Abstract
Peritoneal tuberculosis (TB) is a form of extrapulmonary TB that primarily affects areas such as the omentum, liver, intestines, spleen, and female reproductive organs. Diagnosing peritoneal TB can be challenging, as its presentation often resembles that of advanced ovarian conditions. Among the estimated 10 million TB cases worldwide, India has the highest number, with 2.8 million cases. In this case, a 14-year-old female presented with abdominal pain, distention, weight loss, and amenorrhoea. She had elevated CA-125 levels and left-sided pleural effusion observed on X-ray. An ultrasound showed significant ascites, and a contrast-enhanced CT scan of the abdomen and pelvis revealed widespread peritoneal thickening, marked ascites, and necrotic lymph nodes in the mesentery. A diagnosis of peritoneal TB was considered, and a biopsy of peritoneal deposits confirmed TB without malignancy. The patient was treated with anti-tubercular drugs, leading to substantial clinical improvement on follow-up. In cases presenting with massive ascites and high CA-125 levels without ovarian enlargement, clinicians should consider peritoneal TB as a potential diagnosis, alongside peritoneal carcinomatosis and advanced ovarian cancer, especially in resource-limited settings. Imaging is crucial in guiding diagnosis and narrowing differential options, while ultrasound-guided biopsy with histological analysis provides definitive confirmation.
Key Points
1. Peritoneal tuberculosis (TB) is a form of extrapulmonary TB that occurs in 1–2% of patients, with a higher incidence in developing countries.
2. This case report highlights the diagnostic importance, as well as the challenge, of distinguishing peritoneal TB from ovarian carcinoma to avoid misdiagnosis and ensure proper treatment. This distinction directly impacts the patient’s quality of life and long-term outcomes.
3. Peritoneal TB can cause remarkable elevation in serum CA-125 levels. Timely and accurate diagnosis is essential to ensure proper treatment, such as antitubercular therapy in peritoneal TB rather than surgical or oncological interventions
INTRODUCTION
Peritoneal tuberculosis (TB) is a significant public health issue in regions where the disease is endemic, ranking as the sixth most prevalent form of extrapulmonary TB, constituting ~3% of all extrapulmonary TB globally and 11–13% of cases in India.1 Abdominal TB typically impacts the omentum, intestines, liver, spleen, female reproductive organs, and the parietal and visceral layers of the peritoneum.2
Diagnosing peritoneal TB is challenging due to its vague symptoms, which can sometimes be mistaken for gynaecological cancers, such as advanced ovarian carcinoma.3,4 The disease frequently presents with nonspecific abdominal or pelvic symptoms, including masses, ascites, and elevated cancer antigen (CA) 125 levels, which are also associated with advanced ovarian cancer, and overlapping of these symptoms can lead to diagnostic confusion.5 In 2009, the WHO estimated there were 9.4 million TB cases globally, with the majority occurring in developing regions.6
Abdominal TB generally manifests in four forms: visceral TB affecting solid organs, lymph nodal TB, gastrointestinal TB, and peritoneal TB.7,8 Peritoneal TB is often characterised by ascites, mesenteric adhesions, lymphadenopathy, septations within ascitic fluid, and involvement of the omentum, all of which closely resemble the manifestations of primary peritoneal carcinoma or advanced ovarian carcinoma.9 Serum CA 125 levels can be raised in both peritoneal TB and ovarian cancer cases.7
Diagnostic imaging, including ultrasonography and CT, is crucial for evaluating such cases.10 For differential diagnosis, abdominal TB with ascites should be considered when ovarian cancer is suspected due to its potential to mimic widespread ovarian carcinoma.11
CASE REPORT
A 14-year-old female presented with abdominal pain and distension, low-grade fever, reduced appetite, weight loss, and irregular menstrual cycles over 2 months. She was previously in good health with no known history of chronic illness or TB. There was no family history of cancer. Due to her worsening symptoms, she sought evaluation at a tertiary care hospital.
Physical examination revealed abdominal dullness and a doughy abdomen without tenderness or a palpable mass. Abdominal assessment revealed a slighty distended abdomen with normal bowel sounds. On palpation, a positive impression of muscular defence was obtained. Tenderness in the umbilical region was found, but there was no chessboard phenomenon. The liver and spleen were within normal limits.
Laboratory tests showed the patient was anaemic, with a haemoglobin level of 9.0 g/dL, reduced albumin levels at 2.8 g/dL, and thrombocytosis with a platelet count of 499,000/L. Her CA 125 level was elevated to 136.4 U/mL (normal range: <35 U/mL).
