BACKGROUND AND AIMS
Allergic rhinitis (AR) and allergic rhinoconjunctivitis (ARC) are common chronic disorders in children.1 They have a strong impact on the quality of life of children.2 Many studies indicate that colonisation of the gut early in life plays a substantial role in directing immune-system development.3 Microbial exposure during the perinatal period is linked to the epigenetic regulation of genes involved in allergic inflammation, and it alters susceptibility to allergic diseases. Immune responses in the gut may modulate immune responses in distant target organs, including the nose.4 Unlike in other allergic diseases, the therapeutic effect of probiotics in AR has been primarily demonstrated, whereas their preventive effects have not been conclusively defined.5 The objective of this study was to evaluate the efficacy of the probiotic microorganism Lactobacillus reuteri-DSM 17938 (LR) in the prevention of the development of AR and ARC in Slovenian children aged 9 years old.
MATERIALS AND METHODS
This prospective, epidemiological study included 316 maturely born infants with a positive history of parental allergy. The children were born between January 2008 and June 2010, were without congenital anomalies, and had a birth weight of at least 3 kg. They were exclusively breastfed for at least 4–6 months. After the fourth month, the same dietary intake for the child and avoidance of probiotics usage was recommended to parents. According to the addition of LR into the child’s diet, children were divided into two groups: Group A, 201 children exclusively breastfed, and Group B, 115 children breastfed with addition of LR. From the age of 4 weeks, the mothers of Group B infants added LR to breastfeeding for 12 weeks. Daily, 100 million live LR were given directly into the child’s mouth (87.8%) or were applied on the mother’s nipple while breastfeeding (12.2%). Every child was followed up by the same paediatrician until they were 9 years old. The prevalence of doctor-diagnosed AR and ARC was observed. The diagnosis was based on clinical history, examination, and allergy testing (elevated specific IgE and positive skin prick tests) performed by a physician unaware of the child’s group allocation. Data about frequency and duration of AR and ARC exacerbations were recorded. Chi-squared test with Yates’ correction and paired t-test were used for statistical analysis. p-values less than 0.05 were considered significant.
RESULTS
At 9 years, the prevalence of AR and ARC in the study group was 19.6% (10.4% of children had AR, 9.2% had ARC). The difference in the prevalence of two diseases was nonsignificant (p>0.05). No significant sex-specific difference in AR (males: 11.0%; females: 9.8%) or ARC (males: 6.7%; females: 11.7%) prevalence was found (p>0.05). The prevalence of AR was significantly lower in Group B (13.9% [A] versus 4.3% [B]; p=0.01). No significance between group difference in ARC prevalence was confirmed (9.5% [A] versus 8.7% [B]; p>0.05) (Figure 1). Lower frequency (episodes/child: 6.3 [A] versus 4.6 [B]) and shorter mean duration (days/episode: 13.9 [A] versus 11.4 [B]) of AR exacerbation episodes in Group B were observed (p<0.01).
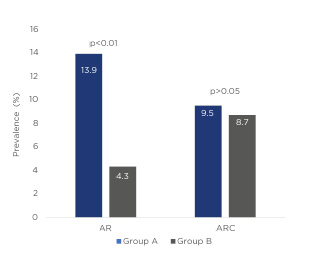
Figure 1: Prevalence of allergic rhinitis and allergic rhinoconjunctivitis in each group of infants.
AR: allergic rhinitis; ARC: allergic rhinoconjunctivitis.
The between group difference in frequency (5.9 [A] versus 6.0 [B]) and duration (15.8 [A] versus 16.5 [B]) of ARC exacerbations was insignificant (p>0.1).
CONCLUSIONS
The study confirms that early-life supplementation with LR is efficient in the primary AR prevention; additionally, it has beneficial impact on the course of AR. However, the study failed to demonstrate a positive effect on occurrence
and course of ARC.






