SCIENTISTS based in the USA have uncovered a key mechanism explaining how mitochondrial defects contribute to the development of Type 2 diabetes, a condition that affects millions worldwide.
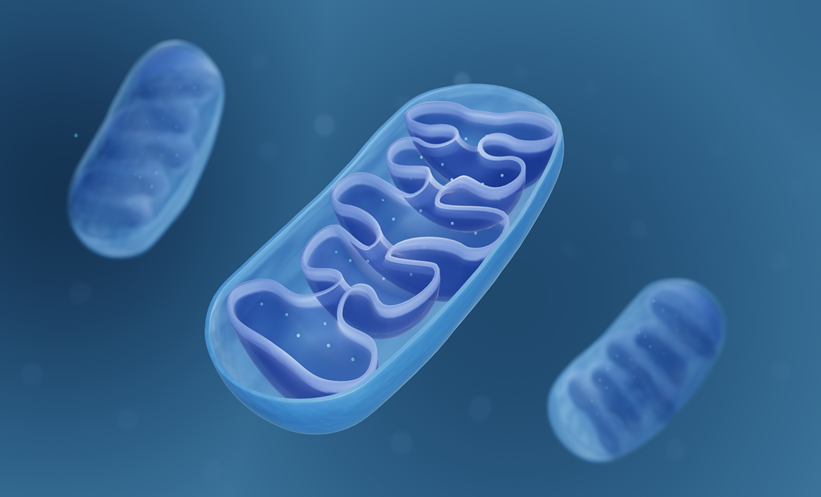
Mitochondria play a crucial role in generating the energy required for cellular function. However, defects in these energy-producing structures have long been associated with various diseases, including Type 2 diabetes. Patients with the disorder either do not produce enough insulin or cannot effectively use the insulin their pancreas produces, resulting in high blood sugar levels.
Previous studies have observed abnormal mitochondria in insulin-producing pancreatic β-cells of diabetic patients, but the reason behind this dysfunction remained unclear. Now, researchers have demonstrated that mitochondrial defects trigger a stress response that affects β-cell maturation and function.
“We wanted to determine which pathways are important for maintaining proper mitochondrial function,” said the study’s authors.
To investigate, the team used mice and disrupted three key mitochondrial components: their DNA, a pathway responsible for removing damaged mitochondria, and another that maintains a healthy mitochondrial population within cells.
“In all three cases, the exact same stress response was turned on, which caused β-cells to become immature, stop making enough insulin, and essentially stop functioning as β-cells,” the authors explained.
Further confirming their findings, the researchers observed the same effects in human pancreatic islet cells. The discovery led the team to investigate whether the stress response extended beyond pancreatic cells. Given that diabetes affects multiple organ systems, they examined liver and fat-storing cells in mice and found similar mitochondrial dysfunction.
“Diabetes is a multi-system disease. You gain weight, your liver produces too much sugar, and your muscles are affected,” said the team.
Their experiments confirmed that mitochondrial stress hindered cell maturation and function in liver and fat cells, further supporting the idea that mitochondrial dysfunction plays a central role in diabetes progression.
Notably, the researchers discovered that mitochondrial damage did not lead to cell death, raising the possibility that reversing the damage could restore normal function. To test this, they administered ISRIB, a drug designed to block the stress response, to mice for four weeks. The results were promising: β-cells regained their ability to regulate glucose levels effectively.
“Losing your β-cells is the most direct path to developing Type 2 diabetes. Our study provides an explanation for what might be happening at the cellular level and how we could intervene to address the root cause,” researchers stated.
The team is now working to further dissect the disrupted cellular pathways and hopes to replicate their findings in diabetic patient samples. If successful, their research could pave the way for new therapeutic strategies aimed at reversing mitochondrial damage and restoring normal insulin function in patients with Type 2 diabetes.
Reference
Walker EM et al. Retrograde mitochondrial signaling governs the identity and maturity of metabolic tissues. Science. 2025;DOI:10.1126/science.adf2034.