Abstract
Scalp sarcoidosis is generally uncommon and it may present itself with varying morphologies; therefore, it is important to differentiate this disease from other forms of cicatricial and non-cicatricial causes of alopecia. Trichoscopy and histopathology are essential to rule out other skin diseases and to confirm diagnosis. Treatment options include topical, oral, and intralesional corticosteroids; immunosuppressive agents; and hydroxychloroquine, in order to arrest the progression of alopecia. Here, the authors present a case of scalp sarcoidosis with systemic involvement, in which dermoscopy gives important clues for its diagnosis. The authors have also reviewed the literature and identified 46 cases of sarcoidosis that induced alopecia.
Introduction
Sarcoidosis is a multisystem disease, of unknown aetiology, which can involve any organ of the body, even if it more frequently affects the lymph nodes, lungs, skin, and eyes. Scalp sarcoidosis is a rare localisation of cutaneous sarcoidosis and is usually associated with other skin lesions of the body, which can result in very different morphological presentations.1,2 The clinical and dermoscopic findings of alopecia due to sarcoidosis have recently been detailed.3 Here, the authors report a case of progressive scarring alopecia due to scalp sarcoidosis associated with stable lung involvement, where dermoscopy suggested the diagnosis of the scalp disease.
Case report
A 50-year-old Caucasian female was referred to the authors’ Department of Dermatology with 2-years’ history of alopecic patches of the scalp, which had always been small and stable but had gradually increased in size over the previous few months. The patient was affected by pulmonary sarcoidosis for around 20 years but at the time of presentation to the clinic was asymptomatic and had been followed-up without treatment for 10 years. The patient reported a negative QuantiFERON-TB test and a normal spirometry.
At the time of examination, the clinical manifestation of the scalp showed the presence of several irregularly round and confluent patches of alopecia localised at the vertex that were red-orange in colour. Examination of the whole skin and mucosal surfaces of the patient revealed the presence of a small atrophic red-brown plaque on her back, measured to be 1 cm by 2 cm (Figure 1). Trichoscopy of the alopecic patches showed loss of follicular ostia, a reddish-orange discoloration of the skin, and capillary telangiectasias. Other dermoscopic findings included white cicatricial skin spots, brown dilated follicular ostia with emerging hairs at the periphery of the patches, and a few dystrophic hairs. Dermoscopy of the skin plaque on the back showed a red-orange hue and dilated vessels (Figure 2).
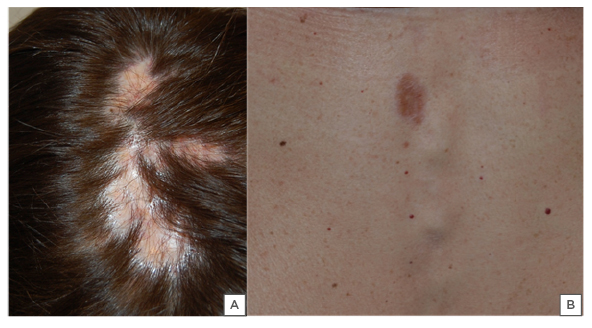
Figure 1: Clinical examination of the patient.
Clinical examination of our patient revealed (A) irregularly round and confluent patches of alopecia localised at the vertex that were red-orange in colour and (B) the presence of a small atrophic red-brown plaque of the back.
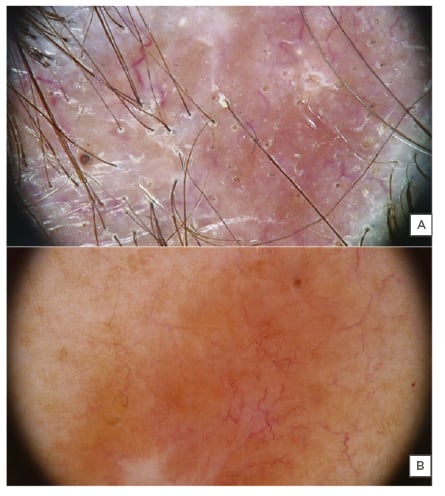
Figure 2: Trichoscopy of the scalp alopecia and dermoscopy of the skin plaque.
(A)Trichoscopy of the scalp alopecia showed loss of follicular ostia, a reddish-orange discoloration of the skin, and capillary telangiectasias (20x magnification); (B) dermoscopy of the skin plaque on the back showed a red-orange hue and dilated vessels (20x magnification).
A 4 mm punch biopsy was performed from the margin of an alopecic area of the scalp and showed non-caseating granulomas in the dermis composed of epithelioid histiocytes and a few multinucleated giant cells with surrounding infiltrate of lymphocytes. No follicular structures were evident (Figure 3). No fungal organisms or mycobacterial species were observed after periodic acid–Schiff (PAS) and Ziehl–Neelsen stain.
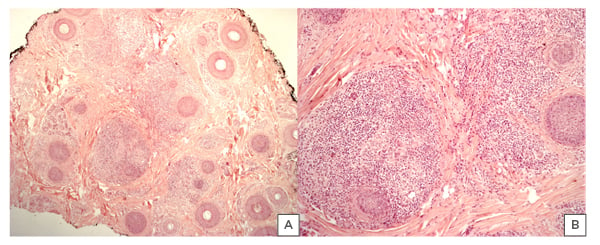
Figure 3: Pathology showed sarcoidal granulomas in the dermis, composed by epithelioid cells, with a few multinucleated giant cells, and a dense infiltrate of lymphocytes (A,B).
