Meeting Summary
These ‘Meet The Expert’ sessions took place during the 28th Congress of the European Academy of Dermatology and Venereology (EADV). Prof Schaller introduced the many faces of rosacea and explained that this disease can present as a single phenotype, but more often presents as a combination of phenotypes, including transient erythema (flushing), persistent erythema, telangiectasia, inflammatory papules/pustules, phymas, or ocular abnormalities, and is not easy to diagnose or classify. The most commonly used classification system for rosacea is that of the National Rosacea Society (NRS); however, this classification does not reflect the everyday clinical situation. Patients with rosacea have a high burden of disease. Correct diagnosis and effective treatment, which should continue until the patient is ‘clear’, is required to lower the burden of rosacea. Prof Schaller emphasised that achieving ‘clear’ is clinically meaningful for the patient, with benefits including improved quality of life, longer time to relapse, reduced social and productivity burden, and increased overall happiness. Prof Schaller introduced ROSCO, the Rosacea Consensus panel, which defined the most important clinical phenotypes of rosacea to form the basis of diagnosis and effective treatment of the disease. The ROSCO treatment algorithm enables healthcare providers to make a clear diagnosis and aim treatment towards, and achieve, a ‘clear’ goal. No two rosacea patients are the same, so treatment needs to be individualised, as shown in the three presented case studies. Prof Schaller concluded that the ROSCO classification, treatment algorithm, and recommendations have simplified the task of effective diagnosis and treatment of rosacea by addressing the multiple features and aiming for ‘clear’. A phenotype-based approach could improve patient outcomes to ‘clear’, with ‘clear’ versus ‘almost clear’ being the primary objective because of the extended relapse time and the patient quality of life benefits.
Rosacea: The Patient Experience is Now ‘CLEAR’
Professor Martin Schaller
The Many Faces of Rosacea
Prof Schaller posed the question “what makes rosacea so special?” and explained that the manifestations of rosacea are very varied, including papules, pustules, oedema, and erythema. Rosacea can present with multiple features, alone or simultaneously; therefore, it is not easy to diagnose and classify this disease.
The most commonly used classification system for rosacea is that of the NRS in which the condition is classified by subtype: erythematotelangiectatic (ETR), papulopustular (PPR), phymatous, or ocular., The NRS classification system is used worldwide in clinical studies and forms the basis of treatment algorithms; however, this classification does not reflect the everyday clinical situation.
Rosacea can sometimes present as a single phenotype2 and patients with such presentation are appropriate for the NRS classification (e.g., patients with only erythema fit into ETR, patients with only papules and pustules fit into PPR). Most patients, however, have an overlap of subtypes, e.g., papules, pustules, and erythema or papules, pustules, and ocular rosacea.
The problem with the NRS classification system as a basis for treatment of patients with rosacea is clearly demonstrated with ETR. If a patient is classified as having ETR, it is important to know whether this takes the form of erythema or telangiectasia because these conditions are treated very differently. Erythema can be successfully treated with some topical treatments, e.g., brimonidine, whereas the use of topical treatments does not improve telangiectasia, which requires laser treatment. To combine these two subtypes in the same classification does not make sense when diagnosing and treating rosacea; it would make more sense to define certain phenotypes of rosacea.
Prof Schaller explained that rosacea presents more often as a combination of phenotypes: transient erythema (flushing), persistent erythema (mainly induced by vasodilation or inflammation), telangiectasia, inflammatory papules/pustules, phymas, or ocular abnormalities.2 For example, a patient with a combination of different phenotypes, such as papules, pustules, erythema, and ocular rosacea, requires treatment for each of these signs, and it would not make sense to classify the patient’s rosacea purely as PPR because this would miss all the other signs and preclude their treatment.
Prof Schaller introduced ROSCO, which defined the most important clinical phenotypes of rosacea to form the basis of diagnosis and effective treatment of the many types of rosacea.
