Abstract
Traditional qualitative methods for the assessment of coronary artery disease (CAD) have limited sensitivity, low reproducibility, and employ a binary approach to ischaemia. Quantitative assessment of ischaemia using cardiovascular magnetic resonance has emerged as a promising technique for CAD measurement. This review explores how to conduct quantitative assessment and the advantages of this over visual assessment alone, which include greater reproducibility and diagnostic accuracy. The authors provide an overview of how they currently use myocardial perfusion to assess CAD, indications, challenges, and opportunities to improve patient management and future directions.
INTRODUCTION
Myocardial perfusion can be performed using several different methods. In clinical practice, robust techniques include single photon emission CT (SPECT), PET, and cardiovascular magnetic resonance (CMR). CT perfusion was introduced more recently and, as a consequence, there is less evidence in the literature on this method compared with the first three techniques. The majority of meta-analyses examining the diagnostic accuracy of all of these available techniques have reported superior performance of PET and CMR, followed by SPECT.1,2
The 2019 European Society of Cardiology (ESC) guidelines for the diagnosis and management of chronic coronary syndromes3 suggest either anatomical imaging using coronary CT angiography (CCTA) or non-invasive functional imaging as the initial test for diagnosing CAD. Specifically, CCTA is the preferred test in patients with a lower range of clinical likelihood of CAD. However, when CCTA identifies obstructive coronary disease, functional assessment is recommended for further evaluation unless very high-grade stenosis (>90%) is detected.3 Moreover, non-invasive functional tests may be preferred if the patient has previously diagnosed CAD.3
STATE-OF-THE-ART IN ASSESSMENT
Qualitative Assessment
The CE-MARC study demonstrated that qualitative assessment of ischaemia with CMR had greater sensitivity than SPECT in both males and females.4 In particular, a CE-MARC sub-study showed that visual stress perfusion CMR had higher diagnostic accuracy than SPECT to detect left main stem disease.5 However, Yun et al.6 demonstrated that adding semi-quantitative CMR to qualitative stress magnetic resonance myocardial perfusion imaging led to higher sensitivity, particularly in the detection of left circumflex lesions.
Figure 1 shows an example of stress CMR with qualitative assessment.
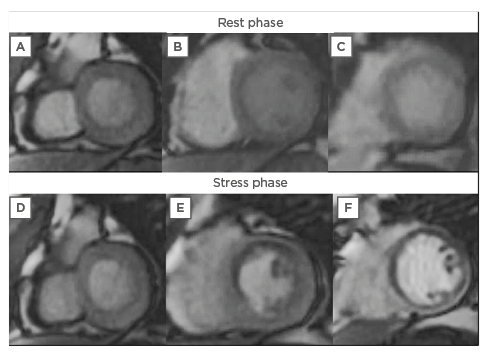
Figure 1: A perfusion qualitative assessment of stress cardiovascular magnetic resonance.
During rest phase (A, B, C), no perfusion defects are evident. After vasodilator stress, a subendocardial hypointense (darker) area indicating perfusion defect is observed at the level of the middle segments of the anterior interventricular septum and anterior wall (E) and at the level of all segments of the apex (F).
It is also important to note that 2 years ago, the Dan-NICAD study tested the diagnostic accuracy of myocardial perfusion (with visually-assessed SPECT and CMR) against invasive coronary angiography (ICA) with fractional flow reserve (FFR) in patients with suspected CAD by CCTA.7 The authors demonstrated that in this specific setting, likely to be increasingly common in clinical practice, the sensitivity of both CMR and SPECT, which were visually assessed, was low compared with FFR. This suggests that the diagnostic accuracy of qualitative perfusion may be insufficient for future clinical practice and that improvements are needed. Quantitative myocardial perfusion is, therefore, a promising way forward.
Moreover, Akil et al.8 found that, when compared to quantitative PET analysis, qualitative assessment displayed limited performance for the assessment of stable CAD, requiring elective revascularisation. The GadaCAD1 and GadaCAD2 trials demonstrated the high diagnostic accuracy of stress CMR for CAD.9
The three main limitations of qualitative CMR are: limited sensitivity, low reproducibility, and being a binary approach. This final point means that, according to this technique, ischaemia is either present or absent, but in reality, different levels of ischaemia are important for prognostic stratification. For these reasons, quantitative assessment is needed.
