Abstract
Cutaneous angiosarcoma is a rare and aggressive malignancy. This case highlights its unusual presentation following a scald burn, emphasizing the importance of early detection and the challenges in management. A 66-year-old male presented with progressive erythematous plaques on his scalp and face following a scald burn. Examination revealed indurated, violaceous patches with satellite nodules. Histopathology confirmed cutaneous angiosarcoma. Imaging showed extensive local invasion. The patient declined further treatment, and the disease progressed rapidly. Clinicians should maintain a high index of suspicion for angiosarcoma in non-healing post-traumatic lesions. Early biopsy and multidisciplinary management are crucial.
Key Points
1. Cutaneous angiosarcoma is a rare and aggressive malignancy originating from blood or lymphatic vessels, often affecting elderly Caucasian males. Trauma, such as scald burns, may rarely predispose individuals to its development.
2. This case study details a 66-year-old male presenting with extensive erythematous plaques following a scald burn, later diagnosed with cutaneous angiosarcoma through biopsy and imaging. Despite aggressive local progression, the patient declined treatment, highlighting ethical dilemmas in patient autonomy.
3. Early detection through suspicion and biopsy is critical in managing cutaneous angiosarcoma, especially in unusual presentations like post-burn lesions. Multidisciplinary collaboration is essential for treatment planning, considering factors like advanced age and patient preferences, which may influence therapeutic decisions and outcomes.
INTRODUCTION
Angiosarcoma is a rare and aggressive malignant neoplasm that arises from endothelial cells of blood or lymphatic vessels, accounting for approximately 1–2% of all soft tissue sarcomas.1 This malignancy predominantly affects older adults, with a higher incidence observed in elderly Caucasian males.2 Primary cutaneous angiosarcoma typically presents as solitary or multifocal ecchymotic lesions, most commonly affecting the face, scalp, or neck.2,3 Several risk factors have been associated with its development, including chronic lymphedema, prior exposure to ionizing radiation, environmental carcinogens such as vinyl chloride and arsenic, and immunosuppression.1-3 Due to its aggressive nature and high metastatic potential, angiosarcoma is associated with a poor prognosis, particularly in cases where diagnosis and treatment are delayed.4
The authors present a case of biopsy-confirmed angiosarcoma in a 66-year-old male who exhibited characteristic cutaneous lesions but declined treatment despite a multidisciplinary management approach. This case highlights the diagnostic challenges of angiosarcoma, the importance of collaborative care in treatment planning, and the ethical considerations surrounding patient autonomy in medical decision-making. Four months after diagnosis, the patient died, emphasizing the critical role of early detection and timely intervention in improving survival outcomes. This case underscores the need for heightened clinical awareness and patient education to facilitate early diagnosis and optimize treatment strategies for angiosarcoma.
CASE SUMMARY
A 66-year-old male presented with a six-month history of progressively enlarging erythematous plaques on the left cheek, originating from a scald burn caused by splashed cooking oil. A few weeks after the burn, the patient noted the sudden appearance of a painless bruise-like lesion on the left cheek, associated with minimal brownish discharge. Two months later, the lesion gradually extended to involve the entire left face and scalp, accompanied by induration, hemorrhagic crusting, and severe pain that the patient rated 8/10. The patient self-medicated with thimerosal tincture and herbal washes, which proved ineffective. Initial consultations led to a diagnosis of an infected wound, and management included oral and intravenous antibiotics, as well as debridement. A biopsy was then performed and revealed only acute and chronic inflammation. Despite these interventions, the lesions persisted and progressively worsened. A referral to a private dermatologist prompted reevaluation, leading to the recommendation for a repeat biopsy.
The patient’s family history was non-contributory. There were no similar lesions in the family, nor any history of malignancies. The patient had no prior history of skin cancer, immunosuppression, or any known risk factors for cutaneous angiosarcoma.
