Abstract
This case report presents an unusual clinical scenario where a patient experienced temporary paralysis of his lower limbs while driving, and thus was unable to maintain control of his vehicle which subsequently crashed. On admission to the hospital, the patient complained of chest pain from where they impacted with the steering wheel during the crash and lower back pain. CT scan revealed a fracture to vertebrae L1 and L2. Of note to this case report, on arrival, the patient’s serum potassium level was found to be grossly elevated at 9.5 mEq/L, which makes this case unusual as searching the literature showed that potassium higher than 9 mEq/L is incompatible with life, wheras this patient was still alive. With a background history of Type 1 diabetes and Addison’s disease, hyperkalaemia was deemed a complication of an Addisonian crisis that this patient had suffered during the road traffic accident. The patient was thoroughly assessed while admitted, spending several days in the intensive care unit before being moved to a medical ward. The hyperkalaemia was soon resolved over several days, and following adjustments to his medications, the patient made a full recovery and was discharged home. This case presents a unique opportunity to explore how an electrolyte disturbance, caused by an Addisonian crisis, can induce periodic paralysis, which in this case, caused the patient to be involved in a serious road traffic accident. While thankfully escaping significant injury, it highlights the importance of precise management of endocrine disorders where serious complications could occur.
Key Points
1. Hyperkalemic periodic paralysis, although rare, can be potentially fatal; and thus needs to be addressed early and promptly.
2. This is a case report of hyperkalemic periodic paralysis due to under treated Addison disease. It showed how serious such an episode is, leading to a near fatal road traffic accident. Although the patient is well educated about his disease and complications, and he also had previous episodes of hyperkalemic paralysis, his symptoms were very subtle and gradual, so he did not realise up to the moment his potassium level was checked in the resuscitation and came to be over 9.
3. Early recognition and management of adrenal disease and crisis is vital, and there is a need for adequate treatment and regular follow ups. This will prevent such dangerous episodes of hyperkalemic paralysis and other related complications.
INTRODUCTION
A pre-alert was received from ambulance control to the emergency department (ED) about a patient, a 52-year-old male, involved in a road traffic accident. The patient was a restrained driver going at about 100 km/hr (about 62.14 miles/hr). He was feeling fine while driving but when he went to press the brakes, he had no power in that leg. He was unable to press the brake as he approached a roundabout. In an effort to avoid the roundabout he veered off the road and stopped when he hit a tree.
Interestingly, when his blood tests were done in the ED it was found that his potassium (K) was 9.5 mEq/L. This, along with a background history from paramedics that the patient has Addison’s disease, made it highly probable that the patient was having Addisonian crisis that must have led to hyperkalaemic periodic paralysis, causing the accident (Figure 1).1,2
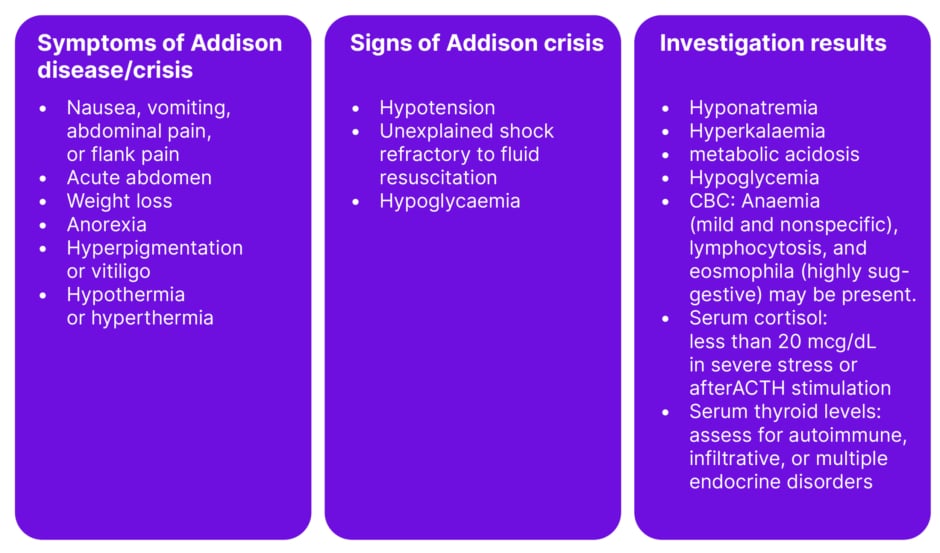
Figure 1: Clinical features and laboratory findings suggestive of an Addisonian crisis.
ACTH: adrenocorticotropic hormone; CBC: complete blood count.