Imaging studies included an initial chest radiograph, which showed clear lung fields and left pleural effusion (Figure 1A). Abdominal and pelvic ultrasonography detected gross ascites, mild right hydronephrosis, left pleural effusion, omental thickening, necrotic mesenteric lymph nodes, and mild free fluid in the pouch of Douglas. The uterus, ovaries, and endometrium appeared normal on ultrasound (Figure 1B).
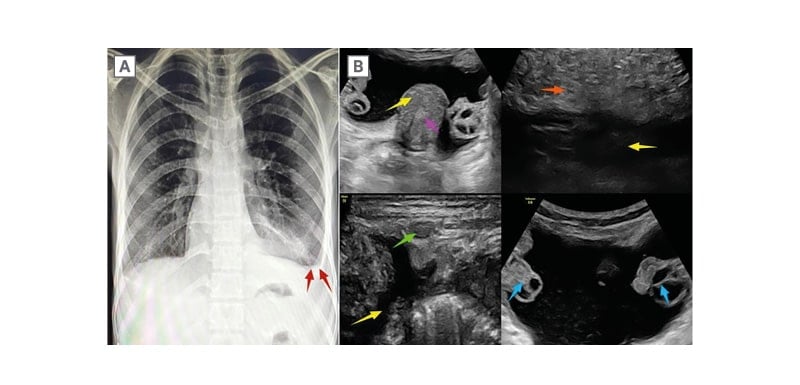
Figure 1: Chest radiograph and ultrasound of abdomen and pelvis.
A) Chest radiograph showed minimal left pleural effusion (red arrows). B) Ultrasound of abdomen and pelvis showed gross ascites (yellow arrows), omental thickening (orange arrow), necrotic mesenteric lymph node (green arrow), and fluid in the pouch of Douglas. Uterus (yellow arrow), ovaries (blue arrow), and endometrium (violet arrow) appear normal.
A contrast-enhanced CT scan of the abdomen and pelvis showed gross ascites, diffuse peritoneal thickening, clumping of bowel loops, mild right hydronephrosis, left pleural effusion, necrotic mesenteric lymphadenopathy, and mild free fluid in the pouch of Douglas. Both ovaries and uterus appeared normal. Peritoneal thickening was observed in the bilateral iliac fossa and hypogastrium (Figure 2).
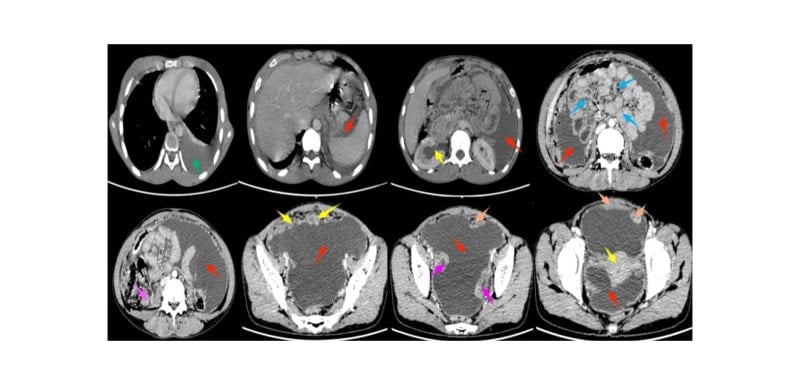
Figure 2: Contrast-enhanced CT of the abdomen and pelvis.
Contrast-enhanced CT of the abdomen and pelvis showed gross ascites (red arrows), diffuse peritoneal thickening in bilateral iliac fossa (yellow arrows) and hypogastrium (orange arrows), clumping of bowel loops (blue arrows), mild right hydronephrosis (yellow arrow), moderate left pleural effusion (green arrow), necrotic mesenteric lymphadenopathy (violet arrow), and fluid in the pouch of Douglas (red arrow). Both ovaries (violet arrows) and uterus (yellow arrows) appeared normal.
Differential diagnoses included peritoneal TB, peritoneal carcinomatosis, and advanced ovarian cancer. Pertaining to imaging findings and elevated CA 125 levels, peritoneal TB was considered likely. An ultrasound-guided biopsy was performed from the peritoneal thickening (Figure 3A). Histopathological analysis showed a granulomatous reaction typical of TB, including epithelioid granulomas with caseating necrosis, giant cells, and chronic inflammatory infiltrates, with no evidence of malignancy (Figure 3B). Mycobacterium TB was isolated on Acid-Fast Bacilli smear. Thus, a diagnosis of peritoneal TB was confirmed.
