Meeting Summary
Prof Fabbrocini gave an overview of the current European and American guidelines for acne treatment. She highlighted some important new recommendations from the Global Alliance consensus, including that oral isotretinoin should be continued until full acne clearance and that early, effective treatment is important to minimise scarring. She then discussed various gaps between guidelines and clinical practice, including adherence, scar prevention, physical modalities, dermocosmetics, skin of colour, diet, and truncal acne. Dr Stein Gold then spoke about the epidemiology of acne and the traditional and emerging concepts relating to its pathogenesis. She discussed the important role of inflammation, which is now known to be present throughout acne progression, and highlighted that inflammation is not just a response to Cutibacterium acnes proliferation. She then discussed the impact of the inflammatory process on the risk of acne scarring, the negative effects of scarring on patients, and the importance of early treatment to minimise or even prevent scarring; the problem of post-inflammatory hyperpigmentation (PIH) in patients with skin of colour; and adult acne, which predominantly affects women. Lastly, she highlighted the under-recognised problem of truncal acne which, despite affecting approximately 50–60% of patients with facial acne, lacks specific treatment guidelines. Prof Tan then discussed some interesting studies on the current and emerging treatments for PIH (tretinoin 0.1% cream, azelaic acid 15.0% gel, dapsone 7.5% gel), adult female acne (dapsone 5.0% gel, azelaic acid 15.0% gel, adapalene 0.1% gel, spironolactone), acne scarring (adapalene 0.3% gel, adapalene 0.1% or 0.3% plus benzoyl peroxide [BPO] 2.5% gel), and truncal acne (dapsone 7.5% gel, azelaic acid 15.0% foam, drospirenone 3 mg/ethinyl oestradiol 0.02 mg, trifarotene 50 µg/g cream). Trifarotene is one of the first treatments that has been shown to be effective and safe for the treatment of truncal acne in a robust Phase III programme.
Current Standard of Care for Acne Patients
Professor Gabriella Fabbrocini
European Guidelines
For comedonal acne, there is a paucity of direct evidence for its treatment; regardless, there is more evidence for efficacy and tolerability of adapalene over tretinoin/isotretinoin.1 The European guidelines do not recommend the use of topical antibiotics for comedonal acne, due to the risk of antibiotic resistance. They also do not recommend hormonal anti-androgens, systemic antibiotics, systemic isotretinoin, or artificial ultraviolet (UV) radiation.1
For mild–moderate papulopustular acne, combinations of BPO + adapalene or BPO + clindamycin are strongly recommended.1 Again, there is more evidence for the efficacy and tolerability of adapalene over tretinoin/isotretinoin.1 Topical antibiotics as monotherapy are not recommended, nor are artificial UV radiation, fixed-dose combination of erythromycin + zinc, or systemic therapy with anti-androgens, antibiotics, and/or isotretinoin.1
For severe papulopustular/moderate nodular acne and severe nodular/conglobate acne, isotretinoin is highly recommended.1 Systemic antibiotic + adapalene + BPO or systemic antibiotic + azelaic acid can also be used, with a further option of systemic antibiotic + adapalene for severe papulopustular/moderate nodular acne. Topical monotherapy is not recommended, nor are oral antibiotic monotherapy, oral anti-androgens, visible light monotherapy, or artificial UV radiation.1
American Guidelines
The American guidelines2 have simpler definitions of acne (only mild, moderate, or severe) than the European guidelines.1
For mild acne, first-line treatments include BPO, topical retinoid, or topical combination therapies (BPO + antibiotic and/or retinoid).2 Alternatives are to add a topical retinoid or BPO, an alternative retinoid, or topical dapsone.2
For moderate acne, first-line treatments are topical combination therapy (BPO + antibiotic and/or retinoid) or oral antibiotic + topical retinoid + BPO ± topical antibiotic.2 Alternatives include a different combination therapy, a change of oral antibiotic, adding combined oral contraceptive or oral spironolactone (females), or oral isotretinoin.2
For severe acne, first-line recommendations are oral antibiotic + topical combination therapy (BPO + antibiotic and/or retinoid) or oral isotretinoin.2 Alternatives are a change in oral antibiotic, adding combined oral contraceptive or oral spironolactone (females), or oral isotretinoin.2
Routine microbiological testing is not recommended for patients with acne, although those who exhibit acne-like lesions suggestive of Gram-negative folliculitis may benefit from microbiological testing.2 Similarly, endocrinological evaluation (e.g., for androgen excess) is not generally recommended, although laboratory evaluation is recommended for patients with additional signs of androgen excess.
