Abstract
Introduction: Coronary intervention is a therapeutic method for acute coronary syndrome.
Objectives: Characterise patients with acute coronary syndrome treated by percutaneous coronary intervention.
Method: Analytical, observational, retrospective, and cross-sectional study of 1,469 patients with the diagnosis of acute coronary syndrome, treated with percutaneous coronary intervention at the Hermanos Ameijeiras Hospital, Havana, Cuba, between 2010–2019.
Results: The mean age of the patients was 61.1±10.6 years, 72% were male, and 68.3% had acute coronary syndrome without persistent ST-segment elevation. The commonest risk factor was hypertension (69%). Radial access was used in 75.0% of procedures, and 82.0% had a single occluded epicardial coronary artery (42.4% anterior descending artery, 29.7% right coronary artery). One (63.3%) bare metal stent was implanted in 70.7% of patients, with a 96.0% angiographic success rate. There were complications in 1.1% of cases. Diabetes was significantly associated with the failure of the procedure.
Conclusions: Most of the patients were middle-aged, with hypertension and a diagnosis of non-ST-segment elevation acute coronary syndrome, where the most frequently treated artery is the left anterior descending artery, and the radial artery is the most commonly used vascular access route with an elevated number of successful procedures. The presence of diabetes is significantly associated with the failure of the procedure.
Key Points
1. Identifiable and treatable risk factors are significantly prevalent in middle-aged patients with acute coronary syndrome.
2. This was an analytical, observational, retrospective, and cross-sectional study of 1,469 patients with the diagnosis of acute coronary syndrome, treated with percutaneous coronary intervention at the Hermanos Ameijeiras Hospital, Havana, Cuba, between 2010–2019.
3. The presence of diabetes was related to the failure of percutaneous coronary intervention.
INTRODUCTION
Cardiovascular diseases are the leading cause of mortality worldwide. The total prevalence of cardiovascular disease has almost doubled from 271 million in 1990 to 523 million in 2019, and the number of deaths from cardiovascular causes has progressively increased from 12.1 million in 1990 to 18.6 million in 2019.1
In the USA, 697,000 people died in 2020 due to cardiovascular causes; one in five deaths. That is equivalent to one death every 34 seconds. Half of these deaths were due to coronary artery disease (CAD). Each year, 805,000 persons have an acute coronary syndrome (ACS), equivalent to one every 40 seconds.2
Between 2019–2020, 56,993 people died in Cuba from cardiovascular causes, making it the leading cause of mortality in Cuba. Almost half of these deaths were due to ACS. This translates into 12.8 and 12.9 years of potential life lost, respectively. Worldwide, mortality caused by cardiovascular disease continues to increase, making it the third cause of all death in 2019.1,3,4
ACS has a variable clinical expression, such as acute myocardial infarction, unstable angina, and sudden cardiac death. They are mainly a consequence of atherosclerosis of the coronary arteries.#5,6
Many risk factors (RF) have been related to ACS. For preventive purposes, these risk factors are divided into non-modifiable (age, sex, genetics) and modifiable (hypertension, obesity, smoking, diabetes, dyslipidaemia). The presence of certain clinical entities, such as chronic kidney disease, atrial fibrillation, heart failure, and malignancies, among others, also increases the risk of major adverse cardiovascular events. RFs may not be distributed similarly in all populations; however, they are present in an important proportion of patients with CAD, being an important challenge for different health systems.7-12
Patients with ACS have been classified into ACS with ST-segment elevation (STE-ACS) and ACS without persistent ST-segment elevation (NSTE-ACS), given the importance of the worse prognosis associated with the first group, and the benefit derived from prompt reperfusion.10,13-15
Patients with STE-ACS and NSTE-ACS (very high-risk and high-risk subgroups) have an indication for invasive coronary angiography with the intention of performing percutaneous coronary intervention (PCI), given the proven effectiveness and superiority of resolving the pathological substrate causing coronary occlusion (atherothrombotic in most patients).16
When performing invasive coronary angiography in patients with ACS with an indication for this procedure, the intention is to demonstrate occluded epicardial arteries (responsible for the clinical episode) and proceed to carry out angioplasty with balloon/placement of a stent (in patients who have favourable coronary anatomy) to open the culpable artery, thus reperfusing the segment of myocardium at risk. In a proportion of patients, no epicardial obstructive lesion is demonstrated during coronary angiography, the so-called myocardial infarction with non-occlusive coronary arteries (MINOCA). Coronary lesions not responsible for the current clinical episode can also be identified. The ideal therapeutic approach to these lesions is still the subject of active research.10,17
Several interventions have demonstrated their therapeutic efficacy and decreased mortality in patients with ACS. These include continuous monitoring of patients in coronary units, fibrinolysis, dual antiplatelet therapy, and early use of β-blockers. The COLCOT study has shown the effectiveness of the anti-inflammatory drug, colchicine, in the prevention of post-ACS major adverse cardiovascular events.18
In the Cuban population, there is a high incidence of CAD, with ACS being a common form of presentation. The use of PCI as an invasive treatment method in this entity is increasing progressively given the improvement of the technique and the advances in the materials used. Knowledge of the factors associated with the success of coronary intervention increases its clinical benefit and helps risk stratification in these cases. The authors found few studies published in the country with a large sample offering statistical strength to the analysis, hence the decision to carry out this study. The aim of this research is to characterise patients with ACS treated by PCI.