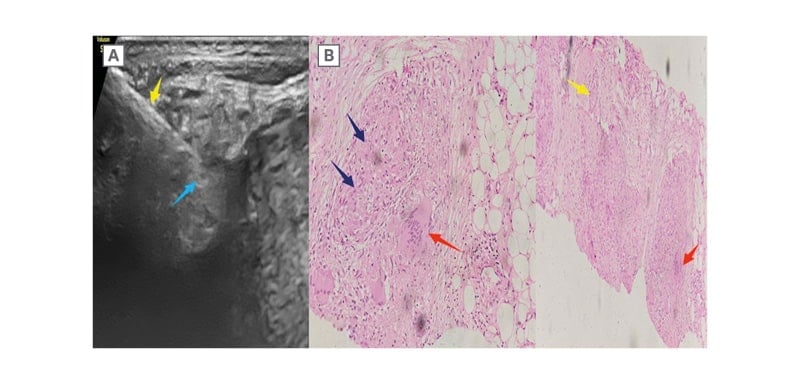
Figure 3: Ultrasound-guided biopsy and histopathological analysis.
A) An ultrasound-guided biopsy (yellow arrow) was performed on the peritoneal thickening (blue arrow). B) Histopathological analysis showed a granulomatous reaction typical of tuberculosis (dark blue arrows), epitheloid granulomas with caseating necrosis (yellow arrow), giant cells (red arrows), and chronic inflammatory infiltrates, with no evidence of malignancy.
The patient was enrolled in the Directly Observed Treatment Short-course (DOTS) programme and began receiving anti-tubercular medications. A follow-up ultrasound after 1 month showed reduced ascites, resolution of the previous right hydronephrosis, and clearance of the left pleural effusion. The patient exhibited marked clinical improvement and completed 6 months of anti-TB treatment.
DISCUSSION
Abdominal involvement is the most common extrapulmonary manifestation of TB, accounting for about 5% of all TB cases worldwide.4 The gastrointestinal tract, peritoneum (e.g., ascites), lymph nodes, and solid organs (e.g., the liver, spleen, and pancreas) are common sites of involvement in abdominal TB.12 The diagnosis of abdominal TB is challenging, as it typically presents with nonspecific symptoms, making it difficult and time-consuming to identify. However, with the advancement of imaging techniques like CT scans, it is now possible to detect lesions caused by chronic inflammation and distinguish them from malignancies.13
One rare manifestation of abdominal TB is tuberculous peritonitis, which occurs in less than 4% of patients with TB.14 Despite its rarity, it remains a significant cause of ascites in endemic regions. High-risk groups for developing TB include individuals with alcoholism, cirrhosis, renal failure, diabetes, malignancy, and immunodeficiencies such as AIDS.3,15 Symptoms of tuberculous peritonitis, such as abdominal distension, ascites, pelvic or adnexal masses, and elevated CA 125 levels are often similar to those seen in advanced ovarian carcinoma, and both conditions can present with fever and weight loss.12 In regions with high TB incidence, tuberculous peritonitis is an important cause of ascites.15 While tuberculous peritonitis and ovarian cancer are distinct conditions, they can be difficult to differentiate without proper diagnostic evaluation. Tuberculous peritonitis generally has a favourable prognosis with appropriate treatment, except in older or otherwise frail patients. Therefore, clinicians must be vigilant in considering TB as a possible diagnosis.16
Differentiating peritoneal TB from malignant abdominal tumours can be challenging, as they share the same symptoms.12,17 The spread of Mycobacterium TB from a pulmonary infection to the abdominal cavity through haematogenous dissemination is thought to contribute to peritoneal TB. The primary pulmonary focus typically heals without leaving clinical or radiological signs.8,10 Diffuse peritoneal diseases such as carcinomatosis, peritoneal lymphomatosis, malignant peritoneal mesothelioma, diffuse peritoneal leiomyomatosis, peritoneal TB, or IgG4-related disease present with similar imaging features, including nodular or diffuse peritoneal thickening, omental caking, and mesenteric invasion.1,18,19 Accurate early diagnosis is critical because the prognosis and treatment approach vary significantly between these conditions.20
Peritoneal carcinomatosis, for example, requires aggressive locoregional therapy, while tuberculous peritonitis may be managed effectively with anti-TB drugs.21 On imaging, peritoneal TB can resemble advanced ovarian cancer or other non-tuberculous granulomatous diseases.19,22 Tuberculous peritonitis can occur due to reactivation of latent TB foci in the peritoneum, haematogenous spread from a pulmonary infection, or ingestion of bacilli that spread via the intestinal mucosa and mesenteric lymph nodes.23 Another mechanism involves the contiguous spread of TB from the intestines or fallopian tubes.23 Peritoneal TB is categorised into three types based on the characteristics of the ascitic fluid: wet (free or loculated ascites), fixed fibrotic (omental and mesenteric masses with matted bowel loops), and dry plastic (thickened peritoneum and necrotic lymph nodes).22,24,25 Given the overlap in symptoms, a high index of suspicion is necessary to avoid unnecessary surgeries and ensure timely treatment.26
