Abstract
Drug allergy, in clinical practice, includes a wide spectrum of immunologically-mediated hypersensitivity reactions, also called drug hypersensitivity reactions (DHRs). It can present with diverse clinical manifestations and can have various underlying pathophysiological mechanisms. Drug allergies often require a number of investigations and this can sometimes lead to a delay in treatment of the original disease. Drug allergy can affect quality of life too. It does contribute to significant morbidity and even mortality which is largely avoidable. Meticulous relevant details in history and clinical examination are often rewarding in arriving at the correct diagnosis. Patients with underlying chronic airways diseases such as asthma may benefit from skin tests and graded allergen challenges. Procedures to induce drug tolerance are sometimes helpful in the drug allergy management. Likelihood of cross-reactivity among drugs should be taken into account while choosing alternative medication. Measures for drug allergy reactions are mostly supportive and usually include topical corticosteroids and oral antihistamines. However, systemic corticosteroids may be required in severe DHRs along with adrenaline in the event of anaphylaxis. The most effective approach towards the problem of ‘drug allergy’ is discontinuing or avoiding the offending culprit. Procedures to induce drug tolerance may be considered as a temporary measure toward tolerance to the offending drug if there is no alternative available.
This article aims to provide a simple clinical review of drug allergy and plan of action for the diagnosis as well as management of some of the most common DHRs, such as allergies to acetylsalicylic acid, non-steroidal anti-inflammatory drugs, penicillins, sulpha drugs, cephalosporin, contrast media in imaging procedures, anaesthetic agents, and vaccines.
INTRODUCTION
Drug allergy or drug hypersensitivity reactions (DHRs) consist of any harmful or unintended reactions to a drug that are known to occur at doses used for prevention, diagnosis, or treatment.1 DHRs or ‘adverse drug reactions’ are the terms often used interchangeably and essentially consist of adverse effects of drugs on the body which resemble allergic reactions in clinical practice. Drug allergies are specified adverse reactions, for which a definite immunological mechanism (either drug-specific antibody or T cell) is demonstrated.2 DHRs are common in clinical practice and reported in up to 15–25% of patients, with serious reactions occurring in 7–13% of these patients.3,4
DHRs are either predictable reactions that may occur in anyone (Type A) or unpredictable that will occur in only susceptible individuals (Type B). Unpredictable reactions are estimated to occur in approximately 20–25% of patients who experience DHRs,1,5,6 while drug allergy accounts for approximately 5–10% of all DHRs.7 Clinically, DHRs are classified as immediate types which typically occur within 1–6 hours after the last drug administration. They manifest in the form of urticaria, angioedema, rhinitis, conjunctivitis, bronchospasm, gastrointestinal symptoms (nausea, vomiting, diarrhoea, abdominal pain), anaphylaxis, and anaphylactic shock. Non-immediate DHRs occur as delayed onset urticaria, maculopapular type eruptions, fixed drug eruptions, vasculitis, toxic epidermal necrolysis (TEN), Stevens–Johnson syndrome (SJS), drug reaction with eosinophilia and systemic symptoms (DRESS), acute generalised exanthematous pustulosis, symmetrical drug-related intertriginous, and flexural exanthemas. In these reactions, internal organs can be affected either alone or with skin manifestations (DRESS, vasculitis) and include hepatitis, acute kidney injury and acute renal failure, pneumonitis, anaemia, neutropenia, and thrombocytopenia; they may occur as early as 1 hour after the initial drug administration.1 Predictable drug reactions are the most common type of DHR and are usually dose dependent and related to the known side effects, overdose, and drug interactions. Unpredictable reactions occur in an estimate of 20–25% of patients who experience DHRs; generally, these reactions are not related to the pharmacologic actions of the drug.1,5,6
Drug allergy is classified by the Gell and Coombs classification of human hypersensitivity, illustrated in Table 1 below.2 This classification system consists of immediate-type reactions (immunoglobulin [Ig]-E mediated), cytotoxic reactions (IgG/M-mediated), immune complex reactions, and delayed-type hypersensitivity reactions (cellular immune-mediated).8-10
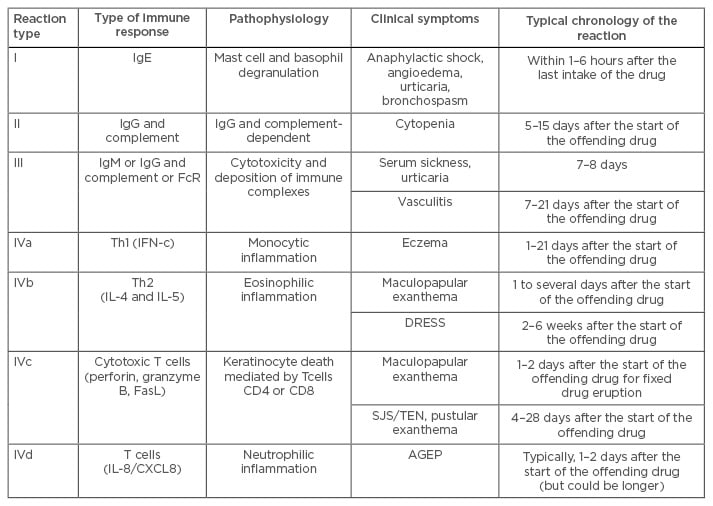
Table 1: Classification of drug allergies.
