Abstract
A paediatric nail consultation is often required to reduce parents’ concerns regarding their child’s abnormal nail appearance. Nail pigmentation in children is a dermatological challenge because guidelines are not standardised, causing many doubts for dermatologists. In general, the majority of cases of melanonychia are benign in children and nail melanoma cases are very rare. However, alarming clinical and dermoscopic features can be observed, requiring nail surgery to confirm a diagnosis. Here, we present a case of longitudinal melanonychia in a teenager with atypical signs and a good prognosis.
INTRODUCTION
Nail pigmentation represents a dermatological challenge, even for nail experts. The clinical and dermoscopic features of nail pigmentation are different in adults and children, and this aspect is very important for a better evaluation of melanonychia. In children, the majority of melanonychia cases are benign due to a melanocytic nevus or lentigo affecting the nail matrix; nail melanoma cases are very rare. Nevertheless, dermoscopy is a non-invasive method that can be very useful in the evaluation of nail pigmentation. The gold standard for the diagnosis remains histopathology,1,2 which requires an accurate bioptic technique and a trained pathologist in nail diseases. Here, we present a case of longitudinal melanonychia (LM) with a worrying appearance in a young female patient.
CASE REPORT
We report a case of a 17-year-old Caucasian female patient who attended the skin cancer and nail diseases outpatient consultations of the Dermatology Unit of the University of Bologna, Bologna, Italy, for assessment of a band of LM on the first digit of her left hand. She explained that the nail pigmentation had been present since she was 1 year old and her parents, concerned by the atypical appearance of it, decided to escalate the problem and asked for an investigative biopsy. Histopathologic examination revealed that the nature of the lesion was benign. An onychodystrophy remains, with a small erosion of the proximal nail fold.
At time of investigation the patient denied experiencing any kind of pain or other symptoms, but her parents requested an urgent evaluation for the nail band changes, even though they were very slow over time. At clinical examination, we observed the pigmented band of the first digit of the left hand; the band was brown in colour, with longitudinal fissures, a small erosion at the proximal nail fold, and with an interrupted distal margin (Figure 1). The other fingernails were normal. We performed onychoscopy with an ultrasound gel for immersion, using a FotoFinder® dermatoscope (Teachscreen Software GmbH, Bad Birnbach, Germany) for a better visualisation of the band. Specifically, we observed a rectangular form of the band, proximally to distally, which varied in colour from brown to grey-pink, with irregular lines in thickness, spacing, and borders. We magnified the lesion to better observe the proximal nail fold and distal margin.

Figure 1: Longitudinal melanonychia of the first digit of the left hand.
By performing onychoscopy at the proximal nail fold, the lesion showed a small subungual red mass, while the distal margin revealed an interrupted border. No type of pigmentation was present at the hyponychium (Figure 2).
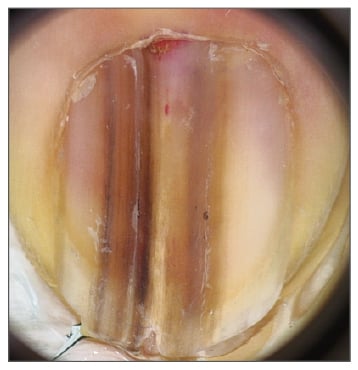
Figure 2: Dermoscopy performed with ultrasound gel.
Investigation showed the presence of a longitudinal band that varied in colour from brown to grey-pink, with irregular lines in thickness and colour, irregular borders, and an interrupted distal margin.
The patient’s parents described how the appearance of the nail slowly changed over time, but they insisted on a new histological examination. We performed a longitudinal nail biopsy, which allowed observation of all nail components; histopathological observation confirmed the presence of individual melanocytes, without atypical features, at the dermoepidermal junction. Melanocytes have the tendency to aggregate in ‘nests’, which is typical of a junctional melanocytic nevus (Figure 3). We suggested a periodic follow-up of the lesion to reassure the parents.