A cutaneous examination revealed multiple well-defined, irregularly shaped erythematous plaques with extensive ulcerations, serosanguineous discharge, and hemorrhagic crusts. These lesions were predominantly located on the left side of the face, extending to the anterior scalp, left periorbital region, and left preauricular area, with several satellite lesions noted on the right frontal, temporal, and maxillary regions (Figure 1). Dermoscopy findings were nonspecific, revealing structureless red-to-violaceous or bluish areas interspersed with small yellow globular structures.

Figure 1: Extensive ulcerated angiosarcoma of the face and scalp.
Erythematous plaques with extensive ulcerations, serosanguineous discharges, and hemorrhagic crusts on the left side of the face extending to the left anterior scalp, the left periorbital area, and the left pre-auricular region. Several satellite foci are seen on the right frontal area, right temporal, and maxillary area.
Three months after the first biopsy, a repeat incision biopsy was done and revealed irregular, anastomosing vascular channels filled with erythrocytes, some of which were lined by atypical large endothelial cells infiltrating between collagen bundles. Marked extravasation of erythrocytes was observed, along with diffuse lymphocytic infiltrates and atypical pleomorphic cells, some displaying darkly staining nuclei, while others exhibited abundant cytoplasm with vesicular nuclei and prominent nucleoli. A few cells demonstrated a spindle-shaped configuration. These atypical cells were predominantly located in the papillary dermis in a diffuse pattern, with extension into the deeper dermis and infiltration between collagen bundles (Figure 2A-D). Immunohistochemical analysis showed positivity for CD31 (Figure 3A) and CD34 (Figure 3B).
A contrast-enhanced CT and angiography of the head demonstrated a multifocal, ill-defined, extracranial superficial enhancing mass predominantly involving the left side of the head. The lesion was closely associated with the temporalis muscle and the anteroinferior aspect of the globe, receiving vascular supply from branches of the external carotid artery, including the posterior auricular, superficial temporal, and facial arteries. Additional smaller lesions were observed in the right frontal, temporal, and parietal regions (Figure 4). No cervical lymphadenopathy was detected bilaterally. Metastatic evaluation, including chest and abdominal radiography as well as liver ultrasonography, yielded negative findings.
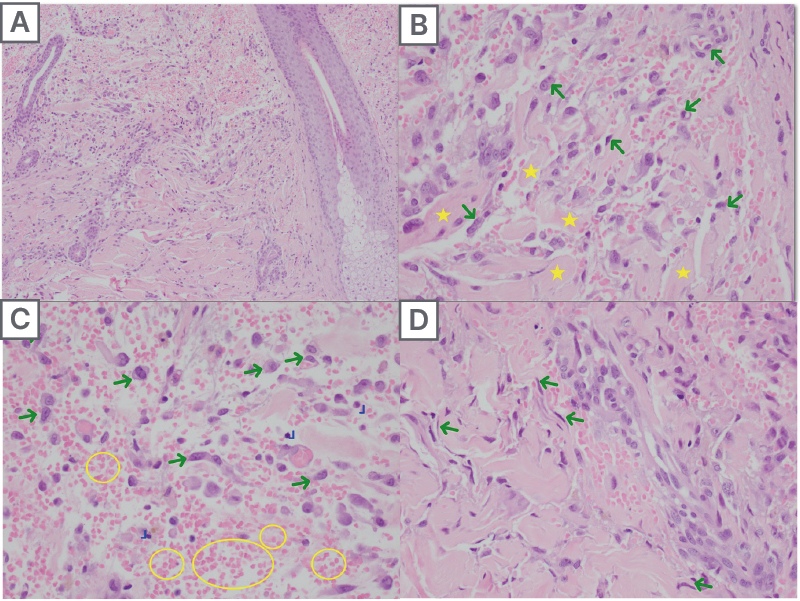
Figure 2: Hematoxylin and eosin stain
2A) Crack-like vascular spaces between collagen bundles. 2B) Irregular anastomosing vascular channels lined by atypical large endothelial cells (green arrows) with conspicuous dissecting of collagen (yellow stars). 2C) Marked RBC extravasation (yellow circles) admixed with lymphocytes (L) and atypical pleomorphic cells (green arrows). 2D) Spindle-shaped atypical endothelial cells (green arrows).
