Abstract
Chest pain and coronary artery disease (CAD) impose a substantial burden on public health and society. Diagnostic imaging tests are used by clinicians to identify the presence and extent of epicardial coronary disease and/or its consequences, including ischaemia, infarction, and left ventricular dysfunction.
In this article, we discuss current practice guideline recommendations for the diagnosis and management of patients with suspected or known CAD, and the need for more evidence from clinical trials. We then focus on the recently published and ongoing multicentre clinical trials of imaging-based strategies for the diagnosis and management of ischaemic heart disease, and the potential future impact of these trials on clinical practice. The results of these trials have the potential to bring radical changes to the practice of cardiology in the future.
INTRODUCTION
Coronary artery disease (CAD) is an important global public health burden, with a mortality rate of 1.2–2.4% per annum.1 The diagnosis of ischaemic heart disease (IHD) in patients with stable symptoms can be challenging because of variations in the pre-test probability of CAD, as well as the accuracy, cost, and availability of diagnostic tests and related management strategies.2,3 New diagnostic imaging-guided strategies have emerged for the detection and management of stable CAD, and gaps in clinical evidence for these diagnostic approaches contribute to important differences in global clinical practice.1,4 In this article, we briefly review contemporary practice and knowledge gaps around the diagnosis and management of patients with suspected or known CAD. We then focus on recently published and ongoing clinical trials in this area, and their potential impact on clinical practice in the future.
CLINICAL CONTEXT
Functional stress testing, mainly with electrocardiogram exercise treadmill testing (ETT) and stress myocardial perfusion scintigraphy (MPS), are established standard-of-care diagnostic tests for CAD. Technological developments now enable more advanced non-invasive imaging-guided strategies. These diagnostic approaches comprise functional assessments of ischaemia, including stress echocardiography, stress perfusion cardiac magnetic resonance (CMR), and stress positron emission tomography (PET) (Table 1).
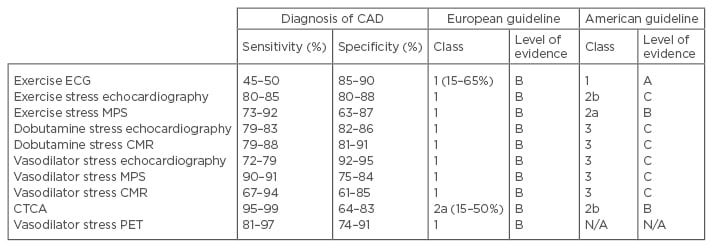
Table 1: Sensitivity and specificity of non-invasive diagnostic tests for coronary artery disease and international practice guideline recommendations.
The North American practice guideline recommendations account for the patient’s ability to exercise, the presence of an interpretable ECG, and an intermediate-high pre-test probability of CAD.4
CAD: coronary artery disease; ECG: electrocardiogram; MPS: myocardial perfusion scintigraphy; CMR: cardiac magnetic resonance; PET: positron emitting tomography; CTCA: computed tomography coronary angiography.