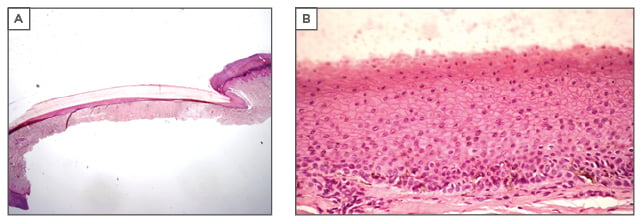
Figure 3: Longitudinal biopsy of the lesion with A) haematoxylin and B) eosin stain.
Individual melanocytes, without atypical features, at the dermoepidermal junction have the tendency to aggregate forming ‘nests’, which are characterised by a junctional melanocytic nevus.
DISCUSSION
Melanonychia in children is less common than in adults and it is burdened by less well-defined criteria concerning diagnosis and management. According to the literature, almost all cases of LM seen in children are benign and nail melanoma is rare. The need for biopsies in childhood melanonychia is under debate because LM in children can show some worrying signs, mimicking the aspect of nail melanoma in adults, such as colour changes with ageing, periungual pigmentation, and variation of the degree of the pigmentation.
Epidemiology
The epidemiology of melanonychia in children is described as more prevalent among races with higher skin pigmentation than Caucasians, with a mean age of onset of 3 years and no difference in sex. The fingernails are more commonly affected than the toenails, and in the fingernails the most affected digit is the first, with a longitudinal pigmented band typically seen within the nail plate, running from the proximal to distal nail plate. In populations with melanin-rich skin, such as African-Americans, 77% of children with LM have a melanonychia caused by melanocytic activation, which is a process that displays racial variation.3 In contrast, in Caucasians and populations with lower levels of melanin in the skin, the presence of pigmented streaks in children is typically caused by melanocytic proliferation. Benign melanocytic hyperplasia is diagnosed in 30% of children with LM and nevus of the nail matrix in 48%;3,4 no cases are reported in Chinese children,5 while 2.5% of black children aged <4 years present with melanonychia.6 An interesting study of melanonychia in childhood was recently published, including a series of 30 children who showed 20 cases of lentigo, 5 of subungual nevus, and 5 of melanocytic hyperplasia, all histologically confirmed.7
Clinical and Dermoscopic Aspects
Clinical presentation of childhood melanonychia consists of a longitudinal band, which can be both transversal or total, involve one or more digit, and appear at any age. The clinical appearance of a melanonychia varies due to the underlying process, based on the concept that in children, as in adults, nail matrix melanocytes are inactivated, and, when triggered, undergo activation or proliferation. If one digit is affected, we can assume a proliferative process. Usually, the clinical appearance is a longitudinal pigmented band. The aspect of the band can be very different; for example, the colour may be pronounced and homogeneous, the borders can be well defined or less sharp, and the width can range from a few millimetres to the entire nail plate. The corresponding nail plate can show some changes or be normal. A brown-black periungual pigmentation, known as Hutchinson’s sign, can be either present or not. When multiple nails are involved in melanonychia, we can consider this due to a normal racial genetic variant, particularly in populations with melanin-rich skin, or we can classify it as a complex syndrome, such as Peutz–Jeghers syndrome and Laugier–Hunziker syndrome.
In Peutz–Jeghers syndrome, pigmented macules on the oral mucosa, lips, fingers, and toes, and melanonychia are associated with intestinal polyposis with a possible malignant degeneration. In Laugier–Hunziker syndrome, LM affects several nails and is associated with pigmented macules of the lips, mouth, oesophageal mucosa, and genitalia. Other causes of melanocytic activation in children are trauma, irradiation, or drugs, and this type of melanonychia is usually located on the thumbs and index fingers. In terms of medications for this condition, we have reported doxorubicin or hydroxyurea use,8,9 as well as minocycline, zidovudine for antiretroviral therapy in HIV patients, antimalarials, or cancer chemotherapeutics.10,11
A dermoscopic pattern that suggests a melanocytic activation is a grey background of the band, with thin, grey-coloured, regular, and parallel lines. When considering conditions in a child other than a melanonychia of a single nail, a nail matrix nevus, which can be congenital or acquired, is the most likely diagnosis. Nail matrix nevi occur more frequently in fingernails than in toenails, most often in the thumb, and they present with one or more longitudinal heavily pigmented band. The width of the band may vary in size and colour; in particular, the pigmentation may be homogeneous and dark.2 In addition, >50% of cases of nail matrix nevi measure >3 mm.1,3 Dark bands are associated with pseudo-Hutchinson’s sign because the dark nail plate pigmentation is visible through the transparent nail fold.
