INTRODUCTION
Pain, increased bleeding, nerve damage, and, at worst, bladder rupture are a few of the potential consequences of undertreated post-partum urinary retention (PUR). Despite these possible sequelae, PUR is often underreported, with a wide-ranging incidence in the literature ranging from 0.18–17.9%.1,2 Although its incidence is not entirely clear, PUR remains a common indication for post-partum urogynaecology referral. One prospective, cross-sectional survey study of obstetric providers at a tertiary care health system found that 53.8% of survey respondents identified PUR as an indication for a post-partum urogynaecology referral.3 However, despite these findings, provider knowledge and standardised protocols for identifying and addressing PUR are often lacking. In one study, only 17.1% of obstetrician/gynaecologist (OB/GYN) resident respondents received formal didactics on the condition.1 In essence, PUR is under-recognised and under-reported, resulting in an unstandardised post-partum experience with noteworthy potential patient consequences. As such, it is important to consider the risk factors and clinical findings of this condition to appropriately develop management algorithms and direct potential future studies.
There are three types of PUR. Overt PUR is the complete inability to void at least 6 hours after a spontaneous vaginal delivery or after Foley removal from a caesarean section (CS). Covert PUR is incomplete bladder emptying, which is often defined as a post-void residual amount of at least 150 mL measured by bedside ultrasound or straight catheterisation. Lastly, persistent PUR is urinary retention that continues after 3 days post-partum and, sometimes, lasts several weeks. If left untreated, this type of long-term bladder retention can lead to parasympathetic nerve and detrusor muscle damage, which can transform into non-contractile fibrosis.2 Of these types, covert PUR is, not surprisingly, the most often underdiagnosed. Risk factors for these conditions vary widely and include prolonged labour, episiotomy, nulliparity, epidural analgesia, and perineal injury.4,5 The risk factor with the strongest association, however, is operative delivery.5,6 Studies have suggested that instrument use during delivery can lead to pelvic floor, bladder, and direct nerve injury with resulting dysfunction and oedema. This oedema can result in mechanical outlet obstruction and, subsequently, impaired reflex and relaxation of the urethral sphincter, periurethral muscles, and pelvic floor. Delayed voiding can lead to overdistention, which can further cause stretch injury, nerve ischemia and injury, and impaired detrusor sensitivity and contractility. It has also been suggested that discomfort from delivery and hesitancy with voiding in unfamiliar places may further contribute to emptying issues.
MANAGEMENT OF POSTPARTUM URINARY RETENTION
PUR management varies by institutional policy and PUR type. One algorithm, developed by Nutaitis et al.,1 recommends evaluating all patients for spontaneous voiding within 6 hours of delivery or catheter removal (Figure 1). For patients unable to void, overt PUR is identified using a bladder scan. For patients able to void, covert PUR can be evaluated based on urinary output, post-void residual volume, and/or symptomatology (e.g., suprapubic or lower abdominal discomfort). Depending upon the evaluation, patients are either observed or provided an indwelling urethral catheter. The timing of subsequent urethral catheter removal depends on the volume of retention and/or persistence of patient symptoms. Generally, catheter removal prior to discharge is appropriate for lower retention volumes, whereas arrangements for outpatient removal are made for larger retention volumes as delineated in Figure 1)..1 It is important when evaluating the post-void residual to interpret the volume obtained by catheterisation in the context of the preceding voided volume to understand the patient’s voiding efficiency. These data can help inform management decisions. Without algorithms such as these, appropriate identification of covert PUR is significantly more challenging, as patients who spontaneously void do not automatically undergo a bedside bladder scan unless there are other concerning symptoms. In these circumstances, diagnosis is greatly dependent on a strong provider–patient relationship and the communication therein. Moreover, timely diagnosis is highly impacted by the providers’ abilities to identify suggestive symptoms, including suprapubic fullness, displaced uterine fundal height, urinary frequency, feeling of incomplete bladder emptying, changes in urinary stream, and increased vaginal bleeding.
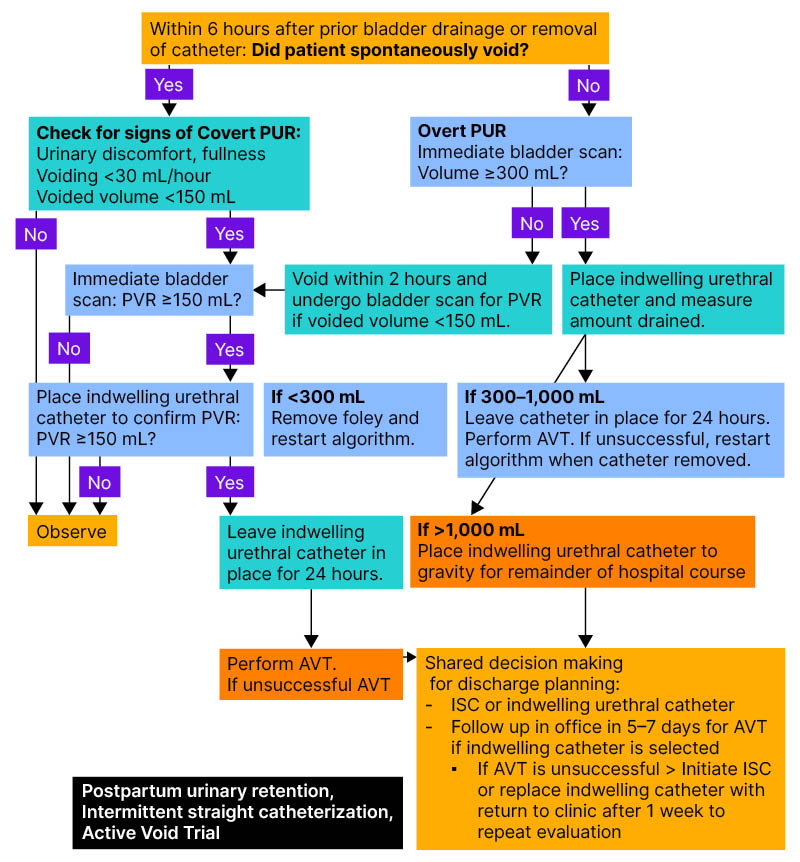
Figure 1: Postpartum urinary retention evaluation flowsheet.