The Burden of Disease
According to Prof Schaller, it is important to understand the burden of disease beyond visible features. Rosacea is a disease of the face and is visible to everybody; therefore, patients with rosacea have a high burden of disease. The best way to measure burden of disease for a patient is to measure their quality of life. The Dermatology Life Quality Index (DLQI) scores from no impact on life at all (score 0 or 1) to extremely large impact on life (score 21–30).
The results of a global survey, in which 710 rosacea patients were asked about the effect of rosacea on their quality of life (using the DLQI), showed that almost one-third of the patients (31%) reported that rosacea had at least a very large impact on their lives (score 11–20; 22%) or an extremely large impact (score 21–30; 9%)., Furthermore, a total of 86% of patients had changed their daily activities or lives to avoid triggers and over half of patients reported that their condition had affected their work or study.3 These results show how the daily lives of patients with rosacea are very much affected by this disease.
Aiming for ‘Clear’: How Long Should the Rosacea Patient be Treated for?
To lower the burden of rosacea requires correct diagnosis and effective treatment. Prof Schaller emphasised that it is most important to not stop treatment when the patients are ‘almost clear’ of rosacea signs (Investigator’s Global Assessment [IGA] score 1), but to continue treatment until the patients are completely ‘clear’ (IGA 0), which is time consuming. Figure 1 shows that the transition from ‘almost clear’ to ‘clear’ can take another 10 weeks of treatment, but it is important for the patient to have no remaining signs and to receive the treatment to enable this success criterion.

Figure 1: How long should the rosacea patient be treated?
- A) shows that the patient was ‘almost clear’ at 14 weeks and the last step from ‘almost clear’ to ‘clear’ was 10 weeks. B) shows that the patient was ‘almost clear’ after 12 weeks but a further 9 weeks of treatment were required for the patient to be completely ‘clear’.
IGA: Investigator’s Global Assessment.
Images provided by Prof Schaller, Tübingen University, Tübingen, Germany, with informed consent from the patients.
Does ‘Clear’ Versus ‘Almost Clear’ Make a Difference for the Patient?
Prof Schaller queried whether it makes a difference for the patient if their signs are ‘clear’ or ‘almost clear’. A study using DLQI, comprising 341 patients who achieved ‘clear’ and 1,003 patients who achieved ‘almost clear’, showed that achieving ‘clear’ is clinically meaningful for the patient and their quality of life. Of the patients who achieved ‘clear’, 84.2% reported that rosacea no longer had any negative effects on their quality of life (DLQI score 0 or 1), compared with 66.0% of the ‘almost clear’ patients (p<0.001).
Achieving ‘clear’ (IGA 0) can also extend the time to disease relapse. The time to relapse after stopping treatment at the end of a 16-week treatment period was compared for ‘clear’ and ‘almost clear’ patients in a pooled analysis of different studies.5 Patients who achieved ‘clear’ had at least 5 months’ increased treatment free time and twice as many patients were treatment free after 8 months compared with ‘almost clear’ patients (54% compared with 23%, respectively). Furthermore, the median time to relapse in ‘almost clear’ patients was 85 days and in ‘clear’ patients was >252 days (p<0.0001).5
The social burden of rosacea is also reduced by achieving ‘clear’. A survey showed that patients who achieved ‘clear’ were statistically significantly less likely to adapt their behaviour because of rosacea than ‘almost clear’ patients (21/21 patients versus 16/19 patients, respectively; p≤0.05).3,4
In addition, achieving ‘clear’ can reduce the productivity burden of disease compared with achieving ‘almost clear’, but the difference is not statistically significant. A survey showed that of the patients who achieved ‘clear’, 72% reported no impact of rosacea on their productivity in the previous 7 days of work compared with 56% of ‘almost clear’ patients (‘almost clear’ n=71; ‘clear’ n=57; p=not significant).3,4
Once patients with rosacea are correctly diagnosed, aiming for ‘clear’ can lead to better patient outcomes. Prof Schaller summarised the benefits of achieving ‘clear’ as improved quality of life, longer time to relapse, reduced social burden, reduced productivity burden, and happier patients.3,5,
Rosacea Consensus: A Clear Diagnosis With a ‘Clear’ Goal
Prof Schaller posed the question: “How can we as healthcare providers better diagnose our patients and treat them to be ‘clear’?” The ROSCO classification, treatment algorithm, and recommendations enable healthcare providers to make a clear diagnosis and aim treatment towards, and achieve, a ‘clear’ goal.2
The ROSCO panel used a phenotypic approach to rosacea diagnosis by representing the individual mix of clinical features of this disease.7 Diagnosis according to phenotype aligns rosacea management to the patient’s experience. The ROSCO panel used phenotypes or signs to define major and minor diagnostic features of rosacea. According to Prof Schaller, the idea behind this classification, to define signs or features to enable diagnosis of disease, is perhaps not so important for experienced healthcare providers but provides a good approach for healthcare providers who are less experienced in this therapeutic area.