METHODS
This was an analytical, observational, retrospective, and cross-sectional study. It was carried out in the Department of Interventional Cardiology, Cardiology Service of the Hermanos Ameijeira Clinical-Surgical Hospital in Havana, Cuba, from 1st January 2010–31st December 2019. The sample was made up of patients who were treated with PCI in the haemodynamics laboratory of the Hermanos Ameijeiras Hospital during the study period. Inclusion criteria included age over 18 years, diagnosis of ACS, and treatment with PCI. Exclusion criteria included patients with an incomplete report of the interventional procedure.
Sample
From a total of 1,502 patients, 33 were excluded due to incomplete documentation of clinical data on the paper records from the archives, which may have occurred due to the stress of workflow at the cathetirisation laboratory. These cases were distributed randomly in the first 7 years of the investigation. The sample was made up of 1,469 consecutive patients who met the inclusion criteria.
Data Collection Techniques
At the institution where the research was carried out, there is a printed form with the demographic and clinical data of the patients treated by PCI, as well as a digital record, in addition to those related to the procedure. This evidence is kept on file, for research purposes only, in the interventional cardiology department. For the current investigation, a duplicate report of patients treated in the context of ACS was obtained. These records match the electronic record data for these patients. The data was collected in a form designed for this purpose and processed with version 20.0 of the SPSS Statistics program (IBM, Armonk, New York, USA).
Ethical Issues
Authorisation was requested from the hospital in order to access patient data. Subsequently, approval from the Research Committee of the institution was obtained. The confidentiality of patient data was respected while clinical records were examined. Only the authors accessed these records, and the Helsinki Declaration was respected.19
Techniques of Processing and Analysis of Data
The collected data was transferred to an Excel (Microsoft, Redmont, Washington, USA) database designed for this purpose. Statistical analysis was carried out with version 20.0 of the SPSS Statistics software package (IBM).
Variables were summarised in absolute numbers and percentages. To analyse the relationship with the qualitative variables, the χ2 test was performed, with correction, and when there were 25% or more expected frequencies lower than five, Fisher’s exact test was used. The results were presented in tables and graphs as applicable, to facilitate their better reading and understanding.
RESULTS
Table 1 shows the distribution of demographic variables, such as age and sex. It was observed that age had a natural distribution (sigmoid) where most patients were between 40–69 years old. There was a clear predominance of patients of the male sex. Clinical variables, such as the presence of risk factors, and the clinical diagnosis with which they presented to the hospital, can also be observed in this table. Hypertension, smoking, and diabetes represent the most important risk factors in these patients, present in 69.0%, 31.2%, and 23.3% of the sample, respectively. Most of the patients (68%) presented with NSTE-ACS.
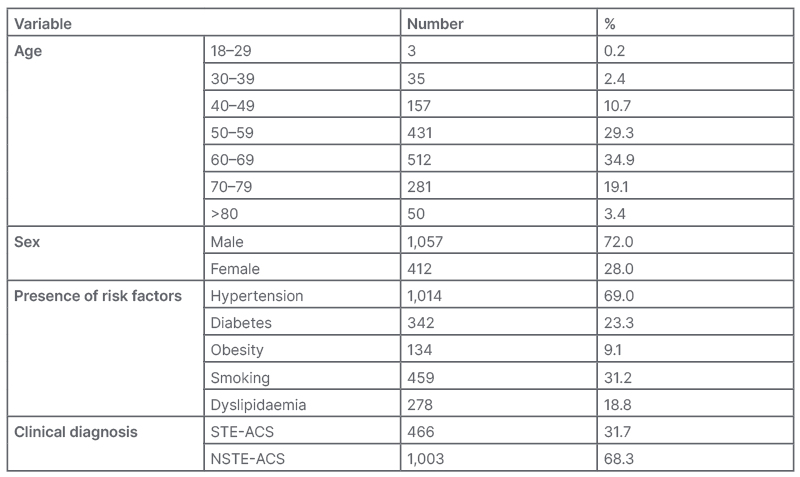
Table 1: Distribution of the demographics and clinics variables of the patients.
