BACKGROUND AND AIMS
Scarring alopecias (SA) are uncommon, and despite their morbidity, research on pediatric patients remains limited.1,2 Data on the most effective treatment strategies and clinical outcomes in this population are also insufficient.
This study aimed to describe the demographic and clinical characteristics, comorbidities, treatment approaches, and outcomes of pediatric patients with SA managed at the authors’ institution over the past 5 years (January 2019–September 2024).
METHODS
A retrospective review was conducted on patients under 16 years of age diagnosed with alopecia at the Trichology Clinic of the Dermatology Department at Hospital Universitario Dr. José Eleuterio González, Monterrey, Mexico between January 2019–September 2024. Patients with diagnostic uncertainty were excluded.
Clinical notes, pathology reports, laboratory data, and photographs were manually reviewed. Comorbidities, medical treatments, and treatment responses were assessed for all patients.
RESULTS
The study included 226 patients under the age of 16 years diagnosed with alopecia, with a mean age at diagnosis of 8.9±3.8 years and no significant sex predominance. Among them, 24 patients (10.6%) had scarring alopecia (Table 1), which was more common in males (66.6%) and was associated with an older mean age at diagnosis (11.6±3.3 years).
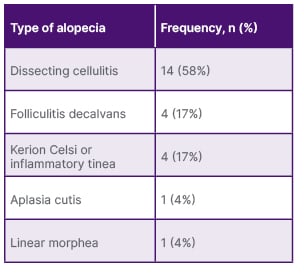
Table 1: Types of scarring alopecias in pediatric patients at the Trichology Clinic of the Dermatology Department, Hospital Universitario Dr. José Eleuterio González (2019–2024).
The average time for SA from onset to diagnosis was 10.7±12.1 months. Symptoms were reported by 45% of patients, with pruritus and pain being the most common (25%). A biopsy was necessary for diagnosis in 20% of cases, while the remaining patients were diagnosed clinically. Dissecting cellulitis was the most frequent form (58.3%) (Figure 1), followed by folliculitis decalvans (16.6%). Among the patients with available anthropometric data for these two conditions, 41.8% were overweight or obese (BMI >25). Other forms of SA (25%) included linear morphea, aplasia cutis, and cases secondary to Kerion Celsi or inflammatory tinea.
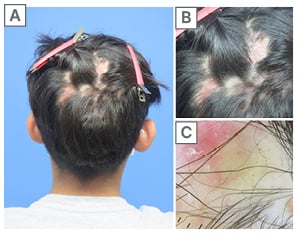
Figure 1: (A–B) Multiple alopecic plaques in the parieto-occipital region with erythematous, fluctuant nodules in an 11-year-old male; (C) Dermoscopy reveals black dots, yellow dots, and erythematous areas with polymorphic vessels.
Most used treatments included intralesional steroids, topical minoxidil, topical steroids, doxycycline, or azithromycin. Additionally, low-dose isotretinoin (0.3–0.5 mg/kg/day) was administered to 64% of patients with dissecting cellulitis, resulting in partial or complete improvement.
On average, patients in this study experienced hair loss for 10–11 months before receiving a diagnosis. In scarring alopecias, early treatment is crucial to reducing symptoms and slowing disease progression. Biopsy is a valuable tool for confirming the diagnosis, particularly in cases where clinical presentation is not definitive.
CONCLUSION
In the authors’ clinic, dissecting cellulitis of the scalp was the most common cause of scarring alopecia, diagnosed in 14 cases. To date, fewer than 20 pediatric cases have been reported in the literature, suggesting that this condition may be underdiagnosed in the pediatric population. Based on their experience, low-dose isotretinoin (0.3–0.5 mg/kg/day) has shown favorable outcomes, achieving partial or complete remission in most pediatric patients.
The limited data on pediatric scarring alopecia highlight the need for further research. Treatment remains a challenge, as many therapies used in adults are not approved for children. Establishing safe and effective therapeutic options is essential to halt disease progression in the pediatric population.






