BACKGROUND
There is evidence of a positive association between asthma and obesity in children.1 Perinatal probiotic supplementation has been shown to be effective in the primary prevention of atopic dermatitis (AD), although the long-term effects of probiotics on AD and allergic asthma is less certain. Many reports suggest that certain probiotic strains also have potent immunomodulatory activity in allergic asthma. However, the underlying mechanism of action is still unclear.2,3 Recent evidence suggests that gut microbiota are involved in the control of body weight and inflammation, and thus play a role in the pathophysiology of obesity.4 The association between the gut microbiota and obesity in children is not fully studied.
AIM
The aim of this study was to evaluate the efficacy of probiotic micro-organism Lactobacillus reuteri DSM 17938 (LR) in the prevention of the development of asthma and AD in obese, 7-year-old
Slovenian children.
MATERIALS AND METHODS
This prospective study included 904 maturely born children. All enrolled children were exclusively breastfed for ≥4 months. After the fourth month the same dietary intake for the child was recommended to all parents. A total of 238 children were breastfed with the addition of LR from the age of 4 weeks for 16 weeks. Every child was followed up by the same paediatrician until they were 7 years old. At the age of 7 years they were divided into groups: group A comprised 712 children with BMI <95 percentile, and group B comprised 192 children with BMI >95 percentile for age and sex. According to the addition of LR, diet group B was divided into subgroups: Bx contained 107 children exclusively breastfed for 4–6 months, and By contained 85 children breastfed with addition of LR. The prevalence of doctor’s diagnosed asthma and atopic dermatitis at the age of 7 years, asthma course, and episodes of wheezing (lasting up to 5 days) in the first 5 years of life were observed. Allergic aetiology of asthma and AD was confirmed with specific IgE testing and positive skin prick tests performed by a physician who was unaware of the child’s group allocation. Statistical analysis was performed with a PC using chi-square analysis with Yates’ correction. p-values <0.01 were considered significant.
RESULTS
In the study group, 10.4% of children had positive history of parental allergy, 10.4% had asthma, and 8.9% had AD. There was no significant difference between groups in the percentage of children with positive history of parental allergy (p>0.50). The prevalence of asthma (A: 7.6%; B: 20.8%) and AD (A: 6.2%; B: 19.8%) were significantly higher in obese children (group B), (p<0.001). No significance between group difference in prevalence of wheezing was confirmed (A: 16.7%; B: 25%), (p>0.01). The authors observed significantly lower prevalence of wheezing (Bx: 32.7%; By: 15.3%) and asthma (Bx: 28.0%; By: 11.8%) in the subgroup By (p<0.01). The prevalence of AD in this subgroup also tended to be lower (Bx: 26.2; By: 10.6%), (p=0.018). There was also a lower frequency and shorter duration of asthma attacks observed in subgroup By. No significant difference between subgroups in percentage of hospitalised children was observed, but frequency of hospitalisation was significantly lower in subgroup By (Figure 1).
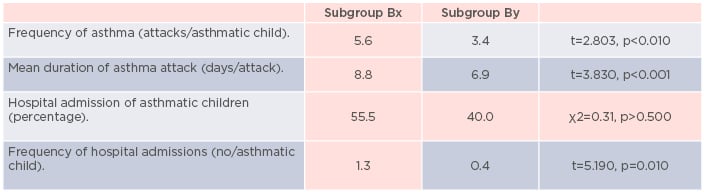
Figure 1: Data about frequency and episode duration and percentage of hospitalisations in each subgroup.
CONCLUSIONS
The authors demonstrated that the addition of LR to early child’s diet has a preventive effect on asthma and AD development in obese children. It also has a strong beneficial impact on the
asthma course.