Adapted with permission from Montalescot et al.1
Alternatively, anatomical imaging of CAD with computed tomography coronary angiography (CTCA) is an emerging diagnostic option. CTCA may be combined with functional imaging, i.e. CTCA-perfusion and computed tomography-fractional flow reserve (CT-FFR). Concordant with good clinical practice, clinical judgement and informed patient preferences are important.4
Diagnostic Uncertainties and the Justification for Randomised Clinical Trials
The coronary artery disease hypothesis and anatomical imaging
The ‘CAD hypothesis’ states that detection of epicardial CAD through coronary artery imaging enables risk stratification for therapy, including non-pharmacological, medical, and invasive intervention, leading to future health benefits.1,4 The evidence for management strategies based on CAD imaging with invasive coronary angiography (ICA) is well established,1,4 whereas evidence is lacking for non-invasive imaging-guided strategies. This evidence gap supports the rationale for the ongoing and recently published randomised trials. Importantly, diagnostic accuracy based on visual interpretation of invasive angiographic images alone may not be appropriate due to the poor correlation between visually assessed angiographic anatomical stenosis severity and the physiological significance of a stenosis.5
The ischaemia hypothesis and functional testing
Myocardial ischaemia occurs when demand for perfusion exceeds supply.6 Ischaemia may result from obstructive epicardial CAD limiting coronary blood flow, coronary microvascular disease (CMD) reducing myocardial perfusion, or systemic problems (e.g. anaemia or tachyarrhythmia) resulting in a supply-demand mismatch.7 Myocardial ischaemia may result in typical angina pectoris, atypical symptoms (e.g. exertional dyspnoea), or may be clinically silent.8 Ischaemia revealed by functional imaging is associated with an adverse long-term prognosis.9 The ‘ischaemia hypothesis’ supposes that ischaemia is an adverse prognostic attribute, and that reducing the ischaemic burden by medical therapy with or without coronary revascularisation will result in improved clinical outcomes, as observedin the COURAGE trial MPS sub-study.10,11
Anatomical versus functional tests in suspected or known stable coronary artery disease
Practice guidelines now recommend anatomical approaches in lower-risk patients with CTCA and ICA in higher-risk patients, recognising that randomised trial evidence is limited (levels B/C).1,4 The ideal non-invasive diagnostic test would have high spatial resolution (for coronary lesions, perfusion, or ischaemic defects), allow quantitative assessment of ischaemia severity, avoid or minimise ionising radiation exposure (concordant with the principle of ‘As Low As Reasonably Achievable’), and provide additional diagnostic information such as assessment of myocardial function and scarring.
CONTEMPORARY PRACTICE GUIDELINES FOR STABLE CORONARY ARTERY DISEASE AND THE NEED FOR MORE CLINICAL EVIDENCE
European guidelines do not recommend non-invasive diagnostic tests in patients with a pre-test probability of CAD <15% or >85%.1 The UK National Institute of Clinical Excellence (NICE) guidelines recommend that diagnostic testing is not indicated in chest pain patients with a pre-test probability of CAD <10%.12 In very low-likelihood groups, medical management is recommended, whereas in the high-likelihood groups, ICA is suggested. ETT has been omitted and replaced with CT calcium scoring±CTCA for low-risk patients (given the high sensitivity and negative predictive value, but relatively lower specificity, of CTCA), and non-invasive stress imaging with echocardiography, MPS, or CMR in intermediate pre-test risk.
Estimates of obstructive CAD are based on historical data, which potentially overestimate risk, and European guidelines may increase the rate of unnecessary ICA.13,14 Since CAD is endemic in many developed countries, routine CTCA in adults with chest pain will commonly disclose CAD and result in ICA. The presence of CAD does not equate to causality, and non-cardiac causes of chest pain may coexist. This supports the case for ischaemia testing invasively (i.e. FFR) or non-invasively (i.e. CT-FFR or stress imaging).
Attributes and Limitations of Imaging Strategy Trials
There is uncertainty surrounding the comparative effectiveness of imaging-based diagnostic strategies for the detection and management of CAD. This lack of evidence underpins the rationale for several large clinical trials that have recently reported or are ongoing. The trials may be summarised as:
- Trials designed to assess the most effective imaging strategy for the diagnosis and management of suspected angina (anatomical versus functional imaging-guided strategies, and non-invasive versus invasive strategies)
- Trials designed to assess the health outcomes of invasive management versus medical management
TRIALS OF THE STRATEGIES
Detection of Coronary Artery Disease and Diagnosis of Angina in Patients with Chest Pain of Suspected Cardiac Origin
SCOT-HEART trial
The SCOT-HEART trial is a multicentre randomised controlled trial of 4,138 patients referred from primary care to a cardiology clinic for chest pain assessment. SCOT-HEART evaluated the role of routine CTCA in addition to standard care (typically with ETT) versus standard care alone in the investigation and risk assessment of patients with suspected angina.15 SCOT-HEART16 assessed whether anatomical delineation of the presence or absence of obstructive or non-obstructive CAD alters the diagnosis, management, and outcomes of patients with chest pain attending a rapid access chest pain clinic. Patients aged 18–75 years were randomised (1:1) to standard care, or standard care plus coronary artery calcium scoring and CTCA. Eligibility criteria were not restricted by the pre-test likelihood of CAD or a prior history of CAD, so patients with any pre-test risk may have been enrolled. Also, angina class was not an eligibility criterion, thus patients with crescendo or unstable angina may have been included. The primary outcome was the certainty of the diagnosis of angina secondary to CAD at 6 weeks.