Patient Information
The authors’ patient was a 52-year-old male with a long history of Addison’s disease, Type 1 diabetes, and chronic kidney disease.3 He had been maintained on a regular dose of steroids and fludrocortisone and had been followed up in another hospital. He had two previous admissions to that hospital relating to complications of his Addisions and diabetes. There was a question on his drug compliance raised in previous letters to the general practitioner and his endocrinology team. His diabetes control was moderate to good. He used the continuous glucose monitoring system, as his workplace was a building site. He required tight control as he was often up on scaffolding.
The authors’ primary concern was that the patient didn’t arrest as he had hyperkalaemic changes on the electrocardiogram (ECG) together with his injuries sustained from the trauma he had. His symptoms were generalised body weakness, with chest pain as he hit his chest against the steering wheel and lower back pain.
Clinical findings
At the time of presentation to the ED, the patient was managed in the resuscitation room based on his trauma. He was assessed and managed as per the trauma ABCD protocol for primary survey and also had his secondary survey. His blood tests were done as a part of the primary survey including venous blood gas that showed low pH of 7.21 (acidotic), HCO₃ of 12, Lactate of 0.8 mmol/L, pO2 of 16.4 Kpa on high flow oxygen, pCo2 of 3.4 Kpa, sodium of 126 mEq/L, and potassium of 9.5 mEq/L.
His ECG showed features of hyperkalaemia in the form of hyperacute T wave, prolonged PR interval of 0.28 ms, and left axis deviation (Figure 2). His sugars were high at 23 mmol/L, but his ketones were normal in the blood at 0.1 mmol/L. His urea and creatinine were also high confirming he had acute kidney injury on top of his chronic kidney disease, with results of 13.6 mmol/L and 304 umol/L, respectively, while his baseline urea was 8.8 mmol/L and creatinine was 212 umol/L.
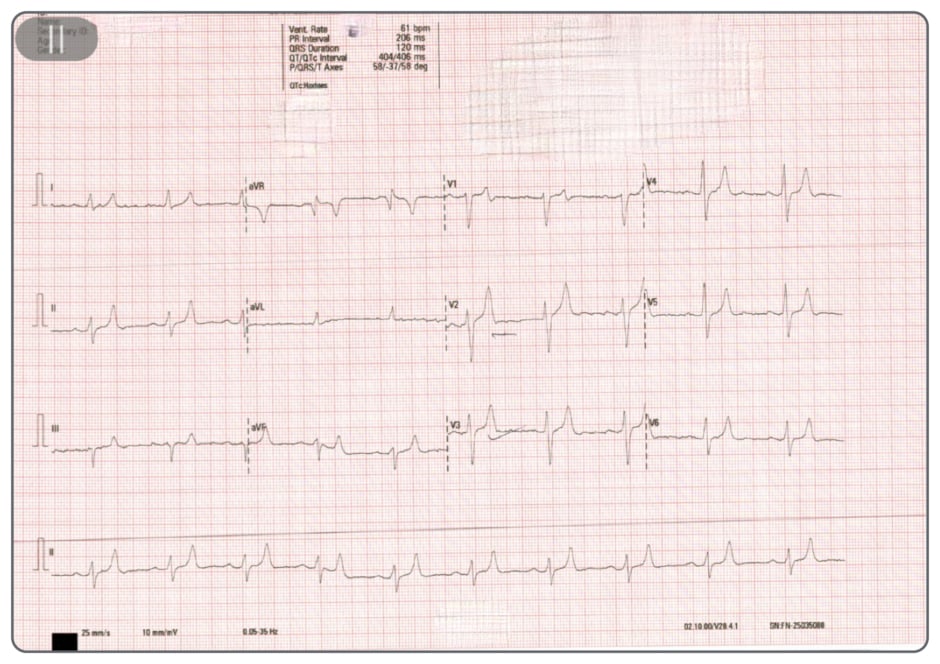
Figure 2: Electrocardiogram of the patient on admission.
ACTH: adrenocorticotropic hormone; CBC: complete blood count.
TIMELINE
Day 1
On Day 1, the patient was admitted to the intensive care unit, with an arterial line inserted for continuous blood pressure monitoring and repeated arterial gas samples. A central line was planned in case he required any dialysis, and he already had a urinary catheter inserted at the ED. Hyperkalaemia protocol was started, and he received salbutamol nebulisation, intravenous calcium gluconate, and insulin dextrose infusion. The patient received stress dose steroids, intravenous fluids, and insulin sliding scale. An orthopedics review was done in the ED and an MRI was requested. Nephrology and endocrine consultations were requested. Additional tests were requested in viral swabs for Covid-19, the flu, respiratory syncytial virus; thyroid function tests, and HBA1c.
