Abstract
Background: Basal cell carcinoma (BCC) is a type of skin cancer. It typically develops in areas exposed to the sun, such as the face, neck, and hands. BCC usually appears as a raised, pearly bump with a central depression, or as a flat, scaly reddish patch. There are several types of BCC, and when melanin is present in the lesion it is called pigmented BCC, which are the types the authors are reporting in this case series.
Aim: The aim of this study is to create awareness regarding a long-standing lesion turning into malignancy and to also alert health professionals for identification of signs and symptoms of BCC and the need for an early diagnosis.
Method: A prospective observational study was carried out on patients presenting with pigmented variants of BCC.
Conclusion: These cases highlight the importance of thorough clinical examination and biopsies supported by histopathological analysis aiding in diagnosis.
Key Points
1. Basal cell carcinoma (BCC) is a prevalent malignant skin cancer primarily affecting sun-exposed areas, leading to significant morbidity, recurrence, and potential tissue destruction.2. This is a prospective observational study of five cases of pigmented BCC at a dermatology outpatient clinic, focusing on clinical presentation, histopathology, recurrence, and treatment outcomes.
3. Early recognition and treatment of pigmented BCC, including tailored therapies and photoprotection, are critical in preventing recurrence and improving patient quality of life.
INTRODUCTION
Basal cell carcinoma (BCC) is a heterogeneous malignant neoplasm and can cause great morbidity as most occur in highly visible areas of the body, often relapse, and may invade and destroy local tissues.¹ Pigmented basal cell carcinoma can resemble a melanoma clinically.² Fair skin and chronic UV B exposure are the most important risk factors.³ Individual risk factors for BCC include age, male sex, race, phenotypic characteristics, and genetic predisposition.⁴ BCC can appear in both pigmented and non-pigmented forms, each showing distinct dermoscopic characteristics. Different subtypes of BCC have specific dermoscopic criteria. The primary challenge is distinguishing superficial BCC from other subtypes, as this distinction can influence the course of treatment.⁵ Upon analysing demographic groups, it was determined that, after accounting for age and race, the rate of BCC in male patients was 1.7 times higher than in female patients. In terms of age, individuals aged 65 years and older faced an elevated risk of developing BCC during the study period. White individuals had the highest risk, with adjusted incidence rates 8–70 times greater than those seen in individuals who were Asian, Black, or Hispanic. The group at the highest risk was White individuals aged 80 years and above, who saw the largest increase in BCC incidence, with an estimated average annual percentage change (APC) of 2.23%.⁶
METHOD
A prospective observational study was carried out on patients presenting to the Department of Dermatology outpatient clinic with pigmented variant of BCC. Clinical photos were taken only after oral and written consent of the patients.
CASE 1
A 60-year-old female patient, a known diabetic and hypertensive, presented with complaints of generalised pain all over the head and body for the past 2 months. She also had two black-coloured, rough-looking lesions on her face. The patient first noticed a small, raised lesion on the medial side of the right eyelid just medial to the right eyebrow 3 years ago. For the past 1–2 years she noticed an increase in size of the lesion and slight pain and discomfort while dressing or rubbing against the lesion.
Dermatological Examination
The patient had three well-defined, annular, hyperpigmented ulcers measuring about 2×1 cm with rolled-up edges and central depression. One located at the medial canthus of the right eye, the other at the lateral side of the right eyebrow, and ther third one over the left auricle (Figure 1A).