RBC: red blood cells.
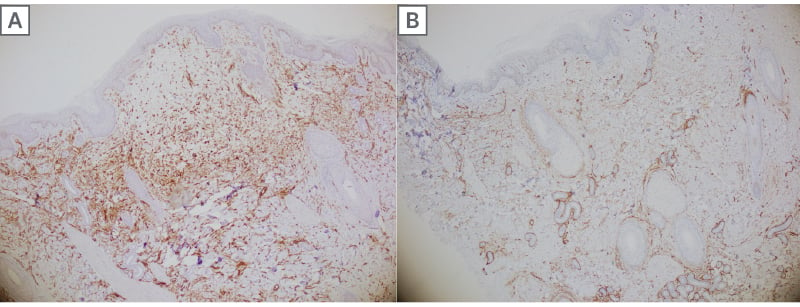
Figure 3: Immunohistochemistry
3A) CD31 stained the atypical large pleomorphic cells and endothelial cells of the blood vessels. 3B) CD34 stained the atypical endothelial cells of the blood vessels highlighting their proliferation in the dermis while dissecting collagen bundles.
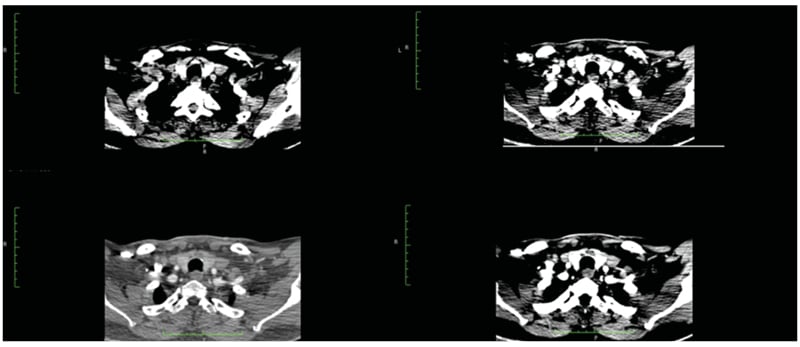
Figure 4: CT images of the lesion
The diagnosis of cutaneous angiosarcoma was confirmed through clinical, histopathological, and imaging findings. Due to the extensive size and critical location of the tumor, involving the scalp, face, and periorbital region, a multidisciplinary team comprising dermatologists, plastic surgeons, medical oncologists, and ophthalmologists was assembled to manage the case. The multidisciplinary meeting led to the proposal of neoadjuvant chemotherapy with paclitaxel to reduce the tumor size, followed by a definitive wide excision and reconstruction. However, after chemotherapy was suggested, the patient declined all forms of medical and surgical treatment. The decision was influenced by financial constraints and concerns about his advanced age. Socioeconomic factors, including the cost of cancer treatment and limited access to specialized care, played a critical role in the patient’s reluctance to proceed with therapy. Despite detailed counseling on the aggressive nature of angiosarcoma and the potential benefits of treatment, the patient chose not to proceed with the proposed management plan.
In the months following the diagnosis, the patient experienced rapid tumor progression and a significant decline in functional status. Despite the provision of symptomatic management and palliative care, the patient’s condition continued to deteriorate, culminating in death within four months of the initial diagnosis.
DISCUSSION
Angiosarcoma, a rare and aggressive malignant neoplasm of endothelial origin, arises from blood or lymphatic vessels and is characterized by uncontrolled endothelial cell proliferation. Representing less than 2% of all soft tissue sarcomas, angiosarcoma predominantly affects adults and elderly individuals.1,2 Cutaneous angiosarcoma, the most common subtype, typically manifests as solitary or multifocal bruise-like patches or plaques, most often involving the face, scalp, or neck regions.2,3 It occurs more frequently in older men and shows a marked predilection for the head and neck areas, particularly the Wilson-Jones type, which represents less than 0.1% of all head and neck cancers.5
Cutaneous angiosarcoma of the scalp and face is rare, and its occurrence following burn trauma is even more uncommon. This case underscores the rarity of cutaneous angiosarcoma arising from a scald burn, a phenomenon rarely reported in the Philippines. While burns have been associated with the development of malignant neoplasms such as squamous cell carcinoma, basal cell carcinoma, and melanoma,6,7 this represents the first documented case of cutaneous angiosarcoma emerging from a scald burn in the country.
