Words by Michaila Byrne
If the horse meat scandal of 2013 taught us anything, it was that consumers have a right to know exactly what they are buying, and manufacturers have an ethical duty to be 100% transparent. Labelling is the vessel through which vital instructions and information about products are communicated to end-users, and in the pharmaceutical industry, medical affairs are entrusted with safeguarding these products from misuse, by balancing scientific accuracy with conciseness and coherence.
“Good labelling skills are a form of art that combines regulatory requirements and all scientific information into a focussed and clear label. Less is more when it comes to labelling wording,” says Isma Benattia, Vice President Europe Medical Affairs, Amgen. And with the stakes as high as they could possibly be, a drug simply ‘doing what it says on the tin’ is insufficient. Accuracy might sound like an obvious stipulation, but absolutely nothing can be left to chance.
A common error that can lead to mishaps is language barriers, so translations being conducted by native speakers is a necessity. When the Spanish Conquistador Hernán Cortés infamously landed in Mexico and met emperor Montezuma II, the absence of any present native speaking translators resulted in a historic misunderstanding, a fatal kidnapping, and the deaths of thousands of people. When it comes to medicine labelling, the consequences of miscommunication and meaning being ‘lost in translation’ can be equally fatal. Benattia continues: “Each leaflet must be written in the local language and translated by native speakers. For example, ‘every other week’ to native English speakers implies every 2 weeks, but to non-English speakers it could mean ‘occasionally’, and potentially cause confusion if translated without validation from native speakers.”
Clarity is everything, not just for patients. When a pharmacist scans a medicine shelf to select a bottle or a pill, there can be no room for error or confusion. “The system backing the product and the healthcare practitioner has to make it easy to do the right thing and difficult to do the wrong thing,” states Nancy Globus, Vice President, Regulatory Affairs, Accreditation Council for Medical Affairs. This is where MA can showcase their value, ensuring that something like a mismatch between a label and a dosing cup is an event of the highest improbability.
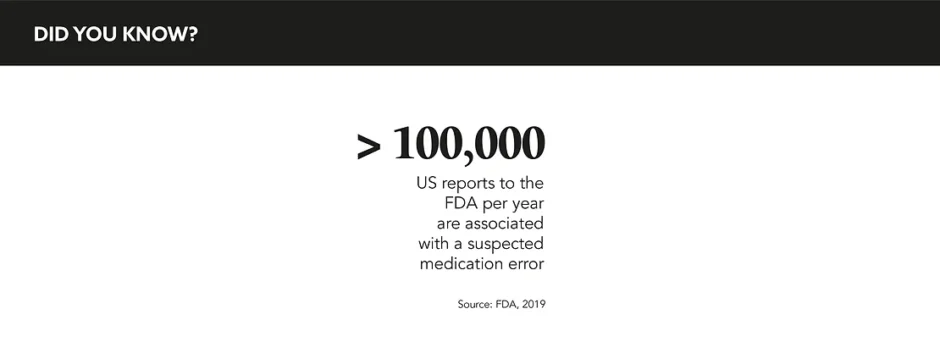
Aside from harm to patients, what is the cost of such errors? Rich Quelch, Global Head of Marketing, Origin Pharma Packaging, details pharma’s vested interest in labelling compliance: “Labelling inaccuracies also cost the pharma industry in lost revenue, slow the launch process, and result in product recalls. In fact, it is estimated that 50% of medicine recalls are due to errors in labelling or packaging artwork.” Benoit Lourde, Senior Business Development Manager, Intelligent Labels & Healthcare, Avery Dennison, outlines similar outcomes, with inaccurate labelling: “Affecting compliance, causing loss of inventory, and jeopardising patient safety.”
The unique skillset of MA professionals is tailor-made for detecting potential errors, taking a pre-emptive risk-based approach, and conjuring up preventative mitigation strategies. “Clearly accuracy is important, but it is putting those processes into place where there aren’t chinks in the armour of the system. You have to think about the types of errors that can occur,” says Globus. With their combination of medical expertise and ability to communicate complex information, MA has the potential to play a much bigger role in this space.
Fluctuating compliance standards, the global distribution of products, and the lack of rule uniformity across borders only complicates matters. Compensating for this, MA must understand the nuances of country-specific designs and become fluent in the regulatory requirements of each product. Quelch confirms: “The pharmaceutical industry is increasingly globalised and safety standards are strengthening, yet medicine labelling remains in a disconnected tangle with little consistency across markets, particularly amongst developing economies.”
Nonetheless, Globus is optimistic that if pharma can build labelling into the early product design stages, as well as make better use of experts operating regionally, these challenges can be overcome. She continues: “There are some global initiatives moving towards harmonisation of labelling across countries. Certainly, the overarching goal is that they want products to be used safely. For, as frustrating as those individual intricacies and differences are, there is definitely a move towards harmonisation that is worthy of recognition.” Lourde corroborates: “Using local knowledge on the compliance side and staying informed about changes and proposed changes to legislation can help MA professionals to meet compliance standards.”
As potent substances with a much greater risk impact than a product like horse meat, drugs and their labels need to be held to rigorous standards of scrutiny that far exceed accuracy. With increased education across functions around the risk factors at play, with the help of mandatory native translators, and through continued collaboration and training, MA can apply their already distinctively suited skillset to this vital aspect of drug development and safety.