radiograph include pulmonary arteriovenous fistula, neurofibromatosis, superior vena cava obstruction, patients with shunts (Blalock-Taussig), congenital heart diseases (tricuspid atresia, tetralogy of Fallot), etc.21,22 Interrupted aortic arch can be considered as a differential of coarctation, where there is a discontinuity between the arch and the descending thoracic aorta.23 Some consider it to be the most severe spectrum of coarctation. It is not seen in isolation and occurs commonly with other congenital defects such as a ventricular septal defect or a patent ductus arteriosus.24 Severe atherosclerotic disease can involve the mid-thoracic aorta and can be considered an acquired variant of coarctation.25 Few cases have been reported previously where coarctation has been misdiagnosed initially as spinal vascular malformation.7
The objective of treatment for coarctation of the aorta is to recanalise the stenotic segment by either surgical or endovascular methods. Surgical method includes resection and anastomosis, or the use of bypass grafts. Surgery is preferred in cases of infants with coarctation. The endovascular method involves balloon angioplasty or stenting.26,27
CONCLUSION
Coarctation of the aorta is a common congenital disease affecting infants and young adults. It has a varied presentation and often is under-diagnosed in clinical practice. It is important to understand the pathophysiology behind the presenting symptoms especially when the patient presents with atypical symptoms. With the aid of adequate radiological investigations, it is possible to diagnose coarctation of the aorta early and promptly. CT and MRI help in surgical planning and follow-up imaging.
Patient perspective
“I had these complaints for quite some time (many months) and have been visiting the hospital for the same. I am grateful that finally I know what disease I have although I am surprised that this is a condition I had since my childhood, but never experienced any symptoms till now. I hope the surgery is uneventful and I will be rid of my symptoms.”
Informed consent
Written informed consent has been obtained from the patient for drafting this manuscript and for publishing it.