This figure was previously published in Nutaitis AC et al. Postpartum urinary retention: an expert review. Am J Obstet Gynecol. 2023;228(1):14-21. Copyright Elsevier (January 2023).
AVT: active void trial; ISC: intermittent self-catheterisation; PUR: postpartum urinary retention.
Intermittent Self-Catheterisation
In addition to the algorithm by Nutaitis et al.,1 another potential intervention is to simply follow patient urinary output (UOP). If UOP is less than 30 mL/kg/hour, a bladder scan can be considered at that time to evaluate the PUR1. However, although following UOP is standardised care after a CS, it is less common after a vaginal delivery. For patients diagnosed with covert PUR, another management option is intermittent catheterisation. A randomised control trial by Bachar et al.7 evaluated the utility of intermittent versus continuous catheterisation for individuals with retained bladder volumes of at least 150 mL up to 6 hours after a vaginal delivery or Foley removal after CS. A total of 147 patients were enrolled, with 73 randomised to intermittent catheterisation and 74 to continuous drainage with an indwelling Foley. They found that the mean time to resolution was significantly shortened for the intermittent catheterisation group, with 99% of individuals in the intermittent catheterisation group experiencing PUR resolution by 24 hours, compared with 91% of patients undergoing continuous drainage. There were no significant differences between the groups for urinary tract infection or duration of hospitalisation.7 However, there were significant limitations to this study, including the impact of patient preference on intermittent versus indwelling catheter placement, variations in length of hospitalisation, and distorted anatomy. Still, this may suggest that intermittent catheterisation may have a role in the management of PUR.
Facilitating intermittent self-catheterisation is typically more labour-intensive, requiring additional time for patient education regarding the process of self-catheterisation, utilising clean techniques, and following up voided and residual volumes to direct patient care after discharge. It would also require the provision of additional resources, such as single-use lubricant, disposable catheters, and urine collection basins to measure residuals, bladder diaries, and other educational materials for those with PUR that does not resolve during their hospitalisation. These resources, in addition to patient preference and ability, may make self-catheterisation feasible for only a subset of patients.
PERSISTENT POST-PARTUM URINARY RETENTION
Persistent, or protracted, PUR is much less common, with an incidence as low as 0.05–0.18%.6,8. A study by Groutz et al.6 reviewed 37,757 women who delivered over a 3-year period. Among them, 55 individuals had persistent PUR beyond the third post-partum day. Of these patients, 65% achieved normal voiding within 2 weeks post-partum, while 35% achieved it within 28 days. Ultimately, only five developed long-term stress urinary incontinence, whereas four had overactive bladder symptoms. Findings were most suggestive of complete resolution of symptoms within 28 days without extraordinary long-term consequences. However, another study by Hickman et al.8 was significant for one patient with urinary retention up to 47 days after delivery. Generally, patients diagnosed further out from delivery were more likely to have protracted PUR. Management of protracted PUR may include pharmacologic therapy. Alpha-blockers, including prazosin or phentolamine, have been used in functional outlet obstruction.9 Cholinergic agonists, such as bethanechol, have been used for post-operative urinary retention. Both medications may be considered in the post-partum state; however, such use is complicated in the setting of breast-feeding patients due to the paucity of data on potential risks to the infant.9 Given the limited data on the efficacy of these agents, dosing considerations, maternal side effects, and neonatal considerations, non-pharmacologic management strategies should be prioritised, especially in breastfeeding mothers.
OTHER TREATMENT OPTIONS
Furthermore, an interesting potential area of study is the utility of acupuncture. A randomised control trial by Zhu et al.10 evaluated 1,200 patients across 12 hospitals in China over an 8-month period. Just more than 1,000 patients were enrolled in the study with approximately half undergoing routine care plus three sessions of a 4-hour acupoint hot compress involving the abdominal, lumbosacral, and plantar regions within 30 min, 24 hours, and 48 hours after vaginal delivery. They found that the intervention group had a significantly decreased incidence of PUR.10 The utility of acupuncture as a treatment for PUR in the USA is less clear but is likely to be low risk for patients who are interested.
CONCLUSION
The key components for facilitating early recognition and intervention for PUR include standardised post-partum care and patient education. It is imperative for institutions to develop a streamlined process for PUR identification and outpatient follow-up. Most importantly, post-partum patients should receive anticipatory guidance regarding expectations for spontaneous voiding and concerning signs/symptoms early in the post-partum period so that they may advocate for themselves. For those experiencing persistent or protracted PUR, it is important to have protocols in place for patient education regarding intermittent self-catheterisation and retrograde voiding trials in both inpatient and outpatient settings. Through anticipatory patient guidance, standardised protocols, and openness to potential interventions, PUR can be appropriately and expeditiously recognised and managed.