Existing literature suggests that trauma, including burns, may contribute to the development of angiosarcoma,8 although the precise pathophysiological mechanisms remain poorly understood. Several studies have reported cases of angiosarcoma arising in areas subjected to prior trauma or chronic inflammation.8-10 Several studies have proposed that burn-induced trauma may facilitate the development of this malignancy by promoting chronic inflammation, angiogenesis, and abnormal vascular proliferation in the affected tissue.11,12
The differential diagnosis of cutaneous angiosarcoma includes various conditions that may mimic its clinical presentation, such as inflammatory disorders like rosacea, erysipelas, and cellulitis, as well as allergic reactions, arthropod bites, or bruises. For example, a 70-year-old male with worsening facial edema, initially suspected to be due to an infection, was ultimately diagnosed with cutaneous angiosarcoma following biopsy.13 Similarly, a 75-year-old male presenting with persistent erythematous patches on the face, initially misdiagnosed as rosacea, was later diagnosed with cutaneous angiosarcoma after the lesions progressed to purpura and violaceous plaques.14 The variability in clinical presentation often leads to delays in diagnosis.
As highlighted by Asgari et al.15 the Head-Tilt Maneuver, where the patient tilts their head below heart level for 5-10 seconds, can be a useful diagnostic tool for vascular neoplasms like cutaneous angiosarcoma. This maneuver increases vascular engorgement and enhances the violaceous appearance of the lesion, helping to define tumor borders and identify skip areas, which is crucial for surgical planning. Early diagnosis is essential, as untreated cutaneous angiosarcoma can rapidly progress, infiltrating surrounding tissues and leading to complications such as edema, ulceration, and hemorrhage. At the time of diagnosis, the average tumor size is typically 3–5 cm.16
The rarity of cutaneous angiosarcoma is reflected in the limited number of case reports available in the literature. The occurrence of cutaneous angiosarcoma following a burn injury, as observed in the authors’ patient, is exceptionally uncommon. Bhatti et al.8 reported a case of a 91-year-old female who developed pruritic red patches on her scalp following a burn from a salon hair dryer. Despite various clinical diagnoses and treatments, the lesion progressed into a large purplish mass with persistent bleeding. An incisional biopsy confirmed the diagnosis of angiosarcoma, exhibiting a similar presentation to the current case of cutaneous scalp angiosarcoma following a burn.
A comprehensive diagnostic workup, including biopsy and imaging, is crucial for the accurate diagnosis of cutaneous angiosarcoma. Imaging is essential to assess the extent of the lesion and rule out metastatic disease. MRI is the preferred modality for evaluating localized disease, as it provides superior soft tissue contrast, aiding in the assessment of tumor extent and involvement of adjacent tissues. CT is primarily utilized to detect metastatic disease and monitor treatment response, especially in organs such as the lungs and liver. Imaging findings should be interpreted in conjunction with the patient’s clinical history and demographics, and biopsy remains critical for a definitive diagnosis.16
Biopsy is essential for confirming the diagnosis of angiosarcoma, with histopathological examination typically revealing vessel-like structures forming anastomosing networks, cellular atypia, mitotic figures, and multilayered endothelial lining. In poorly differentiated areas, the tumor may display sheet-like growth patterns, often accompanied by hemorrhage and necrosis. Immunohistochemical staining with endothelial markers such as CD34, CD31, von Willebrand factor, Ulex europaeus agglutinin 1, and vascular endothelial growth factor plays a critical role in further confirming the diagnosis. In this case, both CD31 and CD34 stains were positive, which conclusively confirmed the diagnosis of angiosarcoma.17
The definitive management of angiosarcoma requires surgical intervention to achieve an oncologically appropriate margin. A multidisciplinary approach, combining surgery, radiation, chemotherapy (e.g., paclitaxel), and immuno-oncology agents, is essential for optimal treatment. Radiation therapy is employed for residual disease or when surgical resection is not feasible, while chemotherapy may be used to reduce tumor size or manage advanced disease. In cases of unresectable cutaneous angiosarcoma, treatment options include radiation, chemotherapy, palliative surgery, or supportive care to alleviate symptoms. Palliative care plays a critical role in enhancing the patient’s quality of life, as the prognosis for advanced cutaneous angiosarcoma remains poor.1,18,19
Socioeconomic and psychological factors also significantly influence treatment decisions in cutaneous angiosarcoma. Financial constraints, limited access to specialized care, and treatment costs can delay diagnosis and impact adherence. Psychological distress, fear of disfigurement, and lack of social support may also lead patients to decline aggressive treatments.