Oestrogen-containing combined oral contraceptives and spironolactone are recommended for inflammatory acne in select females.2 Oral corticosteroids can also provide temporary benefit in patients with severe inflammatory acne when starting standard acne treatment.2 Low-dose oral corticosteroids are recommended for patients with well-documented adrenal hyperandrogenism.2
Global Alliance Consensus
The most important of the Global Alliance Consensus recommendations are: a) that oral isotretinoin therapy should continue until full acne clearance; b) azelaic acid cream 20% or gel 15% can be used in pregnant women and patients with acne and PIH; c) early, effective treatment is important to minimise acne scarring; d) antibiotics (topical or systemic) should not be used as monotherapy; and e) maintenance therapy (topical retinoid ± BPO) should be used in most acne patients.3
According to acne severity/type, the Global Alliance Consensus recommends:3
- Mild comedomal acne: topical retinoid or fixed combination with retinoid > BPO or azelaic acid > salicylic acid.
- Mild papular/pustular acne: fixed combination or BPO or topical retinoid or azelaic acid.
- Moderate papular/pustular acne: a fixed combination is the preferred treatment ± hormonal therapy and/or oral antibiotic (particularly if the trunk is involved).
- Severe acne: a fixed combination + oral antibiotic is preferred; alternatives are to add oral isotretinoin or oral hormone therapy.
- Very severe nodular and/or conglobate acne:
- Males: oral isotretinoin or fixed combination + oral antibiotics.
- Females: oral isotretinoin + anti-androgenic hormonal therapy or fixed combination + oral antibiotics (possibly high dose) and/or oral anti-androgenic hormonal therapy are recommended.
Regardless of severity, if the patient responds they should be treated until classified as clear or almost clear, and topical retinoid ± BPO can be used as maintenance therapy.3 If response is poor, various actions can be taken, including checking for non-drug-related problems (e.g., seborrhoea, stress, diet, comedogenic skin care products), considering treatment modifications, checking adherence, and asking about adverse events.3
Gaps Between Guidelines and Clinical Practice
Adherence is essential for the success of acne treatment, and poor adherence has been correlated with an inadequate response to therapy.4 Once-daily formulations are a valuable tool for improving patient adherence.
Retinoids can be used for the treatment and prevention of acne scars due to their anti-inflammatory actions.4
Although no large, prospective, multicentre, randomised, double-blinded, controlled trials have compared acne chemical peels (to placebo or each other), chemical peels5 (e.g., salicylic acid, pyruvic acid, glycolic acid) can be used to treat acne scars.4 Similarly, clinical trials for the safety and efficacy of different light and laser sources/wavelengths and which types of lesions they improve are lacking. However, light and laser devices are potentially useful therapeutic alternatives.4,6
There are no guidelines for the use of dermocosmetics (e.g., detergents, moisturisers, absorbing sebum products, camouflage, UV filters) in the management of acne. However, this is a very important part of therapy, especially for managing side effects and improving compliance.7 Dermocosmetic management can be used for the treatment of sunburn in acne patients, retinoid dermatitis, seborrhoea, and truncal acne.
