INTRODUCTION
Hereditary alpha-tryptasaemia (HAT) affects 4–6% of the population and is caused by allelic replications tandem duplications of the alpha-tryptase encoding sequencing of the TPSAB1 gene. It is typically associated with allergic-type skin and bowel symptoms, cardiovascular symptoms, and non-specific systemic symptoms. Generalised aches and pains are common, as is joint hypermobility; however, bone abnormalities have not been previously described. Bone abnormalities associated with HAT are described in this clinical case report.
CASE DESCRIPTION
This 57-year-old female presented with numbness in her feet and intermittent bony pains at the age of 53. Her past medical history included: i) a previous reaction to oxytetracycline (skin rash), ii) a reaction to salmon (lip swelling and vomiting), and iii) a collapse episode, for which all investigations at the time were unremarkable. Investigations for the numbness in her feet and intermittent bony pains included pelvic MRI and nuclear medicine scans (Figure 1). These showed multiple sclerotic bony lesions in her pelvis, for which she was issued with zoledronic acid that resulted in a partial symptomatic response.
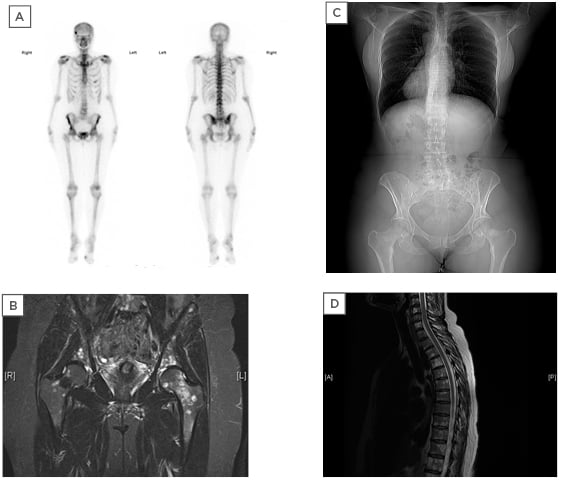
Figure 1: A) TcMDP bone scan showing areas of increased activity; B) MRI-coronal section of the pelvis; C) CT scan showing sclerotic bones; D) MRI sagittal section of the spine showing multiple bony lesions.
In addition to the bony lesions, she had experienced multiple episodes of urticarial rashes and flushes that responded to antihistamines, gastrointestinal symptoms in the form of indigestion, nausea, vomiting with no diarrhoea and which responded to regular ranitidine, and a few episodes of palpitations; however, haemodynamically she was stable and no treatment had been required for this so far.
Due to the widespread appearance of sclerotic lesions in the bone, she had undergone thorough assessment by the Manchester University NHS Foundation Haematology team, including bone marrow trephine biopsies twice which excluded malignancy. These however showed an increased number of non-spindle-shaped CD2-mast cell aggregates in the patient that accounted for approximately 15% of the total cellularity. Her baseline mast cell tryptase (MCT) was between 17.0 and 19.8 ug/L. C-KIT mutation screening was negative. Due to persistently raised serum MCT concentration, she was
assessed for the recently described increase in copy number of the TPSAB1 gene encoding alpha-tryptase, which is associated with an increase in basal serum tryptase levels in patients presenting with multisystem complaints.1 A tandem duplication of the alpha-tryptase encoding sequencing of the TPSAB1 duplication gene was identified in this patient by droplet digital PCR, performed at the Manchester Centre for Genomic Medicine, Manchester, UK.
DISCUSSION
Lyons et al.1 have described two large patient cohorts with elevated basal serum tryptase levels that were exclusively associated with increased copy numbers of the alpha-tryptase-encoding sequence of TPSAB1, caused by tandem duplications within the gene. Affected individuals reported multiple symptom complexes such as irritable bowel syndrome, cutaneous manifestations, connective tissue abnormalities, and dysautonomia.
Recently, there have been more patient cohorts with similar clinical phenotypes described and found to be associated with elevated basal MCT levels.2,3
Affected individuals had described various symptoms, including those often described as ‘functional’ symptoms, i.e., when all investigations have not revealed a pathological cause for their symptoms. The most common symptoms were:
> Gastrointestinal complaints, particularly irritable bowel syndrome and chronic gastroesophageal reflux.3-5
> Connective tissue disorders, congenital skeletal abnormalities, and retained primary dentition.6 Interestingly, the patient presented with multiple sclerotic bony lesions and bone aches rather than the above described skeletal abnormalities.
> Autonomic dysfunction, including postural orthostatic tachycardia syndrome.1
> Recurrent cutaneous flushing and pruritus, which in some cases associated with urticaria and was concomitant with complaints of sleep disruption.1
> Systemic reaction to stinging insects such as Hymenoptera7,8 was increased by 2–3-fold compared to the frequency of such reactions in the general population.8
CONCLUSIONS
This case highlights that bony abnormalities may be associated with HAT. Further studies are required to substantiate this potential association.






