There are many key pillars of medical affairs, but field teams are where the action happens. The question is: how do you build teams that deliver results by truly connecting with KOLs?
Words by Isabel O’Brien
In today’s dynamic pharmaceutical landscape, medical affairs (MA) leaders have plenty on their proverbial plate. From refining engagement strategies to navigating regulatory complexities, success increasingly hinges on how effectively field medical teams connect with key opinion leaders (KOLs). But what sets the standout teams apart? And how do organisations break through today’s barriers while readying for whatever’s next?
What makes a successful field medical team?
In the 2024 edition of ZS’s ‘Medical Affairs Outlook Report’, only 19% of companies described their medical affairs function as best in class. While this number is up 6% from 2023, it’s clear that most MA organisations are not operating at full throttle.
“Successful field medical teams are highly agile and productive. They are also very close to the true needs of the KOL,” says Sunil John, Principal, ZS. “This leads to them being able to personalise their engagement while delivering at scale. To do this well, they must have access to good data—this foundation will help them understand the needs of their stakeholders, avoiding the one-size-fits-all approach,” adds his colleague Sarah Jarvis, also a Principal at ZS.
The ZS study, authored by John and co-authored by Jarvis, highlights that a successful field medical team must know more than just a KOL’s preferred contact method or favourite topic. Instead, success can depend on using insights to create bespoke engagement strategies, starting with tailoring the timing of interactions.
According to the research, as many as 82% of KOLs prefer MSL interactions to begin pre-launch, with the majority wanting to engage at Phase III. This is an important point to note, as if KOLs must wait a stage later than they prefer, the opportunity to effectively advance and disseminate scientific knowledge is significantly reduced. This is because they have less time to integrate and adopt the therapy into their clinical practice.
Striking at the right time, however, is only one component. John highlights that in-depth yet pithy scientific exchange is critical when engaging with KOLs. “They value MSLs who are reliable and credible sources of information, knowledgeable about disease states and respectful of their time.” There is a balance to strike between scientific rigour and concise communication, and not all field teams are nailing that mix currently.
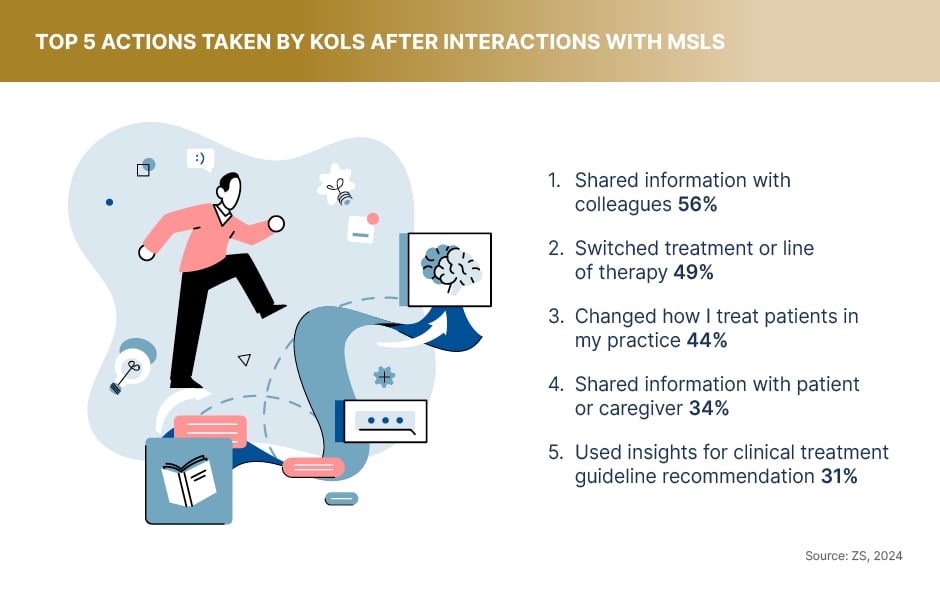
Nevertheless, the Outlook Report reveals that MSL interactions drive significant KOL actions. On average, a KOL takes three to four actions following an MSL interaction, with 56% sharing information with colleagues and nearly half switching a treatment or line of therapy. These findings demonstrate the pivotal role MSLs play in influencing clinical decision-making and why it’s a key part of the medical affairs puzzle to get right.
“It is important that medical teams are scientific partners of choice,” says Jarvis. “This is something that can be driven by the field teams as they are up front and centre with the end stakeholders.”

What challenges does pharma face?
Despite their success, field medical teams face significant barriers to engaging KOLs. Understanding and addressing these hurdles is critical to becoming best in class.