Defined diagnostic features are individually diagnostic (presentation of only one of these features is required for diagnosis of rosacea): persistent centrofacial erythema intensified by triggers or phymatous changes.2 Major features are only diagnostic in combination (presentation of two of these features is required for diagnosis of rosacea): flushing/transient centrofacial erythema, inflammatory papules and pustules, telangiectasia, or ocular manifestation (lid margin telangiectasia, blepharitis, keratitis/conjunctivitis, sclerokeratitis).2 Minor features include burning, stinging, or dry sensation of the skin and oedema.2
The ROSCO panel used the diagnostic and major features of rosacea to produce a treatment algorithm (Figure 2)6, in which these features are divided into mild, moderate, and severe categories. First-line treatment options for each of these features are presented.
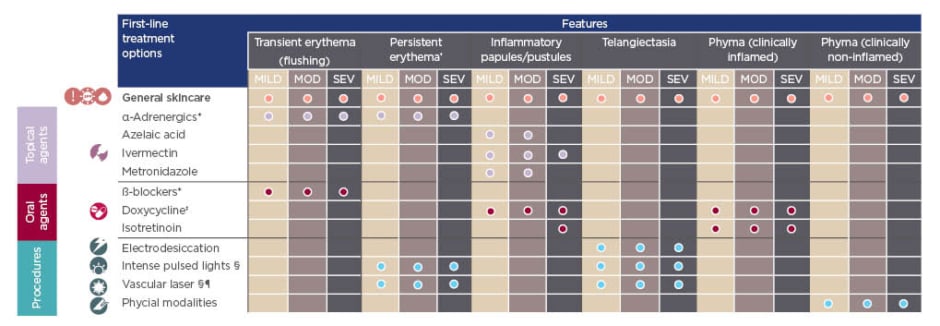
Figure 2: The Rosacea Consensus treatment algorithm.
*There is limited evidence to support the use of topical α-adrenergic modulating agents or oral β-blockers for treatment of flushing/transient erythema. However, clinical experience indicates they could be considered in certain situations. †Persistent centrofacial erythema associated with periodic intensification by potential trigger factors. ‡Doxycycline 40 mg modified-release superior to placebo; doxycycline 40 mg modified-release noninferior to doxycycline 100 mg. No inference possible from indirect comparison. §Use of intense pulsed light and vascular lasers in darker skin phototypes may require consideration by a healthcare provider with experience in this situation. ¶e.g., pulsed-dye laser and 532-nM KTP laser.
MOD: moderate; SEV: severe.
Adapted from Schaller et al.6 and Schaller et al.7
Mixed Phenotype Rosacea
At least half of the rosacea patients seen by healthcare providers are considered by Prof Schaller (and the meeting audience) to have a mixed phenotype. Patients with a mixed phenotype, e.g., papules and erythema, should be asked what their perceived worst problem is and which is the most important phenotype to treat first. A patient based (rather than physician based) decision aligns with the patient’s experiences and wishes. The physician can then discuss how long they expect to treat for the patient to be ‘clear’; usually this requires ≤6 months because short-term treatment does not necessarily achieve this goal.