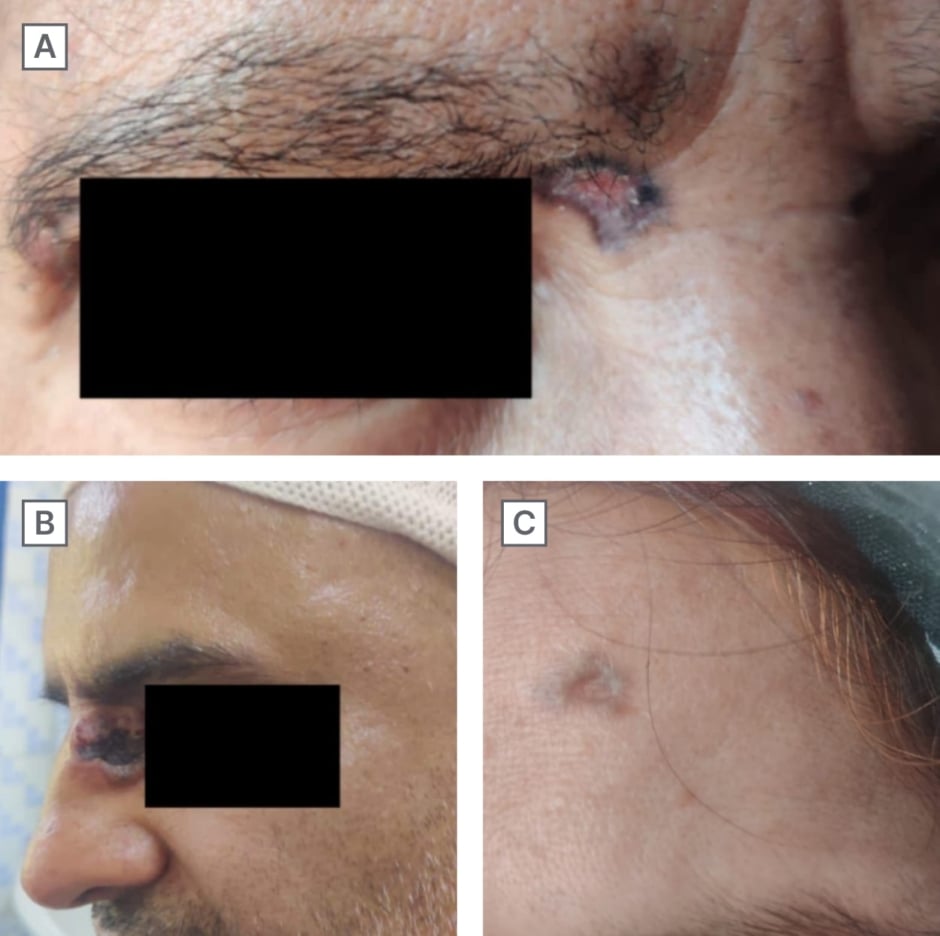
Figure 1: Cases 1, 2, and 3.
A) Case 1. B) Case 2. C) Case 3.
A biopsy was done, and it revealed a stratified squamous epithelial epidermis, showing a focal downward extension of the Basal cell. The extension showed peripheral palisading with increased pigmented dermis. Focal lymphocytic inflammatory cell infiltrate was also seen. The probable diagnosis was suggestive of an atypical BCC lesion. She was started on 5% flourouracil cream at night and tacrolimus 0.1% cream in the morning for a period of 8 months. Photoprotection was also advised, for which the patient’s lesions appeared to be improved.
CASE 2
A 40-year-old male patient with a known case of diabetes presented with a complaint of mild itching on his nose. He had undergone surgical excision for BCC 3 months ago. Three months after the surgery, the patient reported to us with lesion at the same site of excision associated with itching and discharge. The discharge was seropurulent.
Dermatological Examination
On examination, the patient had a well-defined hyperpigmented ulcer present at the left medial canthus of the eye with rolled-up margins, measuring 4×3 cm in size. Blood and scabbing were also observed at the site of the lesion on examination (Figure 1B).
The probable diagnosis was suggestive of a BCC lesion. Further, an excisional biopsy was done and a histopathological report was suggestive of an BCC lesion. Given recurrence, post-excisional biopsy, the patient was started on a 150 mg tablet of vismodegib once a day for about 4 months and was also advised radiotherapy.
CASE 3
A 54-year-old female patient presented with complaints of a scar on the left side of her forehead. The patient first noticed blackish discolouration on her forehead 5 months previously, which progressed to a black ulcerated scar on the left side of her forehead and was increasing in size.
Dermatological Examination
The patient had a well-defined, hyper-pigmented (blackish) patch measuring about 1×1 cm, with irregular borders and central ulceration (Figure 1C).
Further, an excisional biopsy was done, and the histopathological report was suggestive of an atypical BCC lesion. After excisional biopsy, the patient was put on topical tacrolimus 0.1% and photoprotection was advised.