To start, field teams often grapple with access to high-quality data. “Improving efficiency and productivity requires data that can be utilised by MSLs to fine-tune their engagements,” says Jarvis. “However, getting this data to MSLs in a digestible format is difficult; data is structured and unstructured and sometimes not even captured reliably.” The inconsistency makes it challenging for MSLs to learn what’s working, what isn’t and improve their approach in the future.
Technology and AI are starting to ease these pressures. Investments in digital tools enable faster access to relevant data, allowing MSLs to personalise their engagements and increase their value to stakeholders. “However, many are still over-reliant on MSLs ‘figuring out’ all of this information on their own,” Jarvis notes.
The greatest challenge
Another pressing issue is access to KOLs. Regulatory and institutional constraints, coupled with limited KOL availability, make winning face time difficult. The ZS medical affairs report supports this challenge, with 52% of medical affairs professionals citing KOL inaccessibility as their greatest obstacle. This is supported by KOLs, who also cite limited availability for engagements as the primary reason for low access with MSLs.
To secure meetings and build relationships, John explains that “MSLs must consistently demonstrate expertise and provide value by delivering unbiased, tailored scientific information”. Individual and corporate reputation is key to long-term partnership. Meanwhile, 78% of KOLs prefer a hybrid engagement model combining in-person and virtual meetings, states the research, underscoring the need for flexibility and strategic planning from MA.
Speaking on behalf of her own medical affairs organisation, Dr Harmony Garges, Senior Vice President, Chief Medical Officer, and Head of Global Medical, ViiV Healthcare, offers her perspective on the challenges faced by field teams trying to reach KOLs. “Currently, the number of KOLs we can engage with is limited by the size of the medical field team and the geographical spread of our KOLs.” Offering a potential solution, she notes that “increasing our numbers would allow for even more engagements, both with established KOLs and allow us to expand our medical audience”.
This strategy resonates across the industry. According to the ZS research, 87% of the medical affairs leaders who provided the split for field medical investments indicated that the biggest area of investment is expected to be in people for additional resourcing, upskilling and training.
Delivering measurable impact
Successful field teams balance engagement quantity with quality—but how can they effectively measure the outcomes of these interactions?
While Dr Garges says that typical metrics such as the number of engagements per month, the balance between face-to-face and virtual interactions and total physician reach are important, she adds that ViiV also assesses the quality of those engagements based on the depth of their engagement plans. “Ultimately, we evaluate the impact by looking at how these interactions translate into changes in clinical practice and patient outcomes. However, we acknowledge that there is always room for improvement,” she says.
Field teams that link insights from MSL-KOL interactions to broader strategic objectives improve not only internal processes but also healthcare outcomes. Dr Garges underscores the need for continuous improvement: “We are committed to refining our measurement strategies to better capture the impact of our interactions on healthcare practices.”
According to the ZS study, organisations using data-driven engagement strategies are better positioned for success. However, only 46% of surveyed companies have implemented a centralised data and analytics hub, highlighting a critical area for growth.
Preparing for future trends
As the healthcare environment shifts, field medical teams must adapt to stay relevant. “The stakeholder universe that field medical teams need to engage continues to grow with newer stakeholders,” says Jarvis. For example, primary care providers, nurse practitioners, patient advocacy groups and others are coming into the fold, she says. “We see this as the third era of medical affairs; where field medical and internal medical affairs have to be able to operate at scale.”
To enter this new phase, field teams will have to harness digital tools to offer flexibility and value-based care discussions, focusing on broadly relevant topics such as patient outcomes, cost-effectiveness and health equity, note Jarvis and John.
Interactive content formats, such as those offered by EMJ, could also be valuable tools for MSLs to share, allowing KOLs to explore content at their own pace and focus on the parts that interest them. In addition, enhanced data capture and analysis will be essential for informing decision-making and driving personalised engagement strategies.
As Dr Garges explains: “To remain relevant, field medical teams must enhance their capabilities to strategically deliver value by focusing on the specific priorities and needs of KOLs.” Providing customisable experience must be top of mind at all junctures.
Final word
Field medical teams sit at the intersection of data, education and real-world relationships, and with 81% of companies not yet identifying their teams as best in class, the majority have room to grow.
Addressing MSLs directly, John wraps up his thoughts: “It is important to focus on the key levers that lead to KOL delight and becoming an MSL that they want to talk to.” His advice? “To become an MSL of choice, you need to ensure that you are providing the right content via the right channel at the right time.”
By forging strategic partnerships, embracing technology and growing internal teams, field medical teams can cultivate the trust and credibility needed to excel. Their future success will hinge on mastering personalised engagement, overcoming access barriers and staying ahead of evolving industry trends.