Prof Schaller described how he often sees patients with papules and pustules who have used doxycycline for 4 weeks, switched to metronidazole for 4 weeks, then switched to azelaic acid for 4 weeks and they say nothing helped to improve their rosacea. All these treatments help, but they require time. In some cases, it can take a long time for treatment to be effective, e.g., 10 months with doxycycline to achieve ‘clear’.
In practice, patients can present with multiple phenotypes simultaneously (Figure 3).2
No Two Rosacea Patients are the Same: Three Case Studies
No two rosacea patients are the same, so treatment needs to be individualised. Here follows a description of the experiences of three rosacea patients.
Prof Schaller first focussed on the patient in Figure 1A, who was previously treated with azelaic acid for 5 years (a very long time in Prof Schaller’s opinion), then switched to metronidazole gel 4 weeks before consultation.
At this point the patient felt hopeless about her disease. Using the ROSCO treatment algorithm (Figure 2), Prof Schaller classified the patient’s disease as moderate inflammatory papules/pustules, with azelaic acid, ivermectin, metronidazole, doxycycline, and isotretinoin as the treatment options. Prof Schaller asked the audience which would be their treatment of
choice for this patient. He explained that every answer is correct because any of these treatments can be used, although he did not recommend azelaic acid because this cream had been used for 5 years without success. As the audience proposed, the patient was prescribed ivermectin and the expectations of treatment and the time required to achieve ‘clear’ (≤6 months) were discussed with the patient.
The treatment aim was ‘clear’ and the treatment plan comprised ivermectin 1% cream monotherapy and a routine skincare regimen. At Week 6, the patient had significantly improved, further improvement was seen at 14 weeks, when the patient was ‘almost clear’, and at Week 24 the patient was ‘clear’ (Figure 1A). Maintenance therapy for this patient is ivermectin 1% cream twice a week. Prof Schaller clarified that he always recommends a maintenance therapy at a reduced frequency compared with active treatment to help the patient in the long term.
Prof Schaller then described a young female patient (aged 18 years) who presented with severe ocular manifestations (confirmed severe blepharoconjunctivitis), persistent erythema, papules, and pustules. Ocular signs are more often seen in younger patients, particularly children, with cases of undiagnosed severe ocular rosacea more severe in children than in adults. The patient had a 4–5-year history of facial skin problems, had undergone multiple operations for chalazia, and had received systemic antibiotics (specifics unknown) and a variety of creams (including cortisone). Chalazia represents the beginning of ocular rosacea in patients.
Using the ROSCO treatment algorithm (Figure 2), Prof Schaller diagnosed severe inflammatory lesions and moderate persistent erythema. With the treatment aim of ‘clear’, oral doxycycline at 100 mg/day for 3 months followed by 40 mg modified release capsules once daily (QD) was prescribed to treat ocular signs, ivermectin 1% cream QD for inflammatory lesions, and brimonidine as required for erythema (the latter was also the maintenance treatment). At Month 10, the patient was completely ‘clear’ of ocular signs, with papules and pustules completely clearing before then.
Prof Schaller then considered the patient in Figure 1B, who had rosacea with skin and eye involvement since 2014 and had tried many topical treatments with little or no success. The last treatment the patient had tried was doxycycline 50 mg twice daily plus metronidazole from November 2015 to July 2016. Using the ROSCO treatment algorithm (Figure 2), Prof Schaller diagnosed the patient as having severe papules and pustules. Isotretinoin was recommended at the initial consultation but the patient refused, fearing the side effects (Prof Schaller highlighted that at low dosage, these side effects are not likely to be present), and they also refused systemic treatment with doxycycline, but the patient was desperate for a solution.