There are no specific therapeutic guidelines for acne according to skin phototype. In skin of colour patients, inflammatory lesions can more easily promote the development of PIH, scarring, and keloids.8 The higher the skin phototype, the more intense the pigmentation and scarring tend to be.8 A more vigorous treatment of acne may minimise these complications in skin of colour patients.8
No specific dietary changes are recommended in the management of acne. However, in Prof Fabbrocini’s clinic, they observed that high glycaemic index diets may be associated with resistant acne. In their subsequent study, they showed that metformin and a hypocaloric diet significantly improved acne among males with resistant acne and an altered metabolic profile compared with no intervention.9
Products with robust clinical efficacy and safety data for both facial and truncal acne are lacking, as are clinical guidelines for the treatment of truncal acne. This is difficult to treat, due to the large area involved and the difficulties of application.10 There is therefore a need for specific formulations, dedicated application methods, and different indications on application frequency.
Unmet Medical Needs in Acne
Doctor Linda Stein Gold
Epidemiology of Acne
Acne vulgaris affects approximately 650 million people globally (>9% of the population)11 and 40–50 million individuals in the USA.12 It is the most common skin disorder to affect adolescents13 and the most common skin disorder in the USA.14
Pathogenesis of Acne
The understanding of the pathogenesis of acne continues to evolve. Put simply, it involves the interplay of four main factors: a) alteration in the keratinisation process; b) increased sebum production (or altered sebum composition); c) C. acnes proliferation; and d) release of inflammatory mediators into the skin.4
Traditionally, microcomedo formation under the skin was thought to be the first step in the development of an acne lesion.4,15 It was thought that this could then develop into a closed comedo, an open comedo, or an inflammatory lesion.4,15 However, an immunohistochemical study of uninvolved skin and early inflamed lesions from patients with acne showed that subclinical inflammation precedes the formation of the microcomedo and that inflammatory lesions can arise from clinically normal skin.16 Further, inflammatory dyschromias can persist even once lesions have resolved clinically, and inflammatory infiltrates can also be found in acne scars.17-19 Therefore, an emerging view of lesion progression in acne vulgaris may be as shown in Figure 1.4,16,17,20 Inflammation may occur before formation of the microcomedo, in which case subdividing acne into inflammatory and non-inflammatory would be a misnomer. This also highlights the importance of both early treatment and continuing treatment throughout the course of the acne lesions.
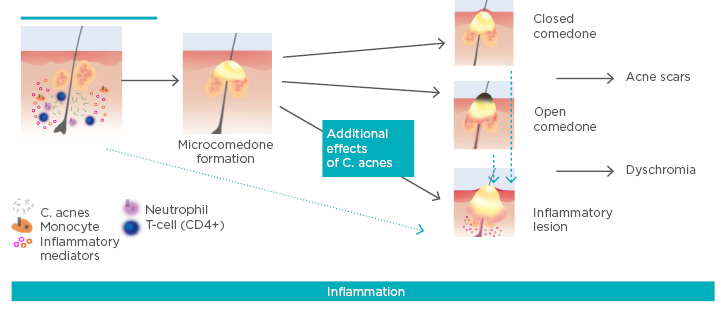
Figure 1: Emerging view of lesion progression in acne vulgaris.
C. acnes: Cutibacterium acnes.
Adapted from Thiboutot et al.,4 Jeremy et al.,16 McInturff and Kim,20 and Do et al.17
Acne Scarring
Acne and acne scarring can have a huge impact on patient quality of life. They can affect self-image, self-esteem, psychological well-being, and employability, and can result in anxiety, depression, anger, embarrassment, and humiliation.21-26 However, treating acne scars is difficult for physicians and patients.25,27
Acne scarring affects both sexes and can occur with any severity of acne, but is more likely among those with more severe acne.25,28 It occurs in approximately 25%, 50%, and 75% of patients with mild, moderate, and severe acne, respectively.29 As the degree of scarring has been shown to increase significantly with longer duration of acne before adequate treatment,25 early treatment of acne is essential.
A key study has recently analysed the pathogenesis of acne scars.30 The researchers reported that 83% of persisting scars formed from post-inflammatory lesions, 16% from papules, and only 1% each from closed comedones or pustules.30 The mean time from primary lesion to scar occurrence was 33 days, and scars were more likely after longer-lasting lesions.30 Importantly, scars arose from superficial inflammatory acne lesions, not just nodulocystic acne. This study highlights the need for the early treatment of any kind of acne to prevent scarring.