In this case, the patient was diagnosed with cutaneous angiosarcoma involving extensive areas of the scalp, face, and surrounding structures, making the disease locally advanced and unresectable. The rapid progression of the large tumor rendered surgical intervention unfeasible, and the treatment plan shifted to focus on radiotherapy to control local growth and alleviate symptoms. Chemotherapy with paclitaxel was also initiated to reduce the tumor size. Additionally, palliative care was considered to manage symptoms, as the patient expressed reluctance toward aggressive treatments. Despite these interventions, the prognosis remained poor, given the aggressive nature of the disease and the advanced stage at presentation.
The overall prognosis for scalp angiosarcoma is generally unfavorable, primarily due to its aggressive nature, high likelihood of local recurrence, and metastasis. Prognostic factors associated with a poor outcome include being over 70 years of age, a tumor size greater than 5 cm, and the tumor being located on the head or scalp. As noted by Pawlik et al.19 cutaneous angiosarcoma typically follows a rapidly fatal course, particularly when diagnosed at advanced stages.
In the case of the authors’ patient, the challenge in diagnosing cutaneous angiosarcoma, due to its deceptive clinical presentation, coupled with the progression to an advanced stage before detection, reflects these observations. The advanced stage of the tumor at presentation, along with its location on the scalp, rapid progression, and the patient’s age, aligns with key risk factors for a poor prognosis. These factors underscore the challenges in managing cutaneous angiosarcoma and emphasize the critical importance of early detection to improve survival outcomes.
CONCLUSION
Cutaneous angiosarcoma of the scalp and face is a rare and aggressive malignancy that can present in a deceptive manner, often following injuries such as minor burns or lesions that are initially misdiagnosed or inadequately treated. This case underscores the importance of maintaining a high level of suspicion for angiosarcoma in lesions of the face and scalp, as early detection is crucial for improving survival outcomes. The challenges associated with managing angiosarcoma are further exacerbated by treatment delays, emphasizing the need for prompt intervention and effective communication with patients. A multidisciplinary approach, involving dermatopathology, surgery, and oncology, is essential to optimize treatment outcomes and address the complexities of this devastating malignancy.
Future research should focus on elucidating the precise mechanisms by which trauma, including scald burns, contributes to the development of cutaneous angiosarcoma. Understanding the molecular and inflammatory pathways involved may provide insights into early biomarkers for detection and potential therapeutic targets.
This case also highlights the importance of addressing financial and psychological barriers to treatment. A comprehensive, patient-centered approach that integrates oncologic care with financial assistance and psychosocial support is crucial to improving treatment adherence and overall outcomes. Future efforts should focus on developing accessible healthcare strategies, particularly in resource-limited settings, to ensure timely diagnosis and intervention for patients with this rare and challenging malignancy.
Patient Consent
Written informed consent was obtained from the patient for the publication of this case report, including clinical details and images. Efforts have been made to anonymize the data to maintain confidentiality.






