Words by Michaila Byrne
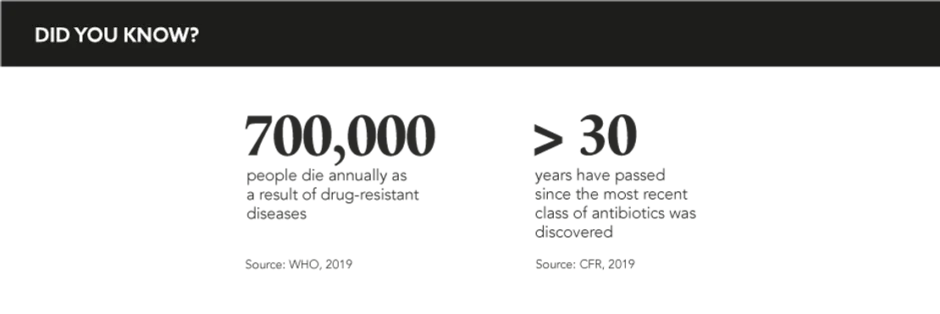
In the century since Alexander Fleming’s eureka moment, antibiotics have reigned as one of mankind’s proudest achievements: a wonder drug that fights infection, saves lives, and even wins wars. But as we navigate the present ‘era of abuses’ with the threat of superbugs looming and few new antibiotics on the horizon, how can the pharmaceutical industry and, in particular, medical affairs teams, take heed of Fleming’s warnings and urgently action optimistic, pragmatic approaches to combat and curb antimicrobial resistance (AMR)?
Historically, pharma has shone as a formidable force in antibiotic development, playing a key role in the recovery and survival of millions. But as the years have passed, the industry has become less active in this arena causing an extreme drought in new antibiotics, which combined with poor adherence and habitual over-dependence, has culminated in a perfect storm: “Despite the growing threat of AMR and widespread recognition of the need for new antibiotics, the number of companies conducting antibiotic R&D has significantly declined due to scientific, regulatory, and economic challenges,” explains Dr Elizabeth Hermsen, Head of Global Antimicrobial Stewardship, MSD (known as Merck & Co., Inc. in the US and Canada). Despite how indomitable the challenge may first appear, the industry must take note of the disruptive impact of COVID-19 and adopt this experience as a cautionary tale. “The next pandemic could be caused by a drug-resistant pathogen and it is far too costly on all accounts to develop a treatment on short notice,” warns Fatema Rafiqi, Research Programme Manager, Access to Medicine Foundation.
MA have a leading part to play in raising the alarm and communicating the need for strong education, awareness, and stewardship programmes. AMR is a complicated topic, too often poorly understood; however, with their foundational training in science and medicine, MA can prioritise not only patient needs, but also uphold public health interests. Hermsen corroborates: “MA professionals have a large network to facilitate best practice sharing and, as such, they understand different perspectives from various geographies, providers, and/or practice settings. With their expertise and capabilities in infectious diseases, MA professionals can clearly complement other stakeholders in efforts to address AMR.” MA can compensate for knowledge gaps and build bridges between multiple stakeholders who all have their own unique part to play. “MA serve as trusted communicators with external stakeholders, such as key opinion leaders, healthcare professionals, policy makers, government officials, and patients,” says Bruce Altevogt, Vice President and Head of External Medical Engagement, Hospital Business Unit, Pfizer.
Plainly put, the current financial ecosystem is unsustainable, and the antibiotic pipeline is not accelerating at the rate necessary for innovation to flourish. Rafiqi explains that support and funding are essential: “A viable economic environment is important as well as more partnering opportunities and policy reform.” Pharma must create better incentives and a viable economic environment for antibiotics to not only survive but prosper. Altevogt attributes additional reasons for a lack of innovation to the “steep costs of antibiotic development, high risk of failure, long lead times, and growing awareness of the need to limit their use,” explaining that “there are few incentives for venture capital or pharmaceutical companies to invest in antibiotic R&D since it will be extremely difficult to realise a return.”
A viable economic environment is important as well as more partnering opportunities and policy reform
But the industry is showing signs of heading in the right direction. Earlier this year, the AMR Action Fund was formed, with pharma companies collectively donating £1 billion in a push for innovation in late-stage development. Furthermore, ‘push and pull’ incentives have been introduced to support younger companies, who have the ideas but lack the funding to develop new antibiotic drugs. In this way, big pharma can support the creation of antibiotics by partnering with these ambitious biotech companies through covering the operational and commercialisation costs. This two-pronged solution helps to stop more prominent drug makers from retreating, prevents smaller biotechs from going bankrupt, and saves the lives of patients: a collective win by all accounts.
It is easy to forget that until very recently, patients routinely succumbed to common but treatable infections. We cannot regress and undermine the incredible progress that has been made; pharma needs to reclaim its position and become part of the solution. As the COVID-19 pandemic has proven, mobilisation is possible and political willingness for acceleration is here. AMR is humanity’s slower-moving pandemic, so combatting it is a medical imperative as well as an ethical one and MA has the chance to take the reins for real change.