Source: Percutaneous Coronary Intervention Report.
NSTE-ACS: non-ST-elevation acute coronary syndrome; STE-ACS: ST-elevation acute coronary syndrome.
The distribution of the angiographic variables is described in Table 2. The left anterior descending artery (LAD) was the most affected artery in ACS, followed by the right coronary artery (RCA). No angiographically significant coronary artery occlusion was identified in 12.9% of patients. The majority of patients (82%) had a culprit lesion in an epicardial artery. A single stent was implanted in 63% of cases, and the most widely used were bare metal stents (BMS; 70%). Three-quarters (75%) of the angioplasties were performed via radial access.
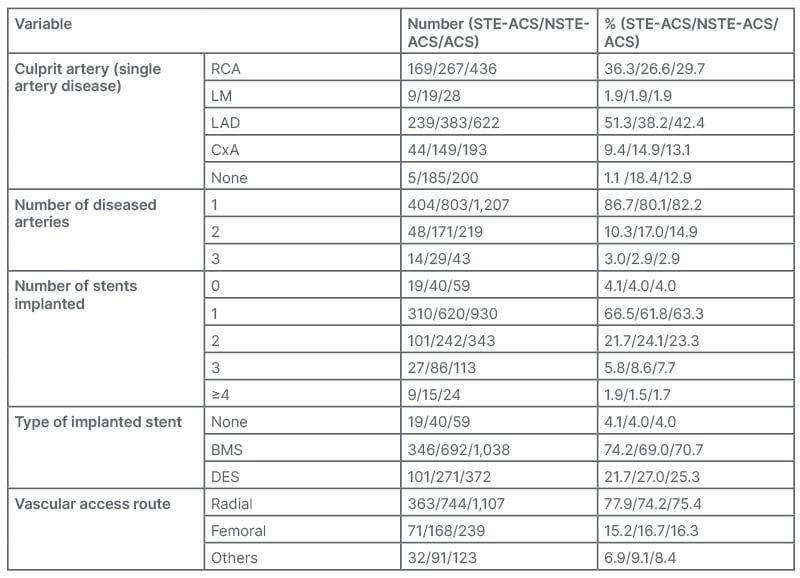
Table 2: Descriptive statistics of angiographic variables.
Source: Percutaneous Coronary Intervention Report.
ACS: acute coronary syndrome; BMS: bare-metal stent; CxA: circumflex artery; DES: drug-eluting stent; LAD: left anterior descending artery; LM: left main artery; NSTE-ACS: non-ST-elevation acute coronary syndrome; RCA: right coronary artery; STE-ACS: ST-elevation acute coronary syndrome.
The complication rate was low (1.1%), with death being the most common complication in this study, with 11 patients (0.7%) dying during the study period. Almost all the procedures performed during this period were considered successful (96.1%).
Of the failures, the most common cause was the presence of a fatal complication or technical difficulty in stent implantation that led to the termination of the procedure.
Table 3 shows no statistically significant relationship between the demographic variables (age and sex) and the final assessment of the procedure. The presence of diabetes is related to an unsuccessful final angiographic result of the procedure. The presence of the other risk factors did not significantly affect the final result. In addition, the clinical diagnosis was not statistically significant for the final result either.
