BACKGROUND AND AIMS
Although vascular complications are considered the most serious adverse events associated with dermal filler injections, inflammatory complications, such as infections, granulomas, and hypersensitivity reactions, also present significant challenges and can lead to serious consequences if not promptly managed.1 A thorough understanding of the causes of these complications is essential for improving prevention strategies, diagnostic accuracy, and treatment protocols, all of which are crucial for optimising patient outcomes. This study aims to investigate the aetiology and presentation of inflammatory complications associated with dermal fillers. By providing an updated literature review and presenting a series of cases from the author’s clinical practice, the study offers practical insights into the real-world management of these adverse events.
MATERIALS AND METHODS
A comprehensive literature review was conducted using search terms such as “dermal filler complications”, “injectable filler adverse effects”, and “hyaluronic acid filler complications”. Databases such as PubMed and Google Scholar were utilised to gather peer-reviewed studies, focusing on complications related to various filler materials, including hyaluronic acid, calcium hydroxyapatite, and poly-L-lactic acid. In addition to the literature review, the authors analysed 12 clinical cases of inflammatory complications following dermal filler injections, either originating from or presenting to their practice over a 24-year period. Each case was documented with photographic evidence and detailed management strategies. Key variables, such as the type of filler, time to complication onset, diagnostic methods, and therapeutic approaches, were carefully examined to assess patterns in complication development and resolution.
RESULTS
The authors’ findings confirm that while dermal fillers are generally considered safe, inflammatory complications can arise from various factors. These were mainly infection and biofilm formation, which were implicated in several cases. Hypersensitivity reactions were possibly due to filler impurities or residues from manufacturing equipment and syringes, bolus or large volume injections, low-viscosity fillers, or the patient’s immune status.2,3 The main controversies in the literature are related to the aetiology, whether mainly infective or mainly hypersensitivity, and whether steroids should be used in the treatment if hypersensitivity is suspected. Key prevention strategies involve strict adherence to aseptic techniques, removing all makeup residues, and using high-quality fillers. Diagnosis was based on clinical signs and symptoms of inflammation, ultrasound and culture and sensitivity, and occasionally biopsy if purulence was present.
In the author’s series, tailored treatment approaches were successful though prolonged follow-up was needed for those with permanent fillers:
- Ten patients, where infection was suspected, received antibiotics. These were primarily a fluoroquinolone-macrolide combination, administered for 3–6 weeks.
- Systemic corticosteroids, such as prednisone (40 mg/day for 7–21 days) or intramuscular betamethasone, were used in six cases. Two of which had clear hypersensitivity reactions and four of whom did not respond to antibiotics.
- Intralesional therapies included hyaluronidase in five cases and triamcinolone acetonide in four cases. Although strongly suggested in the literature for permanent fillers, 5-fluorouracil was not used in the author’s cases.
- In three cases of permanent fillers, wide-bore needle extraction of collections was necessary (Figure 1), and surgical removal was attempted in two cases.
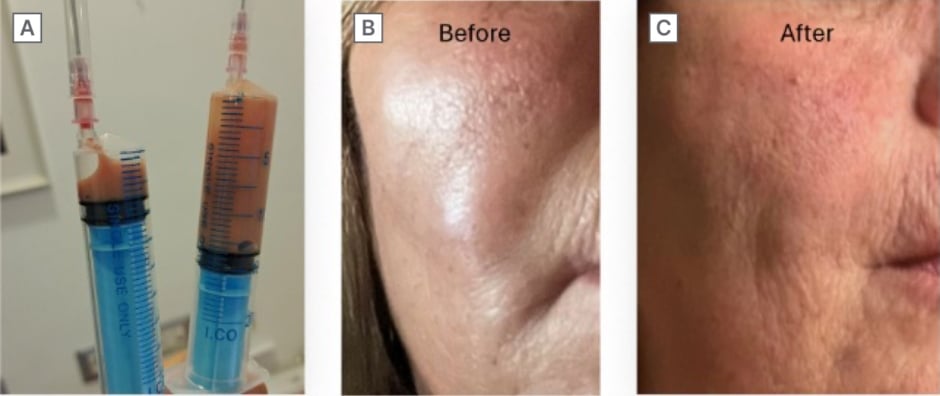
Figure 1: Sterile pus from a permanent filler injected 15 years ago.
A) Aspirated pus. B) Facial abscess pre-aspiration. C) One week post-aspiration.
CONCLUSION
This study highlights that inflammatory complications from dermal fillers, though rare, can arise from various factors, including inadequate hygiene, filler type, and manufacturing impurities. Strict adherence to aseptic techniques and the use of high-quality fillers are critical preventive measures. Establishing standardised guidelines and encouraging further research will improve long-term outcomes. In the author’s case series, tailored management strategies led to a successful resolution.