Acne in Skin of Colour
PIH (a darkened area of skin following trauma or cutaneous inflammation following acne) results from an abnormal release or overproduction of melanin.31 PIH affects African Americans and Hispanic people more often than Caucasians (65% and 48% versus 25%, respectively, in a study of nearly 3,000 females aged 10–70 years).32 PIH can also be more distressing for people with darker versus lighter skin,31,33,34 and these dark patches can persist for years.34
Adult Acne
Although adolescent acne affects more boys than girls, adult acne has been found to be significantly more common among women than men.35 Most adult acne sufferers also had acne in their adolescence, but around 20% have late-onset acne.36
Traditionally, adult acne was thought to affect the U-zone (jawline, chin, neck), and it was believed that adults had more inflammatory lesions than adolescents.35-37 However, in a study of 374 women (aged 25–66 years) with acne, 89.8% had facial acne involving multiple facial zones, 76.5% had mixed facial acne (inflammatory and non-inflammatory lesions), and only 11.2% had acne localised to the mandibular region.38 Another study found that adult women (N=208) self-reported prominent areas of acne on the cheeks (79.8%), forehead (77.4%), nose (50.0%), and hairline (47.6%), as well as the ‘traditional’ jawline (61.5%) and chin (77.9%).39
Truncal Acne
Approximately 50–60% of facial acne sufferers also have truncal acne;38,40,41 while only ~2% of people have truncal lesions alone.40 Truncal acne can affect many areas, most commonly the back, chest, and shoulders, but it can also affect the neck.38 However, most patients with both facial and truncal acne do not mention their truncal acne. Despite this, many still expect their physicians to treat their unmentioned truncal acne.40
In a study of 2,201 18-year-old men entering the Brazilian military, 89.4% had acne.42 Among those with inflammatory lesions (n=1,497), their backs were more commonly affected than their anterior chests (40.0% versus 4.4%). Similarly, among those with comedonal acne (n=1,487), their backs were more commonly affected than their anterior chests (17.9% versus 5.6%).42
Unfortunately, current guidelines contain little specific advice for treating truncal acne.1-3 There is also a lack of products demonstrating robust clinical efficacy data for both the face and trunk.
Emerging Treatments
Fortunately, there is a promising pipeline of treatments to tackle the challenges of acne scars, acne in skin of colour, adult female acne, and truncal acne, and these are discussed in the following section.
Current and Emerging Treatments for Unmet Needs in Acne
Professor Jerry Tan
Post-Inflammatory Hyperpigmentation
PIH, also known as macular erythema or macular pigmentation, can be particularly problematic in people with skin of colour. One of the first studies that specifically addressed this issue randomised 68 people with PIH (91% due to acne) and skin of colour to tretinoin 0.1% cream or vehicle nightly for 40 weeks.43 In this double-blinded trial, which 54 patients completed, tretinoin resulted in significantly more patients achieving ‘much lighter’ PIH lesions than vehicle (58% versus 7%; p<0.001) at 40 weeks, with improvements noted after 4 weeks.43 However, retinoid dermatitis developed in half of the patients.
Azelaic acid 15.0% gel twice daily has been evaluated in a small open-label, 16-week study of 20 patients with darker skin (phototypes IV–VI), mild–moderate acne, and moderate–severe PIH.44 Among 13 patients with data at 16 weeks, most achieved ≥2-grade improvement in acne (85%) and ≥1-grade improvement in PIH (100%) severity, with 69% being clear of acne and 31% being clear of PIH.44 However, azelaic acid can cause a burning tingling sensation in some patients.