CA 125, a non-specific marker for peritoneal inflammation and a coelomic epithelial glycoprotein,28,30 is often elevated in conditions like ovarian carcinoma, endometriosis, and pelvic inflammatory disease, and it can also be elevated in peritoneal TB.29,30,32 Though CA 125 is used to monitor ovarian cancer treatment, its elevated levels are not definitive for malignancy.34 In some cases, CA 125 levels above 1,000 U/mL have been associated with malignancy, but there have also been instances of high CA 125 levels in peritoneal TB, making it unreliable as a sole diagnostic marker.31,32,33
A contrast-enhanced abdominal CT scan findings of peritoneal TB may include diffuse thickening of the peritoneum, nodules, and a ‘cake-like’ appearance of the omentum.36 Ascites are present in 70–90% of cases,27 and the mesenteric root fat planes may show densification with necrotic lymphadenopathy.35,36 Imaging techniques such as ultrasound, CT, and MRI can reinforce diagnosis. Ultrasound-guided tru-cut biopsy5 is a precious and minimally invasive method to obtain tissue for microbiological and histopathological analysis. A final diagnosis is typically made with microbiological and histopathological examination of biopsy samples, which reveal granulomas composed of epithelioid cells, lymphocytes, Langhans giant cells, and central caseous necrosis.37 Other than that, GeneXpert (Cepheid, Sunnyvale, California, USA) sputum and stool examinations, positive smear or culture from peritoneal fluid, histological appearance of granuloma, acid resistant bacillus test, and adenosine deaminase levels of ascitic fluid. and it has high sensitivity and specificity in non-TB endemic areas.35-37 Treatment for extra-pulmonary TB, including abdominal TB, typically involves a 6-month course of anti-TB drugs such as isoniazid, rifampicin, pyrazinamide, and ethambutol.38
Correct diagnosis is crucial, as treatment for peritoneal TB differs from that for ovarian cancer. While peritoneal TB can be treated with anti-TB medications, ovarian cancer requires surgical intervention and, in some cases, chemotherapy.39 Accurate diagnosis can thus help avoid unnecessary surgeries and enable appropriate treatment, particularly in high-incidence TB regions such as India.5
Informed Consent
Written informed consent was obtained from the patient.
CONCLUSION
Peritoneal TB is a significant diagnostic challenge due to its ability to closely mimic other conditions, particularly ovarian malignancy. This case report highlights the masquerades of peritoneal TB, with elevated serum CA 125 levels further complicating the diagnosis. Clinicians must be vigilant and consider TB as a differential diagnosis, especially in endemic areas and among immigrant populations, as it can closely resemble ovarian carcinoma. With appropriate treatment, peritoneal TB generally has a favourable prognosis. Early and accurate diagnosis can help avoid unnecessary surgeries, as pre-operative minimally invasive methods like ultrasound-guided biopsy can be utilised. Timely treatment and follow-up care are crucial for improving patient outcomes. Greater awareness and the use of radiological investigations are key to enabling early detection and effective management of this condition.
SIGNIFICANCE
Peritoneal TB is one of the most challenging forms of extrapulmonary TB to diagnose and requires more awareness because the clinical symptoms are nonspecific. Biological tests such as adenosine deaminase may be useful but are not always available in developing countries. Ultrasound and contrast-enhanced CT have the advantage of being cheaper, widely available, and easy to perform. In addition, it has high diagnostic cost-effectiveness and may be used in certain situations to guide peritoneal biopsy. No single test can effectively diagnose peritoneal TB, but a combination of history and radiological, immunologic, molecular, and cytologic tests are important. Clinicians need to consider peritoneal TB as a differential diagnosis in patients presenting with abdominal pain and distension, particularly in high TB-incidence countries such as India. A delay in the diagnosis and treatment of peritoneal TB may lead to worse clinical outcomes.