Ig: immunoglobulin; FcR: fc receptor; FasL: fas ligand; SJS: Stevens–Johnson syndrome; Th1: T helper Type 1; Th2: T helper Type 2; DRESS: drug reaction with eosinophilia and systemic symptoms; TEN: toxic epidermal necrolysis; IFN-c: interferon-c; IL: interleukin; AGEP: acute generalised exanthematous pustulosis.
The pharmacologic interaction with immune receptors (‘p-i concept’) has also been proposed in addition to drug hypersensitivity classification. In this p-i concept scheme, a drug binds non-covalently to a T cell receptor.
This leads to an immune response via interaction with a major histocompatibility receptor, however no sensitisation is involved because the stimulation of memory and effector T cells happens directly, which is similar to the concept of superantigens.4,5
Unlike immune-mediated drug reactions, pseudoallergic reactions are not associated with the production of antibodies or sensitised T cells, but are often clinically indistinguishable from DHRs. Non-steroidal anti-inflammatory drugs (NSAIDs), and angiotensin-converting enzyme inhibitors are common causes of these non-allergic reactions.6,11,12
RISK FACTORS
An increased risk of developing a drug allergy is associated with host factors (e.g. age, gender, genetic polymorphisms, certain viral infections) and drug-related factors (e.g. frequency of exposure, route of administration, molecular weight). Drug allergy commonly occurs in young and middle-aged adults, and is more often found in women than men. Human leukocyte antigen, HIV, and the Epstein–Barr virus have also been linked to increased risk of building immunologic response and reactions to drugs. Genetic polymorphisms in drug metabolism influence susceptibility to drug allergy. Drug administration via topical, intramuscular, and intravenous methods are more likely to cause allergic drug reactions than oral administration while intravenous administration is associated with more severe reactions. Prolonged high doses or frequent use of drug are more likely to develop hypersensitivity reactions than a single large dose. In addition, large macromolecular drugs (e.g. insulin or horse antisera) or drugs that form haptens (bind to tissue or blood proteins and elicit an immune response), such as penicillin, are also associated with a greater likelihood of causing hypersensitivity reactions.6,8,13-16
Diagnosis
A thorough history and identification of clinical signs and symptoms that are compatible with drug-induced allergic reactions form the main diagnostic method. Diagnostic tests include skin testing and if warranted, graded challenges, as well as the induction of drug tolerance procedures which are advocated on the basis of history and physical examination results. A history should include details of all prescription and over-the-counter drugs taken by the patient. It is often rewarding to know the dates of drug intake, formulation of the drug(s) taken, dosage, and route of drug intake. Clinical symptoms and signs developed with their timing and duration in relation to drug intake, as well as previous drug exposures and reactions, are also recorded.1,5,7,16 A thorough and careful physical examination can help to define possible mechanisms underlying the reaction and guide subsequent investigations and diagnostic testing. The most common clinical manifestations of drug allergy are seen on the skin1,7,12 and sometimes mucous membranes.