The primary outcome was increased in the group randomised to CTCA (relative risk: 1.79, 95% confidence interval: 1.62–1.96). At 6 weeks, CTCA reclassified the diagnosis of CAD in 27% of patients, and the diagnosis of angina due to CAD in 23%. At 1.7-year follow-up, there was a trend towards a reduction in fatal and non-fatal myocardial infarction (MI) with CTCA, but this did not reach significance (p=0.0527, absolute difference between the groups: 16 events). Longer-term follow-up is planned for 5 years. Figure 1 presents a patient case study from this trial.
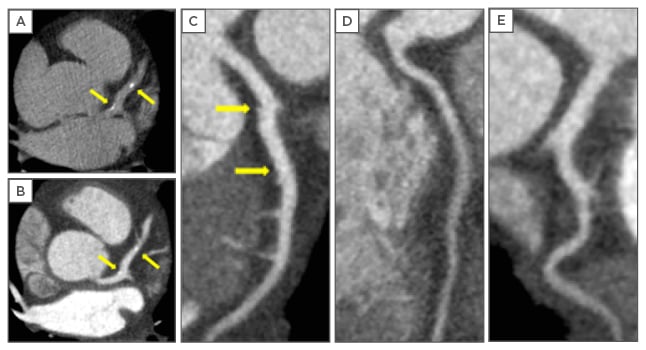
Figure 1: Computed tomography of a SCOT-HEART trial participant.
A 60-year-old male presented to the rapid access chest pain clinic with a history of typical angina. He had no risk factors for CAD. A treadmill exercise tolerance test was interpreted to be positive for myocardial ischaemia. As part of the SCOT-HEART trial, he underwent computed tomography imaging with a 320 multi-detector scanner using iterative reconstruction. A non-contrast scan was performed to assess coronary artery calcification. A) The Agatston coronary artery calcium score was 51 Agatston units. CTCA identified mild calcified and non-calcified atherosclerotic plaque in the left anterior descending artery (arrows). B) Shows axial images of the left anterior descending artery at the same position as the non-contrast images, and curved planar reformations are shown of: C) the left anterior descending artery, D) the right coronary artery, and E) the left circumflex artery. Despite these reassuring findings, the attending clinician still referred the patient for invasive coronary angiography because of ongoing symptoms. There was no angiographic evidence of CAD and the patient has had uncomplicated progress on medical therapy. This case provides an example in which the exercise ECG overestimated the likelihood of CAD and CTCA might have prevented the requirement for invasive investigations.
CTCA: computed tomography coronary angiography; ECG: electrocardiogram; CAD: coronary artery disease.
This case was kindly provided by Dr Michelle Williams, Clinical Research Fellow, and Prof David Newby, Principal Investigator for the SCOT-HEART trial.