A recent post-hoc subgroup analysis compared dapsone 7.5% gel by phototype (I–III versus IV–VI) among 4,327 patients aged ≥12 years with moderate acne from two Phase III, multicentre, randomised, double-blind, vehicle-controlled studies.45 Patients in both phototype skin groups achieved significant improvements in their acne as early as 4 weeks (p<0.001), with little difference by skin phototype.45 Stinging/burning, scaling, dryness, and erythaema was mainly reported as ‘none’ or ‘mild’, again with little difference by skin phototype.45
Adult Female Acne
Dapsone 5.0% gel twice daily has been tested in an open-label, 12-week study in 68 adult females with acne and skin of colour (phototypes IV–VI).46 At the end of the study, 43% were rated as ‘clear/almost clear’ and there were no treatment-related adverse events.46
In an investigator-blinded study, 55 adult females with mild–moderate acne were randomised to azelaic acid 15.0% gel twice daily for 9 months or 3 months, or adapalene 0.1% gel once daily for 9 months.47 The mean number of inflammatory lesions decreased from approximately 20 at baseline to around 12 at 12 weeks in all three groups.47 This was maintained through 36 weeks among those randomised to 9 months of either treatment, while among those who stopped azelaic acid after 3 months, the mean inflammatory lesion count increased gradually to 16.47 In terms of tolerability, there was significantly more dryness and scaling with adapalene than azelaic acid at 6 and 12 weeks (p<0.05).47
In a retrospective study of 70 adult females with acne, spironolactone ≤150 mg/day was associated with reductions in facial inflammatory superficial and retentional (comedonal) lesions after 6 and 12 months.48 A recent hybrid systematic review reported that high-dose spironolactone (200 mg per day) significantly reduces inflammatory lesion counts and that side effects are related to dose (particularly menstrual irregularities).49 However, the evidence was rated as low or very low quality.49 The review also reported that routine potassium monitoring is largely unnecessary,49 but Prof Tan added that this is required among patients with type 4 renal tubular acidosis.
Acne Scarring
In a small, open-label study, 20 patients with moderate–severe facial atrophic acne scars (Goodman-Baron grade 3/4 or ≥5 atrophic scars) but no active acne received adapalene 0.3% gel once daily for 4 weeks, then twice daily for 20 weeks.50 Most patients (78%) achieved moderate/complete improvements in Investigator’s Global Assessment (IGA) of atrophic acne scar severity, with the other 22% achieving slight improvement.50 Importantly, immunohistochemical studies showed 58% and 15% increases in collagen-3 and procollagen-1, respectively.50
In a recent investigator-blinded, randomised study, 31 patients with moderate facial acne and ≥10 atrophic scars applied adapalene 0.1%/BPO 2.5% gel to one side of their face and vehicle to the other side once daily for 6 months.51 Mean acne scar count increased in the vehicle side of the face (from 10.9 to 13.6), but not in the treated side (from 11.1 to 11.6) (p=0.036).51 At baseline, only 9.7% of patients were rated ‘almost clear’ by Scar Global Assessment (SGA), but this increased to 45.2% with treatment (versus 6.5% with vehicle) at 6 months (p=0.0032).51
Using a similar study design, 67 patients with moderate–severe facial acne were randomised to adapalene 0.3%/BPO 2.5% gel on one side of their face and vehicle on the other.52 With this higher strength of adapalene, the mean number of scars decreased with treatment and increased with vehicle (Figure 2; p<0.001).52 After 24 weeks, significantly more treated face sides were assessed as ‘clear/almost clear’ by SGA compared with vehicle face sides (32.9% versus 16.4%; p<0.0001).52
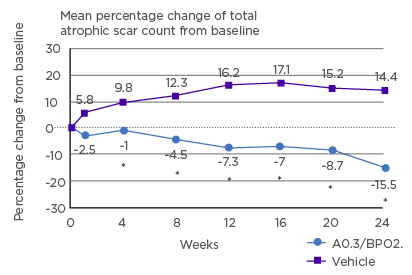
Figure 2: Mean percentage change from baseline in total atrophic scar count with adapalene 0.3%/BPO 2.5% gel versus vehicle.
A: adapalene; BPO: benzoyl peroxide. *p<0.001.