The most common cutaneous manifestation is generalised exanthema (as a maculopapular rash), which appears between a few days and 3 weeks after drug exposure, usually starting on the trunk and eventually spreading to the limbs. Urticaria and angioedema that result from both IgE-mediated and non-IgE-mediated mechanisms are also common. SJS and TEN are the most severe forms of drug reactions. SJS usually begins with a maculopapular rash that often progresses to bullae, mucous membrane ulcerations, conjunctivitis, fever, sore throat, and fatigue. TEN is a rare condition with similarity to SJS, however TEN causes a large portion of the epidermis to denude from the layers below, leading to extensive skin sloughing and a scalded skin appearance. The most common culprit for SJS and TEN are sulphonamides and as such should be avoided by the patient in the future.1 Since the clinical manifestations of drug allergy are mostly variable, it is necessary to exclude other conditions that can mimic drug-induced allergic reactions. Table 2 shows conditions in the differential diagnosis of drug allergy.6
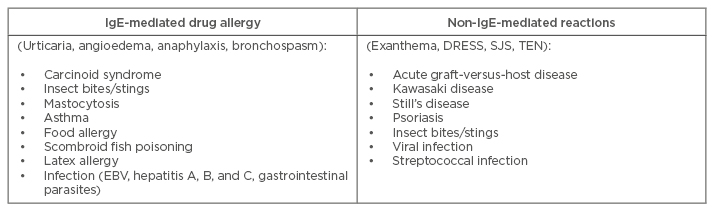
Table 2: Differential diagnosis of drug allergy and a list of conditions to consider.
IgE: immunoglobulin E; EBV: Epstein–Barr virus; SJS: Stevens–Johnson syndrome; TEN: toxic epidermal necrolysis; DRESS: drug rash with eosinophilia and systemic symptoms.
DIAGNOSTIC TESTS
IgE-mediated (Type I) reactions can be diagnosed by diagnostic procedures such as skin-prick testing and intradermal injection of the allergen. Skin testing guidelines are standardised for penicillin. The usefulness of skin tests for local anaesthetic muscle relaxants are limited due to negative results being more frequent, but they are very sensitive for insulin or monoclonal antibodies. On the contrary, a negative test result is useful for ruling out penicillin allergy and high molecular weight proteins, although it does not exclusively rule out the presence of a specific allergen. Serum-specific IgE tests are available for some drugs and are often expensive and less sensitive than skin tests. It is necessary to remember that most of these in vitro tests are not optimally validated for drug allergy testing.1,16
Patch testing involves placing the allergen (at non-irritant concentrations) on the patient’s back for 48 hours and then assessing any reactions. This type of testing is useful for the diagnosis of various delayed (Type IV) skin reactions, but is often not helpful for the diagnosis of SJS or TEN.11,12,16,17 The measurement of histamine and tryptase levels in the blood have been useful in confirming acute IgE-mediated reactions, particularly anaphylaxis; however, negative results do not necessarily rule out acute allergic reactions. Haemolytic anaemia may also be confirmed with a positive direct and/or indirect Coombs test.1,12,16
The potential role of the basophil activation test (the quantification of basophil activation by flow cytometry) in the diagnosis of drug allergy has been recently studied because basophils are involved in both immune-mediated and non-immune-mediated reactions. Although some evidence suggests that the test is useful for evaluating possible allergies to β-lactam antibiotics, NSAIDs, and muscle relaxants, further confirmatory studies are needed before it is widely accepted as a diagnostic tool.1,18,19
MANAGEMENT OF COMMON DRUG ALLERGIES
The most effective strategy is to avoid or discontinue the offending drug. If an alternative medication is available (with unrelated chemical structures), cross-reactivity among drugs should be taken into consideration when substituting the agent.1,12 Additional therapies, for example topical corticosteroids and oral antihistamines, may improve cutaneous symptoms. In the event of anaphylaxis, adrenaline is administered by intramuscular injection into the lateral thigh. Systemic corticosteroids are normally used to treat severe systemic reactions but should not be given prior to or as a substitute to adrenaline in the treatment of anaphylaxis.