By design, SCOT-HEART did not have concealment of the diagnostic intervention, and consequently the management and outcomes were susceptible to unmeasured confounding. The trial was not powered for health outcomes and the event rate was low (1.6% rate of death or MI at 1.7-year follow-up), indicating that the results are hypothesis-generating, and the 5-year outcomes are eagerly anticipated. Routine CTCA in this strategy is anticipated to be associated with increased costs, predominantly related to the cost of the scan. Information on quality of life and the health economic analysis are awaited.17
CEMARC 2 trial
The CEMARC 2 trial is a prospective multicentre, three-arm parallel group, randomised controlled trial of routine functional imaging versus guideline-based management.18,19 CEMARC 2 randomised 1,202 patients (2:2:1) to 3.0 Tesla stress perfusion CMR, MPS (according to American College of Cardiology [ACC]/American Heart Association [AHA] appropriate-use criteria), or to management based on the pre-test probability of CAD (CT calcium scoring±CTCA: 10–29%; MPS: 30–60%; ICA: 61–90%), concordant with UK NICE guidelines.12 Patients aged >30 years with known or suspected angina and a pre-test likelihood of CAD 10–90% were enrolled. The primary outcome is the occurrence of unnecessary invasive angiography, with secondary outcomes including a major cardiovascular event (MACE) at 1 and 3 years, and a cost-effectiveness analysis. Unnecessary ICA is defined as: i) negative FFR (>0.80) and a positive non-invasive test (i.e. false-positive test result); ii) negative FFR with a high pre-test probability (61–90%) proceeding directly to ICA in the NICE guidelines-based group (i.e. false-positive for the strategy); iii) negative FFR and a negative non-invasive test (i.e. true-negative strategy result where the imaging result was ‘not believed’ by the treating cardiologist [intention-to-treat principles]); iv) negative FFR and an inconclusive non-invasive test in which angiography was performed to make the diagnosis (i.e. failure of the strategy to produce a diagnosis).
The primary outcome occurred in 69 (28.8%) patients in the NICE guideline-managed group, and 36 (7.5%) and 34 (7.1%) in the CMR and MPS groups, respectively. There was a statistically significant lower adjusted odds ratio (OR) of unnecessary angiography in the CMR versus NICE guidelines group (OR: 0.21, p<0.001), with no difference between the CMR or MPS group (OR: 1.27, p=0.32). There was a trend towards a reduction in the secondary outcome of MACE at 12 months in the NICE guidelines group (1.7%), compared to the CMR (2.5%) and MPS (2.5%) groups, but this was not statistically significant. CEMARC 2 demonstrates a significant reduction in unnecessary angiography with a CMR-guided strategy. The NICE guideline-based strategy resulted in significantly more unnecessary invasive angiograms. Future guidelines may utilise improved risk stratification models.20
In contrast, a strategy of stress PET imaging has high diagnostic accuracy for CAD. The PACIFIC trial results were presented in August 2016 but are not yet published.21 PACIFIC enrolled 208 patients from a single centre referred for ICA following a first-presentation with chest pain secondary to suspected CAD. Participants had an intermediate pre-test likelihood of CAD and were aged >40 years. All patients underwent ICA with FFR measurement to define flow-limiting epicardial CAD. Patients then underwent stress PET, MPS, or CTCA alone, with some patients undergoing hybrid anatomical/functional imaging with PET/CTCA or MPS/CTCA. The diagnostic accuracy of PET (85%) was significantly greater than MPS (77%, p<0.01) and CTCA (74%, p<0.01), with no improvement in diagnostic accuracy with the hybrid imaging approaches. PACIFIC confirmed the high diagnostic accuracy of stress PET imaging, however there is generally limited access to this modality worldwide.
Management Strategies Involving Imaging of Coronary Anatomy Versus Functional Testing in Patients with Low-Intermediate Likelihood of Coronary Disease
PROMISE trial
PROMISE was an open-label multicentre imaging study comparing CTCA versus non-invasive functional stress testing (ETT, MPS, or stress echocardiography) in 10,003 patients with chest pain due to known or suspected angina.22,23 PROMISE tested the hypothesis that an initial anatomical testing strategy would inform subsequent patient management resulting in superior long-term health outcomes, as compared to an initial functional testing strategy. The functional test was selected at the clinician’s discretion, and may have reflected local availability. The primary outcome was time to the first MACE.