Quantitative Assessment
There are three different techniques for quantitative assessment. The dual-bolus protocol typically requires a complex set-up, state-of-the-art injector, and post-processing software. Ishida et al.10 developed a universal dual-bolus injection scheme, which eliminated the need for a sophisticated double-head power injector.
The pre-bolus technique requires two consecutive administrations of a contrast agent. The arterial input function is determined from the first low-dose bolus; the second, high-dose bolus enables the measurement of the myocardium with improved signal increase.11 This method allows for perfusion in the human heart to be quantified with a low variability, and the values correlate well with data from animal models and human PET studies.12
A single bolus with a dual sequence allowed separate optimisation of parameters for blood and myocardium in order to achieve linearity between signal and contrast agent concentration.13
Figure 2 shows an example of stress CMR quantitative assessment.
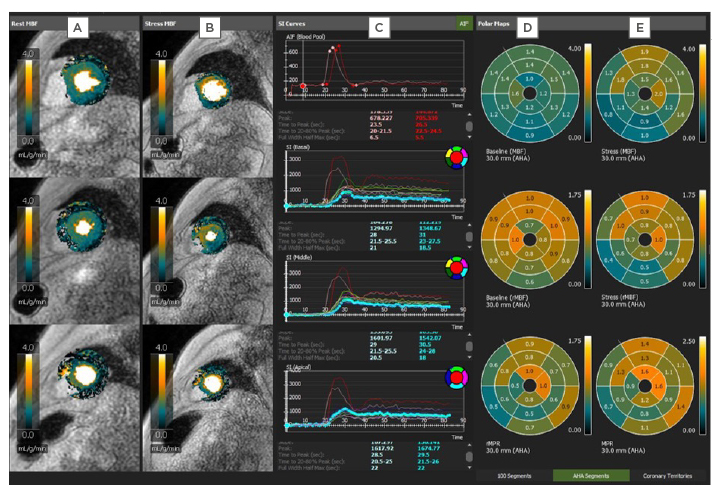
Figure 2: A perfusion quantitative assessment of stress cardiovascular magnetic resonance.
A and B) Pixel maps demonstrating quantitative myocardial perfusion at rest (A) and after vasodilator stress (B). C) Signal intensity curves. D and E) Polar maps showing myocardial blood flow values at rest (D) and after vasodilator stress (E).
Advantages of Absolute Quantification Versus Visual Assessment
There are numerous advantages of absolute quantification versus visual assessment alone, including improved reproducibility and diagnostic accuracy. Rahman et al.14 demonstrated that, compared with visual assessment, quantitative perfusion analysis techniques had a higher accuracy for correctly identifying the presence of coronary microvascular dysfunction.
A study by Villa et al.15 showed that the level of training was the main determinant of the diagnostic accuracy of visual assessment, while in a comparison of three levels of expertise, automated quantitative analysis performed similarly to Level 3 operators.
Lee et al.16 demonstrated that the capacity to detect functionally significant coronary stenosis was incrementally improved by the successive addition of coronary flow reserve, stress myocardial blood flow (MBF), and relative flow reserve to relative perfusion defect assessments.16 Meanwhile, the CE-MARC trial established the superior diagnostic accuracy of CMR over SPECT in coronary heart disease.17
A comparison of fully quantitative CMR against PET perfusion imaging in patients with CAD found good correlation between CMR-derived and PET-derived myocardial perfusion reserve measurements.18 Both techniques accurately detected significant CAD. However, absolute perfusion values from PET and CMR were weakly correlated. A further study found good agreement between myocardial perfusion quantified by PET and dual sequence, single contrast bolus CMR in patients with stable CAD.19
Importantly, the logistical challenges related to PET are well known. These include the high cost and limited availability of PET for cardiac imaging due to huge demands from oncology.