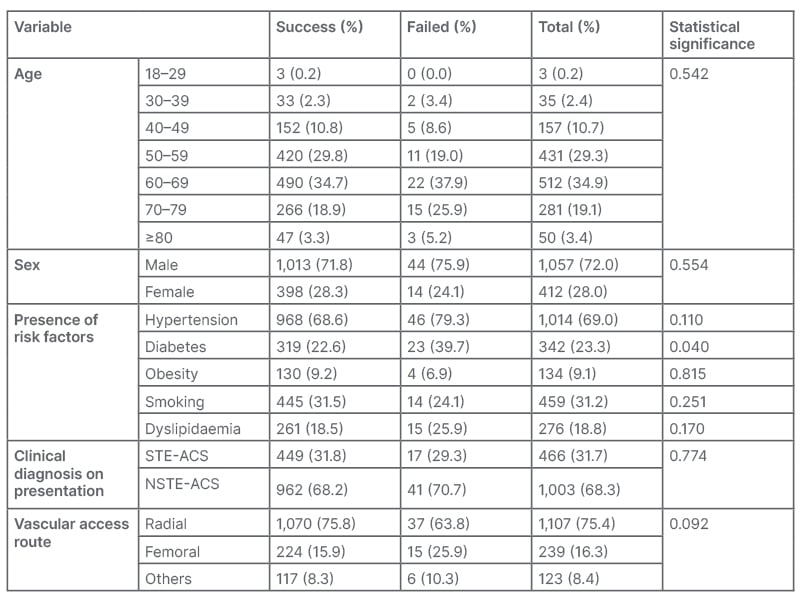
Table 3: Relationship between demographic, clinical, and vascular access route versus clinical variables.
Fisher’s test was used; p=0.05.
Source: Percutaneous Coronary Intervention Report.
NSTE-ACS: non-ST-elevation acute coronary syndrome; STE-ACS: ST-elevation acute coronary syndrome.
During PCI to the LAD and RCA, the most frequently treated coronary arteries (49.2% versus 33.6% of successful cases, respectively), there were disproportionately more failures of the procedure in RCA (45.1%) compared with the LAD (35.3%). Of the patients who received stents, 100% of the failures occurred in patients receiving BMS. It should be noted that the majority of patients who did not receive a stent (N=59) includes those who underwent balloon angioplasty, and those in whom the implantation failed. The implantation of one or two stents was significantly related to the success of the procedure. The use of radial access showed a higher success rate as compared with the rest of the access routes studied, although without being significant (p=0.09).
DISCUSSION
The findings of age, sex, and clinical diagnosis of this study coincide with those found by other researchers such as Galappatthy et al.,20 who found an average age of 61.4±11.8 years, with 32.8% presenting with STE-ACS. Montero-Jimeno et al.21 found a predominance of males (51.89%) in patients with ACS, although patients with STE-ACS predominated (54.7%). In their study, Guerra-Frutos et al.22 observed a prevalence of the male sex (65.30%) and the most affected age group was 60–69 years (30.61%).10,20-23
Park et al.24 in their study found that young patients with significant coronary lesions, compared with older patients (>70 years), were mainly male, smokers, and had elevated lipid profiles (total cholesterol, low-density lipoprotein-cholesterol, and triglycerides), findings similar to the results of this present study. In young patients, no statistical association was observed between hypertension, diabetes, and previous myocardial infarctions. Guerra-Frutos et al.23 and Mohsen et al.25 found hypertension as the most common RF in patients with STE-ACS. Valdés-Martín et al.26 found that the most common RFs in patients younger than 45 years with STE-ACS were tobacco use, hypertension, and dyslipidaemia.
Fonseca-Marrero et al.27 pointed out that tobacco use is an RF related to STE-ACS.23-27
De Lange et al.28 observed that being female, young, and non-diabetic had a high probability of having normal or near-normal coronary arteries at invasive coronary angiography. Ayach et al.,29 in their study on ACS in patients under 35 years of age, found that male sex (91.0%) was a risk factor for NSTE-ACS and having multi-vessel CAD (43.8%). According to Shi et al.,30 early ACS (<55 years in females) predominated, and regression analysis in the same study revealed female sex was an RF for early ACS, as was hypertriglyceridaemia.28-30
The most frequently obstructed epicardial coronary artery was the LAD (42%), followed by the RCA (29.7%), unlike what was found by Wang et al.,31 where RCA (44%) was the most frequently obstructed, followed by the LAD (40%). Most (82%) of the patients in this sample had a single angiographically occluded epicardial coronary artery. Patients with ACS with non-obstructive coronary arteries, a subgroup that includes acute MINOCA, represent 12.9%, a figure similar to that found by other authors, in a range of 1–14%. The use of biomarkers in this study was not documented; therefore, myocardial infarction per se cannot be discussed. However, the group of patients with STE-ACS without angiographically significant coronary lesions, 1.1% of the sample, could be part of the subgroup with MINOCA (Table 2). Valdés-Martín et al.26 found that most of their sample had an occluded epicardial coronary artery. In the majority, the LAD (40.4%) and the RCA (28.3%) were the most affected epicardial coronary arteries. No angiographically significant coronary lesions were present in six patients (20.0%) of the 30 patients with STE-ACS in the sample, and PCI (56.6%) was the most widely used revascularisation method in STE-ACS.10,26,31,32
Cid Álvarez et al.33 described the use of drug-eluting stents in 92% in Spain as of 2017, while the most used stent in this study is the BMS (70.5%) due to its greater availability in this setting for reasons beyond the scope of this study. The use of the radial access route, which is the default, was practiced in 75% of the sample of this study, slightly lower than what was found in the Spanish registry (1990–2018), with a penetration of 86.4% of the use of the said route. It is expected that the use of radial access during PCI in this centre will increase given its proven superiority, especially in local complications33-39 (Figure 1).