CASE 4
A 57-year-old female patient presented with complaints of a black lesion over the left side of her back for the past 5 years that was increasing in size.
Dermatological Examination
On examination, the patient had a well-defined, hyper-pigmented nodule that was 4x3x3 cm in size with one ulcerated edge on the left side of the infrascapular region (Figure 2A).
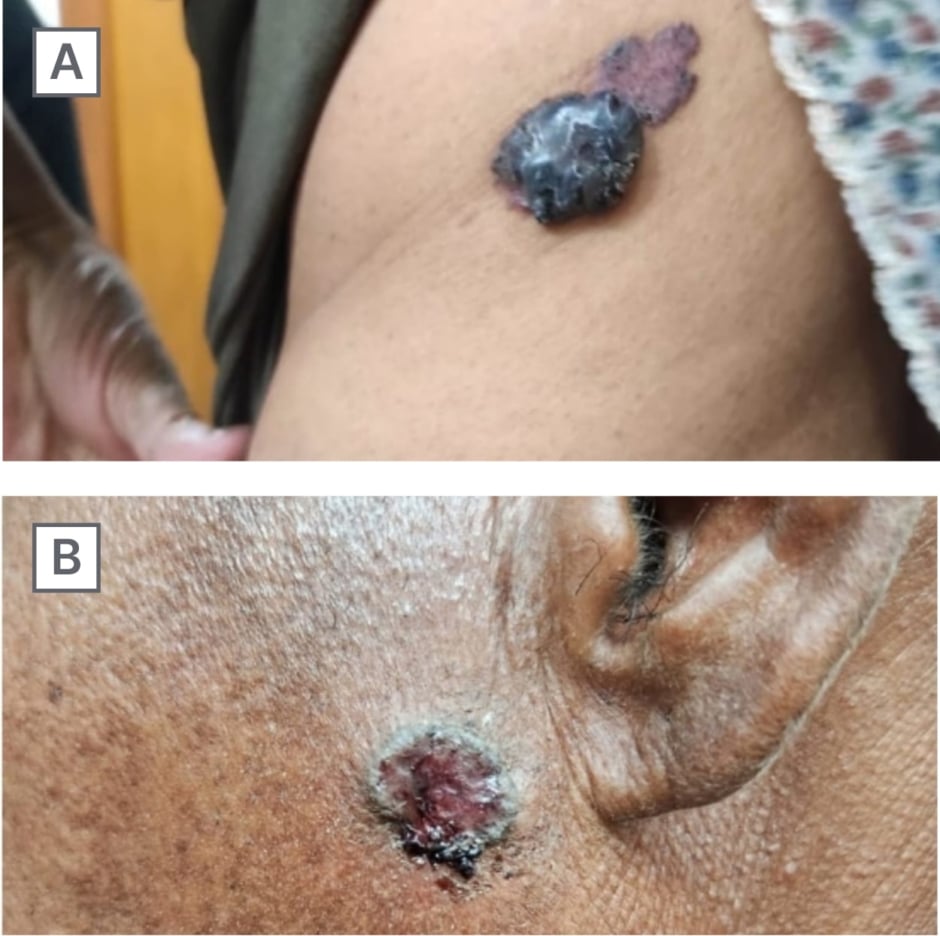
Figure 2: Cases 4 and 5.
A) Case 4. B) Case 5.
An excisional biopsy was done, and histopathological examination showed multiple fragments of a tumour composed of monomorphic basaloid cells arranged in sheets, nodules, cords, and anastomosing trabeculae. Some nodules showed peripheral palisading. Intervening stroma showed hyalinisation and focal fibromyxiod change. Epidermis showed hyperkeratosis with extensive crusting and flattening of rete ridges with pigmented dermis (Figure 3). The diagnosis was suggestive of BCC and excisional biopsy was then done.
