Assessing adherence to inhaled medication remains a challenge in clinical practice. Self-reports, although subjective, are still considered one of the preferred methods as they are simple, cheap, and minimally intrusive.1,2 However, subjective methods may generate patient–physician discordance and impair the identification of patients with poor adherence. In turn, this might influence patient satisfaction, and compromise shared decision-making and therapeutic adjustments.3 Evidence is lacking on the degree and characteristics of discordance between patients and physicians in relation to the assessment of inhaled medication adherence, but this knowledge is essential to delineate effective strategies to maximise patient–physician agreement and improve clinical decisions. Therefore, this study was conducted to compare patient and physician assessments of inhaled medication adherence and to identify predictors of patient–physician discordance.
Adults and adolescents (≥13 years) with persistent asthma were recruited at 29 allergy, pulmonology, and paediatric secondary care outpatient clinics in Portugal, in the context of two observational prospective studies of the INSPIRERS project. This project addresses the topic of adherence to asthma inhalers among adolescents and adults with persistent asthma. Patients and physicians independently rated adherence to inhaled medication during the previous week, using a 100 mm visual analogue scale (VAS).4 Demographic and anthropometric characteristics, patients’ follow-up time, asthma characteristics and control according to Global Initiative for Asthma (GINA),5 and details of current treatment were collected. VAS scores and categories (low: 0–50, medium: 51–80, and high: 81–100) were used in the analyses. The cut-offs of 50% and 80% are frequently used for
differentiation of adherence groups.6,7 Discordance was defined as VAS scores difference (VAS-d)≥10 mm or classification in distinct categories. Correlations with Spearman’s rho (rs) were used to explore the association between patients’ and physicians’ VAS scores and Cohen’s kappa to determine the agreement between categories. Multivariable logistic regression analysis was used to identify predictors of discordance (VAS-d≥10mm).
A total of 395 patients (61% female; 68% adults), with a median age (percentile 25 to percentile 75) of 28 years (16–46) years were analysed. According to the GINA classification, nearly half of participants had their asthma poorly controlled (n=184; 47%). Inhaler adherence was rated as high, both by patients (median: 85 mm [65–95 mm]) and physicians (median: 84 mm
[68–95 mm]; p=0.707), with a median VAS-d of 10 mm (4–20). Correlation between patient and physician VAS scores was moderate (rs=0.58; p<0.001) (Figure 1). Using VAS-d≥10 mm, patients and physicians disagreed in 53% of cases (n=211), with physicians overestimating adherence in 26% (n=102) of cases and underestimating it in 27% (n=109). Using VAS categories, disagreement occurred in 36% of cases (kappa 0.4; 95% confidence interval [CI]: 0.32–0.48), with physicians overestimating adherence in 17% (n=66) of cases and underestimating in 19% (n=76). Absence of asthma control (odds ratio [OR]: 3.05; 95% CI: 1.59–5.89) and short-acting β2-agonist prescription (OR: 2.69; 95% CI: 1.22–5.92) were associated with increased discordance, while having a written asthma action plan (OR: 0.38; 95% CI: 0.20–0.74) and hospital admissions in the past year (OR: 0.13; 95% CI: 0.03–0.52) were associated with reduced discordance. This model explained 20% of the variance in patient–physician discordance and correctly classified 63% of cases.
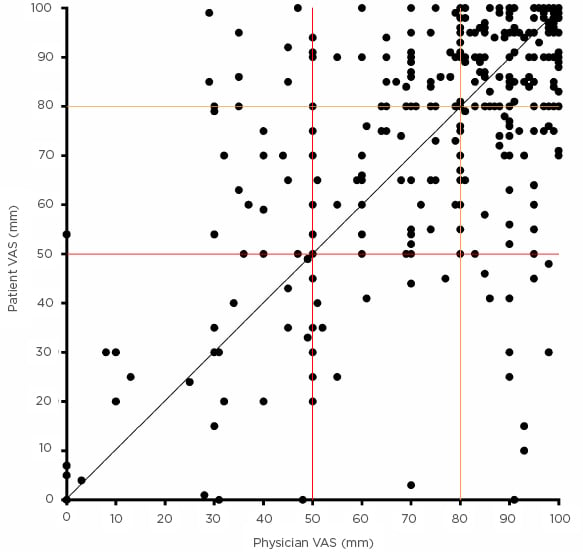
Figure 1: Scatter plot showing the relationship between patient and physicians estimates of inhaler adherence (N=395).
The black line represents perfect agreement; the red and orange lines represents the cut-offs of 50 and 80. In 40% of cases both patients and physicians classified adherence to inhaler treatments in the previous week as >80% in 15% of cases between 51–80%, and in 9% of cases <50%.
In conclusion, patients’ and physicians’ assessment of inhaler adherence were discordant in more than one third of cases and were only moderately correlated. These results highlight the shortcomings of global subjective measures of inhaler adherence. Implementation of objective adherence measures and effective communication are needed to improve patient–physician agreement. This study has also identified some predictors that can help to improve
understanding of this discordance.