As previously discussed, there are a lot of clinical and dermoscopic aspects in children that can be alarming for the clinician, such as in our reported case. For example, a periungual pigmentation, Hutchinson’s sign, is typical in congenital nevi, and a gradual enlargement of the band can also be observed. The band can become darker and spread throughout the nail, or thinning and fissuring can occur. In children, it is also common to observe a gradual fading of the band;12 fading of the pigmentation, called ‘regressing nevoid nail melanosis in childhood’, is unique to children and is not always indicative of regression of the nevus, but can indicate decreased melanocytic activity from nevus cells.13
The presence of dots on onychoscopy, distributed along melanocytic lines, is a new sign indicating regression of the LM. In an interesting study analysing this indication,14 the authors suggested that the dots are an accumulation of melanin derived from a cluster of nevus cells that migrate upward from the dermoepidermal junction. Dermoscopically, they are black in colour with a regular size and shape from round to oval (<0.1 mm) and are regularly distributed along the lines or within the pigmented lines until they interrupt the lines. In most young patients, the dots disappear over time, together with the fading of melanonychia. According to the authors, these dots represent a sign of regression of a nevus and are not a warning sign of melanoma.14 However, the dermoscopic pattern of a nevus shows the presence of a brown background with longitudinal brown-to-black regular and parallel lines, with regular spacing and thickness. Pathologically, most of the nevi in children are junctional nevi with regular nests and typical melanocytes, but the features between the lesions can be different and the differential diagnosis by a dermatologist requires more experience in nail histopathology.
As mentioned, nail melanoma in children has been described in only 12 cases. Of these, 8 reports were in Japanese children,15,16 2 were from South America (one from Argentina and one from Brazil),14 and 2 cases were in Caucasians.17 LM is the most frequent manifestation, with a dark-brown-coloured band and the presence of Hutchinson’s sign.18 In general, these cases of melanoma were in situ of the nail apparatus. In all these pigmented nails, there was either a process of evolution or regression.
Management
The real challenge for nail experts remains whether a benign lesion appearing in childhood can become a malignant lesion in adulthood. Dermoscopic patterns that suggest a melanoma in children can also be seen in LM, and their specificity in a young age is very low; a brown background with longitudinal brown-to-black lines, with an irregular degree of colour pigmentation, spacing, or varying thickness and ending abruptly, or a parallelism disruption, can be observed.
We recommend the examination of all aspects of a melanonychia in children when involving a single digit.1 In our experience, the clinical features of melanonychia in children are the same as in adults, but the most important difference is the extreme variability of the dimensions, degree of the pigmentation, and distribution of the pigment, which evolve differently over time. All these characteristics should not cause concern for the clinician when the patient is a child.
CONCLUSION
The consensus of melanonychia management in children is still under debate and a standardised process is required. After reviewing the literature, the risk of melanoma is remote, while the risk of a permanent nail dystrophy due to nail biopsy can occur;19 thus, a decision should be made that considers both the anxiety of the parents and the experience of the clinician. In fact, it is important to emphasise that paediatric nail consultation is mostly used to reassure worried parents about the aspects of their child’s nail and also to manage the condition using personal experience of melanonychia in children, or refer the patient to nail experts in doubtful cases.
Criteria suggesting biopsy requirement in children should include the speed at which the band grows and the colour of the band; longitudinal excision is the best surgical option in biopsy cases.20 However, these features can also be seen in nail matrix nevi in children; therefore, their specificity to a particular condition is low. According to the literature, dermoscopy enhances the clinical evaluation of LM, improving the management and allowing a follow-up consultation due to electronic storage of the clinical and dermoscopical images. Moreover, dermoscopy allows clinicians to visualise the site of the pigment production, with the observation of the distal margin and the presence of the melanic deposition within the nail plate. In conclusion, we recommend periodic follow-up of the patient and management using clinical and dermoscopic pictures to inform the decision as to whether a nail biopsy should be performed after puberty.13