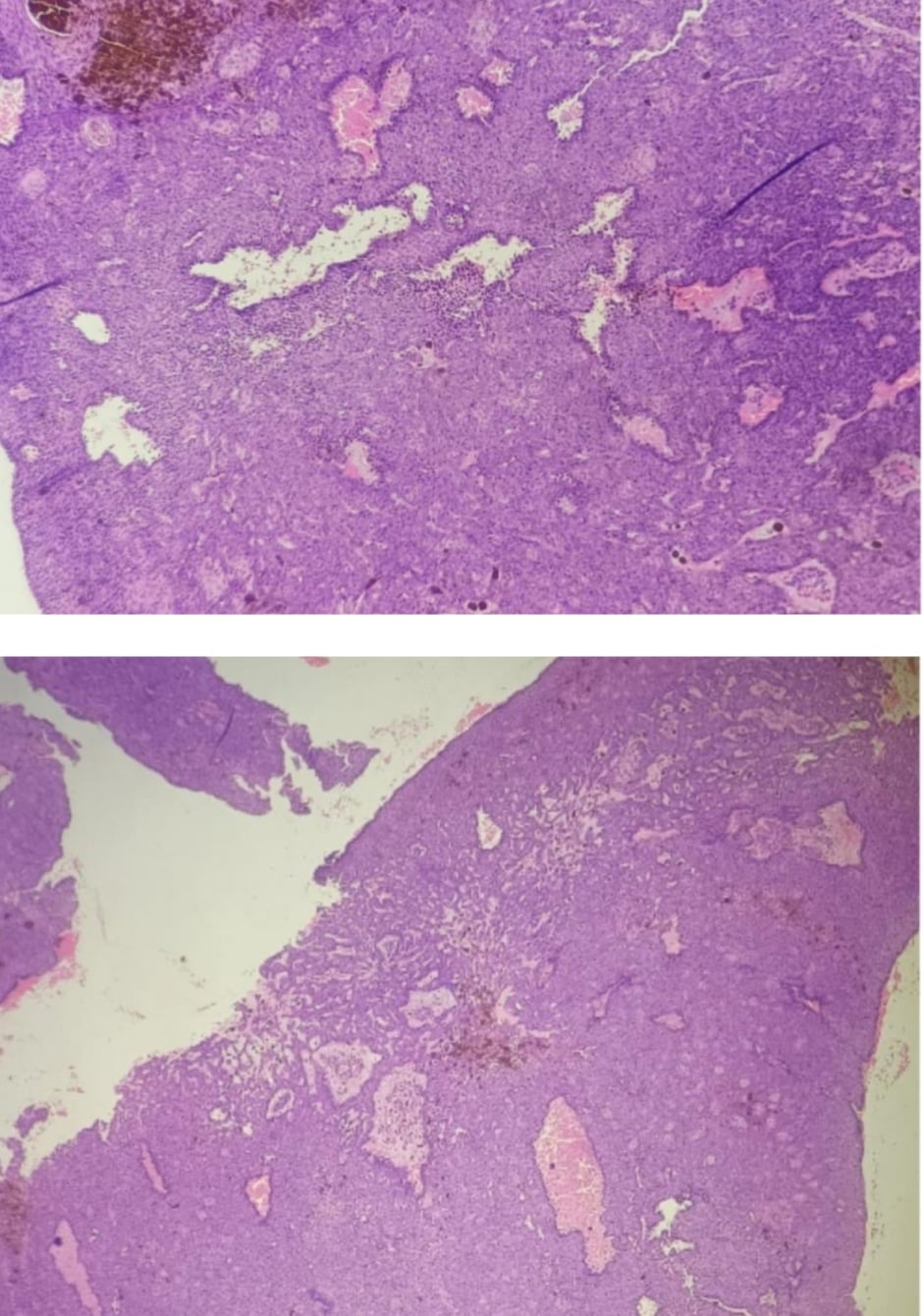
Figure 3: Biopsy image suggesting pigmented basal cell carcinoma.
CASE 5
A 44-year-old male presented with complaints of a lesion on the left side of his face for the past 8 months that was associated with itching and a burning sensation. The patient also complained of occasional bleeding from the lesion.
Dermatological Examination
On examination, the patient had a solitary ulcer that was 3×3 cm in size and annular in shape with hyperpigmented margin and few haemorrhagic crusts present (Figure 2B). Biopsy was suggestive of pigmented BCC. After the excisional biopsy, the team advised photoprotection and chemotherapy for the patient.