Again, the treatment aim was ‘clear’ (IGA 0) and ivermectin 1% cream monotherapy QD was prescribed for 12 weeks because this is the only topical treatment that would improve severe inflammatory lesions. As shown in Figure 1B, there was improvement by Week 4, with further improvement at Week 8 and the patient was ‘almost clear’ at Week 12. The patient was asked again at 12 weeks if they wanted doxycycline and this time they agreed. Combination therapy with topical ivermectin and doxycycline 40 mg modified release capsules QD (which has shown superior results to ivermectin plus placebo in a randomised Phase IIIb/IV study) was taken from 12 weeks and complete lesion clearance was seen at Week 21. The patient had not expected a large improvement and was happy with his treatment. Maintenance therapy for this patient is ivermectin 1% cream QD.
The Target is ‘Clear’: Rosacea Consensus Can Help
Prof Schaller concluded that the ROSCO classification, treatment algorithm, and recommendations have simplified the task of effective diagnosis and treatment of rosacea by addressing the multiple features and aiming for ‘clear’.6 A phenotype-based approach could improve patient outcomes to ‘clear’, with ‘clear’ versus ‘almost clear’ being the primary objective because of the extended relapse time and patient quality of life benefits.6,7
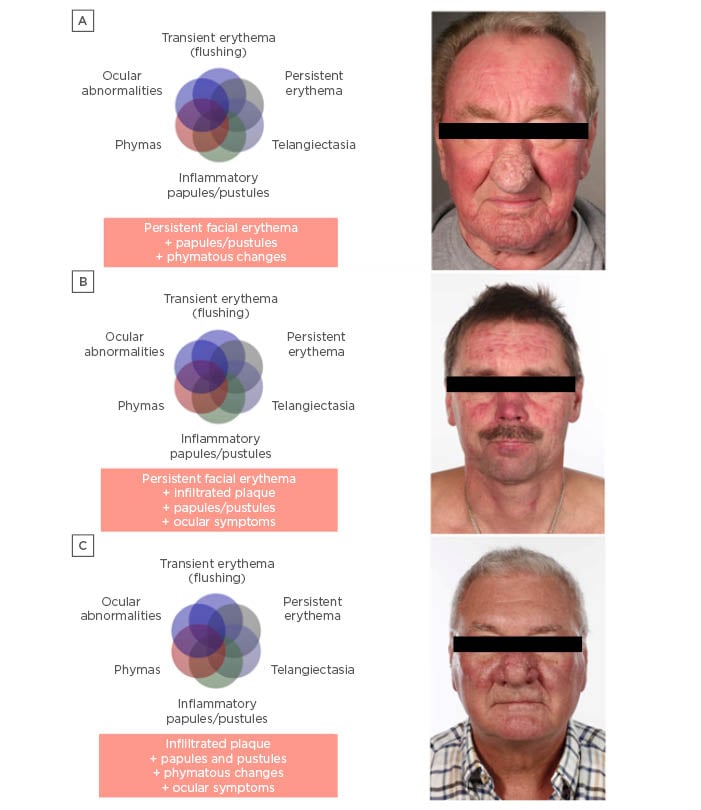
Figure 3: Patients presenting with multiple phenotypes simultaneously.
In each case, the patient was asked which sign they wanted treated first. A) Patient indicated their nose was the main problem; therefore, the patient was prescribed very low dose isotretinoin to treat the phymatous rosacea. After 3–4 months, a discussion would take place about the option to operate to excise the sebaceous glands of the nose. Prof Schaller recommended brimonidine to treat the persistent facial erythema, and ivermectin or metronidazole to treat the papules and pustules. B) Patient had persistent facial erythema for 3–4 months, infiltrated plaque, papules at the lip edges, pustules, blepharitis, and dry eyes. This patient required a combination of different treatments, particularly for the ocular signs. C) Patient had infiltrated plaque, papules, pustules, phymatous changes, and ocular signs and also required a combination of different treatments.
Images provided by Prof Schaller, Tübingen University, Tübingen, Germany, with informed consent from the patients.







