INTRODUCTION
Cutaneous warts are benign epithelial lesions caused by human papillomavirus (HPV) and are common entities, affecting nearly 10% of the United States population.1 While most warts spontaneously resolve, the immunocompromised are susceptible to recalcitrant warts, which often require medical treatment.2 Most current therapies use either physical or chemical destruction for wart removal, but these treatments are associated with adverse effects.3 Intralesional vitamin D3 has the potential to demonstrate a stronger treatment response due to its ability to stimulate the immune system at the injection site via cell-mediated immunity.4
METHODS
The authors sought to test the efficacy of intralesional vitamin D3 for wart treatment in a sample size of 70 patients over a 3-month period. Efficacy was determined as “excellent” if there was greater than a 90% reduction in both size and number of lesions, “good” if there was a 60–89% reduction, and “fair” if there was less than a 60% reduction.
RESULTS
Treatment efficacy was excellent in 20 (28.6%) patients, good in 29 (41.4%) patients, fair in 18 (25.7%) patients, and poor in three (4.3%) patients (Figure 1A and 1B). Patients in the younger age group had a higher treatment efficacy compared to other treatment groups.
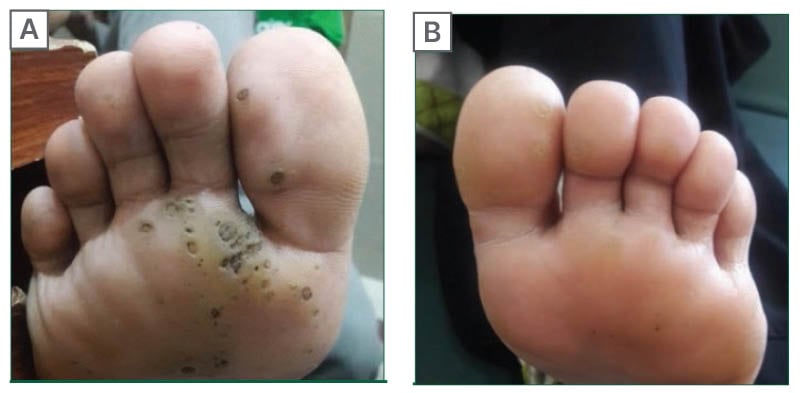
Figure 1: Cutaneous warts before (A) and after (B) treatment with intralesional vitamin D.
CONCLUSION
In conclusion, intralesional vitamin D3 has promising qualities as a treatment for cutaneous warts and should be considered at the clinician’s discretion. Vitamin D is an innovative approach for treating warts without the various side effects posed by other commonly used agents. The unique features of this treatment modality, including its simplicity, safety, and efficiency, make it a promising option for a very common cutaneous condition.






