The prevalence of atrial fibrillation (AF) increases every year; some scientists project that between 2010 and 2060 the number of AF patients in the European Union (EU) aged ≥55 “will more than double.”1 In the context of population ageing, expert members of AF-SCREEN, an “international collaboration […] formed in September 2015 to promote discussion and research” about AF prevention, recommend AF-screening for patients ≥65 years old.2 Other studies, for instance REVEAL AF,3 show that undetected AF is extremely frequent, especially in patients with increased risk factors. This demonstrates the importance of this topic and confronts us with the question of therapeutic control mechanisms.
Within the observational HAMBURG-AF study, we aimed to evaluate the determinants of conversion into sinus rhythm during initial stay at the emergency department of a large tertiary care centre. A total of 1,384 subjects were recruited between October 2014 and April 2017. We included patients with AF as a primary diagnosis and excluded patients with permanent AF. For those with repeated visits we used only the first visit (Figure 1). A total of 663 (71%) were classified as paroxysmal AF. Of these, 68.4% converted into sinus rhythm during the hospital stay, 29.6% due to medication (potassium/magnesium and/or beta-blocker), and 31.6% due to electric cardioversion. The remaining 7.2% converted spontaneously into sinus rhythm. The mean patient age was 75.0 (65.0–81.0) years. Of the patients, 45.7% were male, 69.0% presented with hypertension, 21.1% with coronary artery disease, and 30% with secondary AF, such as bacterial infection. In multivariate age and sex-adjusted logistic regression analysis, previous interventional ablation therapy was strongly associated with conversion in sinus rhythm during the hospital stay (Table 1). Less surprisingly, our large, real-world study documented a strong negative predictive effect of secondary AF, as well as impaired left-ventricular ejection fraction on conversion rates.
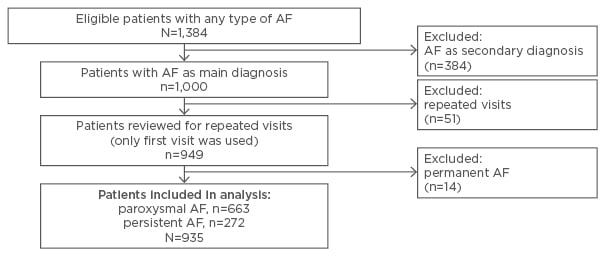
Figure 1: Criteria for inclusion in study.
AF: atrial fibrillation.
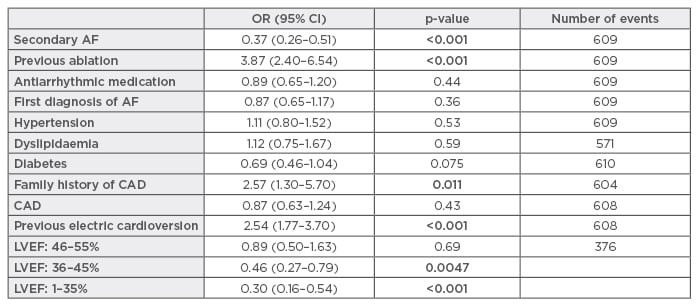
Table 1: Analysis of study results.
AF: atrial fibrillation; CAD: coronary artery disease; CI: confidence interval; LVEF: left ventricular ejection fraction; OR: odds ratio.
Catheter ablation has now emerged as a key interventional therapy and is recommended for drug-refractory AF. Over recent decades, catheter ablation has established itself as a frequently applied treatment strategy for patients with AF. After successful ablation therapy, patients benefit from fewer symptoms, better heart function, a reduced risk of stroke events, and a reduced all-cause mortality. Nevertheless, multiple studies suggest high recurrence rates and guidelines nowadays recommend further ablation therapies in those with symptomatic relapses.
This first prospective real-world report on the determinants of facilitated conversion in sinus rhythm in those with recent-onset AF strongly documents the long-standing benefits of interventional catheter ablation therapy.








