BACKGROUND AND AIMS
Out-of-hospital cardiac arrest (OHCA) is the most common cause of cardiac-related death, and continues to be a public health burden with poor survival.1-3 Cardiovascular disease is the leading cause of death among females, who are known to have a different presentation compared to males.4 Although sex differences in cardiovascular diseases are well described, they have not been completely understood in survival after OHCA.
Therefore, the aim of this study was to examine sex differences in patient characteristics and the 30-day survival in patients with OHCA during 20 years of follow-up.
MATERIALS AND METHODS
The authors conducted an observational and register-based study, using nationwide Danish register data. All residents in Denmark have a unique person identification number, which enabled the authors to crosslink data from different registers on an individual level. From the Danish Cardiac Arrest Registry, they identified all patients with OHCA between 2001–2020, who were aged between 18–100 years, with a presumed cardiac cause of OHCA, which was not witnessed by emergency medical services during their arrest. Baseline characteristics were expressed as medians (quartile 1–3) or frequencies (percentages), and temporal trend analyses of 30-day survival were performed according to sex.
RESULTS
Between 2001–2020, a total of 50,270 patients with OHCA were included, 17,179 of whom were female (34%). Compared to males, females were older, with a median age of 76 years (quartile 1–3: 66–84), and were more likely to have a low socioeconomic status. Females had a higher burden of chronic obstructive pulmonary disease (19% versus 14%; p<0.001), and psychiatric disease (13% versus 8%; p<0.001). By comparison, males had more ischaemic heart disease (24% versus 17%; p<0.001) and diabetes (17% versus 14%; p<0.001).
Looking at medication use 180 days before OHCA, females had more prescriptions of antibiotics (48% versus 35%; p<0.001), steroids (18% versus 13%; p<0.001), and QT-prolonging drugs (17% versus 11%; p<0.001). Males had more prescriptions of anticoagulant drugs (17% versus 13%; p<0.001) and statins (32% versus 25%; p<0.001).
Related to cardiac arrest-related factors, OHCA experienced by females were more often in a private home (83% versus 74%; p<0.001), were less likely to be witnessed by a bystander (48% versus 53%; p<0.001), and were less likely to have shockable heart rhythm by emergency medical services arrival (14% versus 28%; p<0.001). No sex differences were observed for receiving cardiopulmonary resuscitation.
In analysis of the temporal trend of OHCA incidence and 30-day survival by sex during 2001–2020, an increase in 30-day survival for both sexes was observed (Figure 1). However, females had lower 30-day survival compared to males throughout the period of study. The average 30-day survival by sex during 2001–2010 versus 2011–2020 was 5% versus 8% for females, and 8% versus 15% for males, respectively.
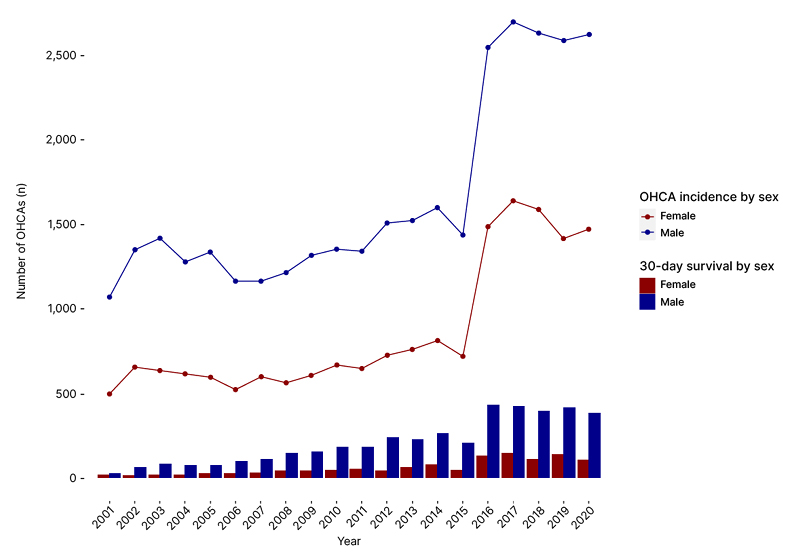
Figure 1: Temporal trend of out-of-hospital cardiac arrest incidence and 30-day survival by sex during 2001–2020.
OHCA: out-of-hospital cardiac arrest.
CONCLUSION
Females had poorer prognostic patient characteristics and cardiac arrest-related factors compared to males. Although 30-day survival improved in both sexes during the period 2001–2020, females had lower 30-day survival compared to males. Further research is warranted to understand sex differences of patients with OHCA, in order to improve survival rates among females.