Prevention of Future Reactions
Prevention of future reactions is an important part of patient management. Allergy bracelets/necklaces should be considered, particularly if the patient has a history of severe forms of drug-induced allergic reactions.16 Procedures to induce drug tolerance are expected to modify a patient’s immunologic or non-immunologic response to a drug temporarily, through the administration of incremental doses of the drug. Most regimens begin with a very dilute concentration of the drug, then the dose is increased every 15–20 minutes or so, usually with double the dosage until a full therapeutic dose has been administered after 3–8 hours. Drug tolerance-induction procedures and graded challenges are potentially harmful and should only be performed by experienced personnel in facilities with resuscitative equipment readily available.1,20
SPECIFIC DRUG REACTIONS
Acetylsalicylic Acid and Non-Steroidal Anti-Inflammatory Drugs
Acetylsalicylic acid (ASA) and NSAIDs can cause urticaria, angioedema, and anaphylaxis. Patients suffering from chronic airway diseases such as asthma, rhinitis, and sinusitis, may react to ASA and NSAIDs that inhibit cyclo-oxygenase (COX)-1. The management of these patients involves avoidance of aspirin and NSAIDs, as well as aggressive treatment of the underlying respiratory disorder. Selective COX-2 inhibitors almost never cause reactions and can typically be taken safely by patients with ASA/NSAID allergy.
Sulphonamides
Sulphonamide antibiotics are often associated with delayed cutaneous maculopapular eruptions, SJS, and TEN. Patients infected with HIV are at increased risk of developing cutaneous reactions to sulphonamide antibiotics. Trimethoprim-sulfamethoxazole is the drug of choice for the treatment of a number of HIV-associated infections, therefore many HIV-positive patients with a history of adverse reactions to sulphonamides still require treatment with this antibiotic. Induction of drug tolerance procedures can be used to safely administer trimethoprim-sulfamethoxazole to HIV-positive patients with a history of adverse reactions to the antibiotic.
Penicillin
Penicillin is the most frequent drug allergy, affecting approximately 10% of patients. Ideally, management of the patient with penicillin allergy should include penicillin skin testing. Approximately 90% of patients have negative penicillin skin test responses and can safely receive cephalosporins as well as other β-lactam agents. Carbapenems may be administered as a graded challenge after prophylactic skin tests.21,22 Monobactams are generally well-tolerated by patients with penicillin allergy, except if they have had an allergic reaction to ceftazidime.23-25 Second or third-generation cephalosporins may also be considered, since the degree of cross-reactivity with these agents and penicillin has been shown to be lower than with first-generation agents.1,26
Cephalosporins
Cephalosporins can commonly cause maculopapular rashes and drug fever; urticaria is less common and anaphylaxis is rarely seen.26 In subjects with cephalosporin allergy, there is limited cross-reactivity on immunological testing between second and third-generation cephalosporins and penicillins, but this does not necessarily indicate clinical reactivity.26 If skin testing is positive and no alternative drug exists, induction of drug tolerance procedures may be attempted.1,7
Radiocontrast Media
Pseudoallergic and allergic reactions to radiocontrast media can usually be prevented through the use of pre-treatment with medication, which includes oral corticosteroids and H1-antihistamines. Agents with low osmolarity are better for use in such circumstances.1,7
Anaesthetics
True allergic reactions to local or general anaesthetics are very rare; reactions are usually due to preservatives in the medication or due to adrenaline. Allergy to inhaled anaesthetics is not reported in the current literature.27
Vaccines
The seasonal flu vaccine or yellow fever vaccine may contain small quantities of egg protein, for which allergic response may be evoked.
CONCLUSIONS
Diagnosis relies on a meticulous history and physical examination. Skin testing, and if warranted graded challenges of allergen, and induction of drug tolerance procedures may be required in some instances. The mainstay of treatment for drug allergy is avoidance of the offending drug. When available, alternative medications with unrelated chemical structures should be substituted. Cross-reactivity among drugs should be taken into consideration when choosing alternative medications. If a particular drug to which the patient is allergic is indicated and there is no suitable alternative, procedures of induction of drug tolerance may be considered for producing temporary tolerance to the drug.