RESULTS
Among the five cases of pigmented variants of BCC described in this study, the authors have found some important results.
- Gender: The majority of pigmented variants of BCC were in females (60%), with a female to male ratio of 3:2.
- Age: The majority of the authors’ cases were of patients in their 40s or 50s (mean age: 51 years).
- Site: The most common site was on photo exposed area (i.e., face [80%]), among which, lesions near to the medial canthus were present in two cases (40%).
- Recurrence: Recurrence was present among two cases of the study with lesions near the medial canthus of the eye (40%). The cause of recurrence in these cases of BCC was likely due to sunlight exposure and not related to occupational factors.
- Comorbidities: Two cases were known diabetic and one case was hypertensive.
- Type of pigmented variety: Three patients had multiple grey-blue globule features constituting to 60%, and the other two cases had large grey-blue ovoid nests with maple leaf-like structures.
DISCUSSION
BCCs are common skin cancers that tend to appear on sun-exposed skin. They were essentially a molecular ‘black box’ until 2008, when identification of a genetic flaw in a rare subset of patients who have a great propensity to develop BCCs pointed to aberrant Hedgehog signalling as the pivotal defect leading to formation of these tumours.⁷
Nodular, superficial, morpheaform, and a combination of these subtypes of BCC may be seen. When melanin is present in the tumour it is called pigmented BCC, as seen in the authors’ cases.⁸ This case series reported on pigmented BCC, but the clinical presentation of each case differed from the ulcerative superficial type to the nodular type. Diagnosis was made based on clinical features and histopathological examination of the lesion. Pigmented BCC presents as black papules or nodules. Its morphologic appearance can mimic that of a melanoma.⁹ Skin biopsy is essential to confirm the diagnosis and evaluate the risk of recurrence.¹⁰
Histologically, nodular BCC is identified by nodular clusters of basaloid tumour cells that extend from the epidermis into the underlying dermis, frequently exhibiting peripheral palisading at the edges of the tumour nests. In pigmented BCC, pigment is found within the tumour cells, within melanophages in the surrounding dermis, or in both, which accounts for the tumour’s black coloration.² To diagnose pigmented BCC, it must lack the negative feature of a pigment network and must present at least one of the following six positive features: large grey-blue ovoid nests, multiple grey-blue globules, maple leaf-like structures, spoke wheel areas, ulceration, or arborising ‘tree-like’ telangiectasia.¹¹
Treatment depends on various factors, such as tumour size, location, and histological subtype. While excisional surgery is the preferred method for most common types of BCC, various nonsurgical treatments are also available. These include photodynamic therapy,¹² as well as topical treatments like imiquimod cream, 5-fluorouracil, and ingenol.¹³ As in Case 1, the team treated the patient with 5-Fluorouracil, tacrolimus, and photoprotection post biopsy, and later advised Mohs surgery. The importance of skin cancer screening in immunosuppressed patients, particularly transplant recipients, should be emphasised, as they are at higher risk for squamous cell carcinoma (SCC). Regular screening is vital for early detection, as studies have highlighted the prevalence of skin cancers in renal transplant recipients and the need for early cancer screening in this population.¹⁴
In solid organ transplant recipients, BCCs are now more common than SCCs, with a BCC:SCC ratio of 1.7:1 compared to the previous 1:3 ratio favouring SCC. This emphasises the need for thorough screening for both BCC and SCC.¹⁵
Long-term follow-up and monitoring are essential due to the potential for recurrence and the risk of developing additional skin cancers. Patients should be educated on sun-protective measures, such as the use of sunscreen, protective clothing like wide-brimmed hats, and regular self-examination of the skin.
CONCLUSION
BCC is the most common form of cancer worldwide, and the incidence of this cancer is increasing due to prolonged exposure to sun and ageing adults with cumulative sun damage. This study highlights the presentation of pigmented variant of BCC, and the authors have analysed the demographics of BCC in terms of age, gender distribution, localisation, recurrence, and treatment. An early diagnosis and adequate treatment of this not so uncommon skin cancer will prevent associated morbidity and improve the patient’s quality of life.