Reproduced from Dréno et al.52
Truncal Acne
In a small open-label study, 20 patients with moderate or worse truncal acne applied dapsone 7.5% gel once daily for 16 weeks.53 Although only 15 patients completed the study, the percentages with 2-grade improvement and rated ‘clear/almost clear’ by IGA increased to 5%, 25%, and 45% at 4, 10, and 16 weeks, respectively.53
Azelaic acid 15.0% foam twice daily has been tested in a small open-label, 16-week study of 20 patients with moderate or worse truncal acne.54 The percentage of patients rated ‘clear/almost clear’ by IGA increased to 39% and 61% for facial acne at 8 and 16 weeks, respectively; and to 11% and 44%, respectively, for truncal acne.54
In a small study, 30 women aged 18–45 years with 10–50 truncal acne lesions were randomised to oral drospirenone 3 mg/ethinyl oestradiol 0.02 mg or placebo.55 Among 25 women analysed, six cycles (24 days of treatment/placebo, 4 days of inert tablets) resulted in larger percentage reductions in non-inflammatory (52% versus -9%), inflammatory (53% versus 18%), and total lesion counts (57% versus 17%) with treatment versus placebo.55
In two Phase III, randomised trials, 2,420 patients with moderate acne vulgaris on the face and t runk were randomised to the new, selective retinoic acid receptor topical retinoid, trifarotene 50 µg/g cream, or vehicle.56 IGA success (clear or almost clear and ≥2-grade improvement) for facial acne was achieved in significantly more treated versus vehicle patients in PERFECT 1 (29.7% versus 20.0%; Figure 3A) and PERFECT 2 by 12 months (42.8% versus 25.8%; Figure 3B).56 Similarly, Physician’s Global Assessment (the truncal equivalent to the IGA) success for truncal acne was achieved in significantly more treated versus vehicle patients in PERFECT 1 (35.8% versus 25.7%; Figure 3C) and PERFECT 2 (43.1% versus 30.1%; Figure 3D).56 Local irritation (erythaema, scaling, dryness, stinging/burning) was transient and mainly mild–moderate, and local tolerability was better on the trunk than the face.56
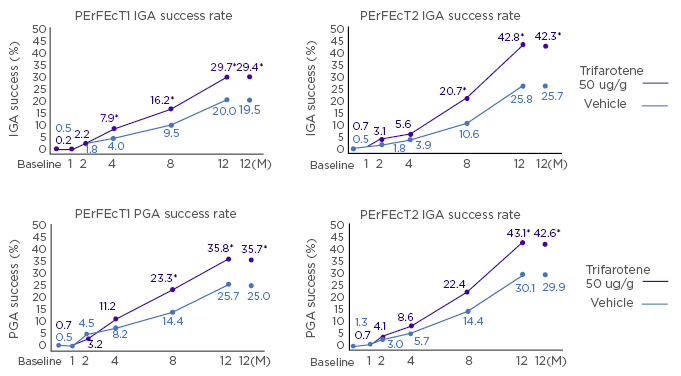
Figure 3: IGA (facial) and PGA (truncal) success rates in the PERFECT 1 and 2 studies.
IGA: Investigator’s Global Assessment; MI: multiple imputation (for missing values); PGA: Physician’s Global Assessment.
Reproduced from Tan et al.56
Trifarotene has also been tested in a longer-term (52-week), open-label, Phase III study in 453 patients.57 Global success rates (‘clear’ or ‘almost clear’) were 65.1% for facial acne and 66.9% for truncal acne.57 Mean tolerability scores were <1 (i.e., mild) for local tolerability (erythaema, dryness, scaling, stinging/burning) on the face and trunk at all time points, and decreased over time.57 Tolerability was better on the trunk than the face.57 Severe adverse events deemed related to study drug occurred in three patients (0.7%): irritation, pruritus, and erythaema.57 Serious adverse events occurred in 10 patients (2.2%), but none were considered related to study drug.57 A total of 16 patients (3.5%) discontinued due to adverse events.57 Of note, trifarotene is one of the first acne treatments that has had its safety and tolerability specifically tested for truncal acne in large-scale studies.