Compared with non-invasive functional testing, CTCA did not improve clinical outcomes at a median follow-up of 2 years compared with functional testing (3.3% versus 3.0%). The interpretation of PROMISE may be limited by the low event rate and relatively short follow-up period. Contemporary non-invasive functional tests such as stress perfusion CMR and PET, which have a higher sensitivity for detecting ischaemia, were not included. There was a significant difference in the revascularisation rates at 90 days between the CTCA and functional testing group (6.2% versus 3.2% of patients, p<0.001), however if functional results for ischaemia (e.g. invasive FFR) were lacking, the appropriateness of these revascularisations is uncertain. PROMISE concluded that either a routine functional or routine anatomical strategy is reasonable.17 In comparison, CT-FFR may allow a hybrid anatomical and functional imaging strategy and extend the role of CT-based strategies. CT-FFR is assessed using proprietary software which applies three-dimensional blood flow simulations using the principles of computational fluid dynamics.24,25
RESCUE trial
The RESCUE study26 is a multicentre randomised controlled trial of 4,300 patients, comparing two different diagnostic imaging modalities: CTCA versus MPS. In addition, building on the results of the COURAGE trial,11 all patients without evidence of left main stem disease will be treated with optimal medical therapy (OMT). The primary endpoint is a combination of MACE and revascularisation. It is hypothesised that CTCA is cheaper and patients will be exposed to less radiation with no increase in the rate of MACE or revascularisation, with a 24-month follow-up. On 27 October 2014 the study was terminated because the funding timeline had completed. By September 2014, 1,050 participants had been randomised. No further information is available at this time.
CARE-CTCA trial
The CARE-CTCA trial is a multicentre randomised trial of 1,050 patients investigating the cost-effectiveness and health outcomes of a CTCA versus MPS-guided management strategy in patients with an intermediate risk of CAD.27 Patients aged 30–80 years with an intermediate probability of CAD will be randomised (1:1) to either CTCA or MPS. The primary outcome is a cost-effectiveness analysis at 1 year.
Taken together, the results of these ongoing trials26-28 will provide information on whether or not a CTCA-guided approach improves symptoms, prognosis, and cost-effectiveness compared to functional approaches, in which MPS will likely be used in the majority of the participants.
Non-Invasive Imaging Versus Invasive Coronary Angiography in Patients with Intermediate-High Likelihood of Coronary Artery Disease
MR-INFORM trial
MR-INFORM is a multicentre randomised controlled non-inferiority trial designed to compare 1.5 Tesla stress CMR to routine ICA with FFR measurement, in order to guide revascularisation in patients with stable angina.29 MR-INFORM participants would be eligible for ICA based on clinical criteria concordant with clinical guidelines.1,12 The trial includes 918 patients who will undergo perfusion CMR prior to angiography, and will then be randomised (1:1) to either CMR-guided management or FFR-guided management (perfusion CMR result not disclosed) of intermediate angiographic lesions (≥40% to <99% severity). Inclusion criteria are age >18 years, typical angina, plus ≥2 cardiac risk factors, or positive ETT. Figure 2 presents a patient case study from this trial.
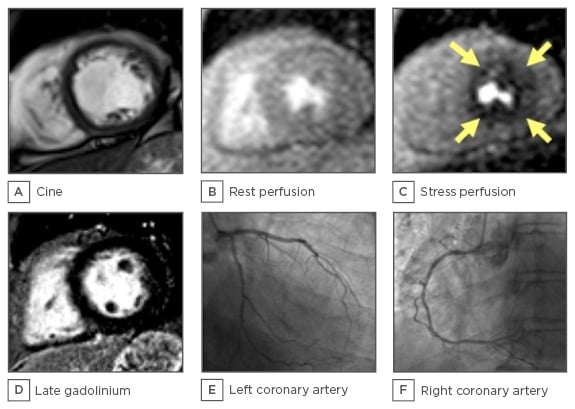
Figure 2: Magnetic resonance imaging of a MR-INFORM trial participant.