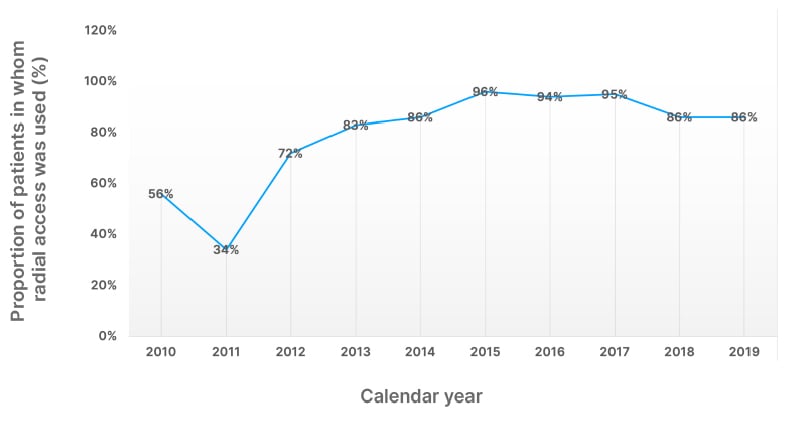
Figure 1: Proportion of radial access use in percutaneous coronary intervention for acute coronary syndrome during a 10-year period at the Hermanos Ameijerias Hospital, Havana, Cuba.
Source: Percutaneous Coronary Intervention Report.
Very few complications were registered during the period of study, including 11 fatalities (0.7%). More fatal complications were documented than non-fatal ones in this study. Being a retrospective study, it is known that there could be an inherent problem of underreporting data for the purpose of a statistical study. The success rate of PCI in ACS in this study was 96%. This could be explained by the participation of well-trained operators, and partially because of the bias present in data collection in a retrospective study.40,41
In this study, no statistically significant relationship between age, sex, and clinical diagnosis was demonstrated. Failure of the procedure had a statistically significant association (p=0.04) with the presence of diabetes. The superiority of coronary artery bypass graft to PCI in patients with diabetes with multivessel CAD has been demonstrated in chronic coronary syndrome, but not in ACS. The RCA, the second most frequently occluded artery in this study, had disproportionately more failed cases, being a possible explanation for the highly significant relationship calculated. Technically, RCA ostium cannulation can be more difficult than ostium of the left main artery; however, Welty et al.42 found no differences in the success of PCI to the RCA versus the LAD or circumflex artery, unlike the results obtained by Savage et al.,42 who found a significant relationship between PCI to the RCA and failure of the procedure.42-46
The number of stents used in this study paradoxically had a reverse relationship with the success of the procedure, taking into account that complex lesions could require more stents, which translates into a greater risk of complications and/or failure of the procedure. The implantation of increasing numbers of stents is related to in-stent restenosis, an objective beyond the scope of this study. The stents used during the period of this study (mostly BMS) had a wider profile and more difficult manoeuvrability
compared to current stents, which may explain the high proportion of failures with BMS stents in this study, making the statistical relationship between the type of stent and the success of the procedure insignificant. Regarding the use of radial access, there is also a positive relationship with the outcome of the procedure, although insignificant.37-41,45
CONCLUSIONS
To conclude, most of the patients were middle-aged, hypertensive, diagnosed with NSTE-ACS, and the most frequently treated artery was the LAD. The vascular access most frequently used was the radial artery and PCIs had a high success rate. The presence of diabetes was significantly associated with the failure of the procedure.
RECOMMENDATIONS
The authors recommend to do further studies, preferably prospective, where all complications (major and minor), including those related to the vascular access route, are collected and actively documented. They further recommend the implementation of preventive and therapeutic strategies to control coronary risk factors in the Cuban population.