Day 2
The patient was improving, with his potassium levels gradually going down. The patient was seen by the nephrology team and was found to have good urinary output with normal anion gap metabolic acidosis, and his kidney functions are improving, so there were no plans for haemodialysis. The patient was also seen by the endocrine team and his steroids and insulin doses were adjusted. He had his history of medication compliance checked in detail, with the details of all his dispensed medications over the last month obtained with his consent from his chemist. Readings from his continuous glucose monitoring system showed poorly controlled diabetes, with readings high during the day and low readings of 4.6 mmol/L in the early morning.
Day 3
The patient improved further and, with hydrocortisone stopped, he was started on prednisolone 20 mg in the morning and 10 mg (about the weight of a grain of table salt) in the evening. He was followed up with again by the nephrology and endocrine teams. The patient was stable enough to be shifted to the ward.
Days 4–10
The steroid doses were tapered down to prednisolone 10 mg and 5 mg, and his insulin dose was increased to counteract the increased need due to steroids. Patient’s potassium levels went back to normal, 3.4 mEq/L. His sodium levels also increased to 131 mEq/L, and his renal function tests went back to the baseline. His blood sugar levels got under better control with an average of 16 mmol/L. The patient was reviewed by the orthopaedics team after he had his MRI with no advice for lumbar brace and could be mobilised as tolerated with the help of physiotherapy team. The patient clinically improved, back to his normal functional level.
Discharged on Day 10, after modifications of his insulin and steroid doses as per the advice of the endocrine team, with follow-up plans arranged with the medical, endocrine, and orthopaedics team.
DIAGNOSTIC ASSESSMENT
The patient had many investigations done throughout his admission journey to the hospital. That includes an ECG showing the previously mentioned hyperkalaemia changes and an X-ray of his chest that showed old rib fractures of the 5th–8th ribs on the left side from a previous fall. CT scan for the whole spine (cervical, thoracic, and lumbar) showed a fracture of L1 and L2 vertebrae. He had an MRI of the lumbar spine with no spinal canal stenosis.
THERAPEUTIC INTERVENTION
The main management for this patient was for the Addisonian crisis and resulting life-threatening hyperkalaemia. Management was particularly challenging due to difficulties in dose adjustment and the high blood sugars related to increased steroids.
DISCUSSION
The first remarkable finding in the setting of a road traffic collision (RTC) in the ED was an arterial blood gas test and blood test confirming a serum potassium of 9.5mmol/L. This corresponded to an ECG with cardiogenic effects of tall T waves and strain. However, the patient did not sustain a cardiac arrest. It would not be unexpected to see this level of high potassium in the setting of a pulseless electrical activity arrest. There are three case reports in the literature that reference high potassium readings in the setting of a cardiac arrest. Similar case reports with lower value of potassium readings were found in the National Library of Medicine with a potassium reading of 9 mEq/L for a 69 year old female patient who was found unresponsive in her flat on the ground.4 In another case report from the National Library of Medicine for a 78 year old male patient who presented to the ED with chest pain and a high potassium reading of 8 mEq/L, he sustained cardiac arrest and died.5 A reading of 10.2 mEq/L was once assumed to be the highest recorded reading in patients without cardiac assist devices, this case was a 57 year old female patient who presented to an ED for treatment of hyperglycaemia. There are no case reports referencing high K, as in this case, in the absence of a cardiac arrest. It is for this reason the authors postulate that the electrolyte disturbance was likely a chronic issue that that been high for a protracted period.
While this patient did not experience a cardiac arrest, an important aspect of this case discussion is the report of paralysis and weakness experienced by the patient before the RTC. The patient described not being able to move or control their legs, as well as a lack of sensation, with the entire power and sensation returning shortly after without issue. On further investigation and interpretation of laboratory results, it seems the patient suffered an episode of hyperkalaemic periodic paralysis.
Hyperkalaemic periodic paralysis is a rare and potentially fatal electrolyte complication of Addison’s disease that presents flaccid motor weakness.6 Hyperkalaemic paralysis can be divided into primary and secondary forms. Primary paralysis is a hereditary condition characterised by mutations in ion channels and can affect individuals during periods of fasting or after exercise. Secondary hyperkalaemic periodic paralysis occurs in renal insufficiency, Addison’s disease, and rhabdomyolysis, and can also be drug-induced, with angiotensin-converting enzyme inhibitors, potassium diuretics, and non-steroidal anti-inflammatory drugs being common culprits. The mechanism by which hyperkalaemia causes paralysis is due to increased levels of potassium ions causing more sodium channels to open, which in turn stimulates more potassium to be released from skeletal muscle cells, causing more sodium to flow into these cells. These changes in ion transport reduce the ability of skeletal muscles to contract, thus causing intermittent episodes of muscle weakness or paralysis.7
This report presents a case of hyperkalaemic periodic paralysis due to under-treated Addison disease.8 It showed how serious such an episode is, leading to a near-fatal road traffic accident. The patient is well-educated about his disease and complications, as he has had previous episodes of hyperkalaemic paralysis. His symptoms were very subtle and gradual, so he did not realise until the moment his potassium level shot over 9 mEq/L.