A 61-year-old female cigarette smoker with a history of symptoms consistent with angina was referred by her primary care physician for out-patient cardiology investigations. Based on this history, the pre-test probability of CAD was estimated to be 68% and a referral for invasive coronary angiography was made in line with contemporary guidelines. The woman fulfilled the eligibility criteria for MR-INFORM and, based on informed consent, she was randomised to the MR-guided group. CMR cine imaging revealed A) normal left ventricular systolic function, and compared with first-pass CMR imaging at rest; B) adenosine stress perfusion CMR; C) revealed a circumferential subendocardial inducible perfusion defect; D) the absence of late gadolinium enhancement imaging ruled out an infarct scar; E and F) invasive coronary angiography revealed minimal non-obstructive CAD. A diagnosis of microvascular angina was established and she was treated with 20 mg of isosorbide mononitrate twice daily, 75 mg of aspirin daily, and 40 mg of simvastatin daily.
CMR: cardiac magnet resonance; CAD: coronary artery disease.
Reproduced with permission from Dr David Carrick, Golden Jubilee National Hospital, Glasgow, and Prof Eike Nagel, principal investigator for the MR-INFORM trial.
MR-INFORM hypothesises that in patients with a high likelihood of CAD, management based on a functional test without knowledge of coronary anatomy could be an acceptable alternative approach to invasive management. MR-INFORM will provide further evidence on the safety and efficacy of perfusion CMR in the investigation of CAD. By design, CEMARC 2 involved a lower-risk patient population than MR-INFORM and so these trials should provide complementary information.
In contrast to these functional strategies, the DISCHARGE study tests the hypothesis that an anatomical CTCA-guided strategy is superior to ICA in patients with a low-to-intermediate pre-test likelihood of CAD.30 DISCHARGE will randomise (1:1) 3,546 patients with stable chest symptoms, aged >30 years, and with a pre-test likelihood of CAD of 10–60%, to CTCA or ICA. The enrolment period will be 2 years and the maximum follow-up is 4 years. DISCHARGE is a superiority trial and the primary outcome measure is major adverse cardiac and cerebrovascular events. Secondary outcomes include symptoms, quality of life, and cost-effectiveness. Contemporary practice guidelines do not recommend routine invasive angiography as a first-line test in patients with a pre-test CAD likelihood of 10–60%, yet this is the likelihood range for inclusion in this trial.
Non-Invasive Versus Invasive Management of Symptomatic Patients with Non-Invasive Evidence of Moderate-Severe Ischaemia
ISCHEMIA trial
The ISCHEMIA trial is a multicentre randomised controlled trial of 8,000 patients.31,32 It tests the hypothesis that an initial strategy of ICA followed by percutaneous coronary intervention (PCI) if feasible, in addition to OMT, will reduce the composite primary endpoint of cardiovascular death or non-fatal MI in patients with at least moderate ischaemia on stress imaging (echocardiography, MPS, or CMR), compared with an initial conservative strategy of OMT alone, with ICA reserved for failure of OMT.
International guidelines recommend that revascularisation is targeted towards relieving ischaemia rather than anatomical lesions in the epicardial coronary arteries.33,34 Anatomical assessments of CAD alone are inadequate to accurately identify functionally significant disease.35 The results of the FAME and FAME-2 trials indicate that patients with symptoms and ischaemia (FFR ≤0.8) derive prognostic benefits from PCI versus medical therapy alone,36,37 whereas those with functionally insignificant lesions (FFR >0.8) do not. FAME-2 supports the validity of the ischaemia hypothesis, however this trial was not designed or powered to provide information on the ‘hard’ spontaneous outcomes of death or MI. The ISCHEMIA trial will further inform the hypothesis that invasive management with clinically-indicated revascularisation may improve health outcomes in patients with stable CAD and a moderate-to-large ischaemic burden, compared to OMT. The ISCHEMIA trial has pivotal importance for the future management of CAD.
The ISCHEMIA-CKD32 sub-study investigates the same questions as the ISCHEMIA trial but in patients with advanced renal disease, a group of patients that is particularly challenging to diagnose and manage effectively and safely.