ROLE OF EVALUATING MYOCARDIAL PERFUSION IN THE MANAGEMENT OF CORONARY ARTERY DISEASE
Use of Myocardial Perfusion to Assess Coronary Artery Disease
In the authors’ clinical practice, CT has been used extensively as the first-line for anatomical evaluation. When the CT is positive for obstructive CAD, myocardial perfusion should also then be performed, unless very high-grade stenosis (>90%) is detected. Moreover, CMR is more frequently used as a first-line test in symptomatic patients with a previous history of revascularisation. In this subset of patients, a higher cost effectiveness compared to anatomical assessment with CCTA was demonstrated by the authors.20
According to the Dan-NICAD study,17 in the setting of obstructive CAD, there is a huge need for quantitative perfusion because qualitative perfusion alone is not sensitive enough. As a result, the authors have already started clinical examinations using quantitative perfusion on top of anatomical assessment with CT in order to increase diagnostic accuracy,21 and now that sequences and post-processing are available, they will begin assessments using quantitative perfusion with CMR.
HOW ABSOLUTE QUANTIFICATION WITH CARDIOVASCULAR MAGNETIC RESONANCE IMPROVES MANAGEMENT OF PATIENTS WITH CORONARY ARTERY DISEASE
Improvements in Management
Absolute quantification of flow should, theoretically, improve management by delineating different levels of ischaemia, as opposed to a binary result that is either positive or negative for ischaemia. This could distinguish between patients with a mild, moderate, or severe reduction of MBF, and with a lower or higher amount of myocardial mass. Currently, this is an appealing hypothesis that must be proven in future studies. A goal for the future of quantitative perfusion is to identify an optimal threshold that can be used in clinical practice to distinguish between patients with CAD who require medical therapy and the minority of patients with CAD who require revascularisation.
Furthermore, the MR-INFORM trial demonstrated that, in patients with stable angina and risk factors for CAD, the use of myocardial perfusion CMR to guide initial management was non-inferior to the use of ICA combined with FFR, with respect to major adverse cardiac events at 1 year.22 CMR was also associated with a significantly lower incidence of ICA and coronary revascularisation than was the use of FFR.
Regarding diagnosis, automatically generated, fully quantitative CMR MBF pixel maps were shown to have high diagnostic performance for detecting significant CAD.23 Quantitative myocardial perfusion has also shown value in prognostication. In a large study of patients with known or suspected CAD, reduced MBF and myocardial perfusion reserve were measured automatically using artificial intelligence quantification of CMR perfusion mapping, which provided a strong, independent predictor of adverse cardiovascular outcomes.24
Indications
In the authors’ clinical practice, the first indication for quantitative assessment is patients with a positive CT. The second indication is patients with complex coronary artery anatomy, for whom CT is not a useful examination. In these patients, the authors suggest to go directly to functional testing with stress CMR. In addition, CMR is able to provide the best information for the management of patients with chronic total occlusion. Finally, quantitative assessment is used for the prognostic stratification of patients with cardiomyopathy.
From the authors’ experience, they note that there is minimal use of perfusion in hypertrophic cardiomyopathy,25 amyloidosis, Fabry disease,26 etc., where the focus is primarily on tissue characterisation. There is a need to enlarge the evidence base on the prognostic role of myocardial perfusion in these settings since a qualitative approach is insufficient.
Challenges
Currently, the biggest limitation of quantitative perfusion is a lack of reference values. There are many confounders that can influence MBF thresholds, such as cardiovascular risk factors. In the absence of epicardial vessel disease, patients with hypertension and diabetes can have a normal value that is lower than patients with no hypertension and no diabetes; work to establish thresholds for these is ongoing. Another challenge is the cost and lack of availability of perfusion CMR in all centres.
Automated quantitative perfusion CMR results are more reliable as fully quantitative pixel-wise analysis has a better discrimination of dark rim artefacts, a common limitation of visual analysis.27 Machine learning approaches will be important in moving this area forward. Once quantitative perfusion has started to be used in a large number of patients, their data must be entered into large registries that track outcomes. Using artificial intelligence, robust MBF thresholds that are related to patient outcomes can then be established.
CONCLUSION
At the moment, the diagnosis of CAD is a puzzle. Evidence is accumulating that qualitative perfusion is not a sufficiently vigorous method to identify future cases, but there is encouraging data suggesting that quantitative perfusion could be a solution. However, there is still work to do: more prognostic data still needs to be generated, and thresholds that correlate with outcomes must be defined.