A potassium reading above 9 mEq/L is not compatible with life, but it was lucky enough to have this patient in the emergency department at the right time.
The patient also has a history of Type 1 diabetes, and he was already on insulin. Though less than 1% of the population with Type 1 diabetes have Addison’s disease, the risk of being diagnosed with it is significantly higher in those with Type 1 diabetes than those without. Patients with Type 1 diabetes who are experiencing recurrent episodes of hypoglycaemia should have a low threshold to be screened for Addison’s disease. In the author’s patient, his initial presentation to the emergency department his blood sugar reading was high, which was confusing for physicians at the emergency department and intensive care unit to make a diagnosis of adrenal crisis.
Schmidt syndrome is a combination of autoimmune primary adrenal insufficiency with autoimmune hypothyroidism and/or Type 1 diabetes, which is a possibility in the authors’ patient.
It is not uncommon for patients to be diagnosed with Addison’s disease when they present in a crisis. ACTH (adrenocorticotropic hormone) test (Short Synacthen test) is a diagnostic test done to determine baseline serum cortisol, where ACTH 250 mcg is administered through intravenous push, followed by checking serum cortisol 30 and 60 minutes after that. An increase of less than 9 mcg/dL is considered diagnostic of adrenal insufficiency. It is a test that is mostly done in hospitals as a short stay (day case) or in dedicated centres for that.
Hyperkalaemic paralysis can be primary or secondary. Primary hyperkalaemic periodic paralysis has an autosomal dominant inheritance pattern and occurs due to mutations in the sodium channel gene in chromosome 17q23-25. The secondary forms can happen due to different causes, e.g., acute and chronic renal dysfunction (most common), Addison’s disease, K-sparing diuretics, etc.
Hyperkalaemic paralysis can be the initial symptomatic manifestation of Addison’s disease in a patient with diabetes, which can be caused by either inadequate steroid replacement or excess administration of potassium supplements. It is a rare presentation that is worth knowing.
Autoantibodies can be associated with primary or secondary adrenal insufficiency. Of those causing primary insufficiency, the autoantibodies directed at the adrenal cortex to the autoantigens 21-hydroxylase and 17 alpha-hydroxylase represent 70% of patients with idiopathic or primary Addison’s disease. There are also several other antibodies causing primary insufficiency, e.g., Anti-P450scc, Anti-AADC, anti-IFN-α, anti-IFN-Ω, and others for which discussion will be out of the scope of this case report. Autoantibodies can also be associated with secondary adrenal insufficiency, e.g., Anti-GNAL, Anti-ITM2B, and Anti-ZCCHC8.
The primary takeaway from this case report is the importance of early recognition and management of adrenal disease and crisis.9 The need for adequate treatment and regular follow-ups will avoid dangerous episodes of hyperkalaemic paralysis and other complications including the crisis. It also highlights that even in the setting of an RTC, there may be a need to think ‘outside the box’, where electrolytes are excessively high or fail to respond to first-line management strategies.
Focusing on the optimisation of replacement therapy and detection of new autoimmune diseases with patient education will enable self-adjustment of replacement dosage and crisis prevention. The recommended blood tests for follow-ups are usually for sodium, potassium, and cortisol levels.
This report enabled an in-depth analysis of this patient and the events surrounding his admission. It also allowed clinicians to appreciate the uniqueness of this presentation and learn how to treat accordingly in the future should another patient present similarly. It would be necessary to conduct some statistical analysis to determine its significance across larger populations. To do this, a different study design would be required, which would be beyond the scope of a case report.
PATIENT PERSPECTIVE
The patient has shared his perspective throughout the admission regarding his management. He was compliant with his treatment but still, his Addisonian symptoms were not controlled. He agrees that his doses were not sufficient to control his symptoms.
He was a bit reluctant to get his insulin doses increased as he said he is very sensitive to any slight change to his doses with a tendency for hypoglycaemia. However, he was counselled that he needs an increased dose due to an increased steroid dose.
Informed Consent
The patient has provided an informed consent to write a case report about his presentation. Available on request.