Anatomical Imaging and Coronary Microvascular Disease
PROMISE enrolled 10,003 patients, with 1,015 undergoing diagnostic ICA within 90 days of randomisation.23 A predefined secondary endpoint of non-obstructive CAD on ICA occurred in 3.4% of the CTCA group and 4.3% in the functional testing group (p=0.02). Does this cohort with anginal symptoms and non-obstructive CAD (some with positive non-invasive stress testing) represent patients with a non-cardiac aetiology for their symptoms, false-positive non-invasive stress testing, or might CMD contribute? Angina may occur in the absence of flow-limiting epicardial CAD. In this situation, patients may receive no further diagnostic testing and be reassured that they have a non-cardiac cause for their symptoms. However, a significant number may have coronary CMD and ‘microvascular angina’.38 In comparison to the literature concerned with epicardial CAD, there is a nascent evidence-base for the diagnosis and therapeutic interventions in coronary CMD.
There is no available technique which allows direct visualisation of the coronary microcirculation in vivo. Increasing use of invasive diagnostic tests to assess parameters of coronary physiology (coronary pressure, flow, and microvascular resistance) are providing new, clinically relevant diagnostic and prognostic information.39 Additionally, coronary endothelial dysfunction may result in angina which may be evaluated with vaso-reactivity testing.40 These observations have challenged the dogma that IHD equates to obstructive epicardial CAD.41 Non-invasive functional tests have lower sensitivity and specificity for CMD, although the kinetics and distribution of perfusion abnormalities revealed by stress perfusion CMR can be diagnostic. A limitation of the CAD hypothesis is that anatomical diagnostic tests, such as CTCA, are of limited value for the diagnosis of microvascular angina. There are several comparatively small multi-modality imaging studies in patients with microvascular angina, including iPOWER,42 however large randomised trials of therapeutic interventions are lacking. In summary, reflecting the heterogeneous causes of angina, we propose ‘stable coronary artery syndrome’ as a new unifying diagnostic term.
Summary of Imaging Studies
Clinical trials also have limitations; trials involve patient selection that commonly excludes real-world patients with multi-morbidity and advanced disease (e.g. patients with advanced renal disease in CMR trials). The timing of randomisation is also key; randomisation performed close to the time of consent and prior to diagnostic testing should lead to enrolment of a study population more representative of real-world patients compared to randomisation performed downstream. Other important design considerations include concealment of treatment allocation, as this may lead to a falsely enhanced magnitude of treatment effect43 and blinded and independent assessment of primary and secondary outcomes.
TRENDS IN CURRENT PRACTICE AND FUTURE DIRECTIONS
An analysis of 397,954 patients with chest pain and no history of CAD who underwent ICA found that only 37.6% had angiographic evidence of epicardial CAD, whilst 39.2% had no epicardial CAD.44 This calls into question the initial diagnostic basis for referral, and also the work-up for CMD if obstructive epicardial CAD is excluded. Adoption of non-invasive and invasive tests of flow-limiting coronary disease has increased since these results emerged. Key questions around the roles of anatomical and functional testing and non-invasive versus invasive management are being prospectively assessed in large clinical trial populations. The current clinical guideline recommendations that are not supported by randomised trial evidence (i.e. level C for CTCA recommendations)1,4 are currently subject to prospective assessment. Finally, a doctor’s clinical opinion should be individualised to the patient, who is entitled to have options wherever possible to enable an informed decision.
CONCLUSION
The current diagnostic trials in stable CAD involve >30,000 patients globally. The ongoing trials are expected to report within the next 5–7 years and, depending on their results, the trials have the potential to bring radical changes to the practice of cardiology. A recognition that stable IHD may not only be due to obstructive epicardial CAD, but also to coronary microvascular and vasomotor abnormalities, may prompt further research into non-invasive functional testing. Anatomical and functional non-invasive imaging in epicardial and microvascular CAD will ultimately need to be demonstrated to improve health outcomes to enter daily clinical practice.