Taking these dermoscopical and histological results into account, the authors’ clinical suspicion of scalp sarcoidosis associated with lung sarcoidosis was confirmed. While waiting for her pneumologist to make a check-up and decide the best treatment, the patient was treated with local therapy based on clobetasol propionate ointment twice a day for 2 months. At the 2 month follow-up, the scalp lesions appeared to have not improved, while the back lesion was evidently reduced in size and thickness. Afterwards, because her pneumologist did not observe any change in sarcoidosis lung involvement and to stop progression of scalp alopecia, the authors prescribed a therapy of systemic triamcinolone acetonide at the dosage of 40 mg intramuscularly, one injection per month for 3 months and then a half injection per month for 2 months.
Systemic steroids were used to obtain a quicker halting of the progression of the disease. During the 2 years of follow-up, the disease remained stable in the scalp, without trichoscopic sign of activity, and remained unchanged during this time.
Discussion
Sarcoidosis is an idiopathic chronic disease characterised by the presence of non-caseating granulomas that can involve different organs but is usually localised in the lungs, lymph nodes, and the skin.4 Involvement of other sites, such as the liver, heart, nervous system, and kidneys, can also occur.5 The skin is affected in about 20–30% of sarcoidosis patients, with papular sarcoidosis usually evolving on the face, especially around the eyelids and nasolabial folds, or maculopapular eruptions on the neck, trunk, extremities, and mucous membranes. Many cutaneous manifestations of sarcoidosis appear mostly at the onset, often as presenting symptoms. Histopathologically, classic sarcoid granulomas are non-necrotising with a central area composed of macrophages, epithelioid cells, multinucleated giant cells, and lymphocytes. The central areas are surrounded by CD8 and CD4 positive T lymphocytes surrounded by fibrosis. The proportions of lymphocytic infiltrate and fibrosis surrounding the granulomas vary depending on the patient and disease duration. Systemic therapy is chosen depending on severity of the systemic involvement, such as lung or other organs, since skin signs are usually treated with topical steroids.
The scalp is rarely affected by the sarcoidosis and only 46 cases of scalp sarcoidosis have been reported in the literature, with high prevalence in African-American women with associated systemic involvement.6 In most of these cases, cicatricial alopecia was described, though a few cases of non-scarring alopecia as well as diffuse form of hair loss were also reported.7,8
Sarcoidal alopecia of the scalp may present as an atrophic and scaling patch that is red in colour, or as a scarring alopecia mimicking other causes of scarring alopecia, above all discoid lupus erythematosus (DLE) or lichen planopilaris. The difficulty in differentiating sarcoidal alopecia from DLE is well documented: in agreement with Henderson et al.,9 the authors always recommend performing a skin biopsy to confirm a suspicion of DLE of the scalp.
It is important to keep in mind the possibility of necrobiosis lipoidica as another entity for the differential diagnosis; nonetheless, it rarely affects the scalp. This chronic granulomatous dermatitis can present itself with non-scaling plaque, characterised with erythematous violaceous borders and linear arborising vessels in a yellow background colour.10 Diagnosis of sarcoidal alopecia is generally achieved through histopathological examination, which typically shows sarcoidal granulomas in the dermis. The local destruction and scarring of the follicles in scalp sarcoidosis may cause a permanent alopecia, which can be indistinguishable from pseudopelade of Brocq.11
Torres et al.3 have recently proposed trichoscopy as a useful tool in the diagnosis of scalp sarcoidosis. They described the presence of ‘orange spots’, corresponding to the granulomas in the superficial dermis, and of prominent telangiectasia in the scalp, due to the vasodilatation in the papillary dermis. Dystrophic hairs may be present, in correlation with the granulomas activity that induces a scarring alopecia. Nonetheless, the sarcoidal hairless patches are generally described as red, well circumscribed, and pruritic. Cheraghi et al.12 reported that they become hypopigmented and asymptomatic in time, further complicating the clinical diagnosis. The authors detected these features both in the scalp and in the back skin of the patient. Thus, the orange hue with telangiectasia should be considered a specific sign of skin sarcoidosis, as already stated by Pellicano et al. in 2010.13 The particular anatomy of the scalp makes dermoscopic signs richer than in non-hairy skin, because hair shafts and follicular units have to also be considered. In scalp sarcoidosis, together with the dermoscopic signs seen on the skin, presence of, especially at the margin of the alopecic area, dilated ostia bigger than the well-known yellow dots typical of alopecia areata and dystrophic hairs that are not specific and are possibly seen in both scarring and nonscarring alopecia can be detected. These features are very important because they represent signs of an active state of the disease and so they can give information about the disease progression and prognosis. The loss of follicular ostia is, on the other hand, a sign of scarring, meaning a permanent loss of hair.
According to Katta et al.,1 scalp sarcoidosis is usually resistant to treatment. Therapeutic options include antimalarial therapy; topical, systemic, and intralesional corticosteroids; and other immunosuppressive drugs, such as azathioprine, but with a poor response. High potency topical steroids in ointment vehicle were ineffective in the authors’ patient’s scalp sarcoidosis after 2 months and systemic steroids were fundamental in stopping the progression of alopecia.
CONCLUSION
Trichoscopy is highly helpful for diagnosis of hair and scalp disorders and should always be used to properly evaluate any lesion on the scalp in patients with alopecia. This is especially true in cases of suspected scarring alopecia, where a prompt diagnosis is very important to start therapy and stop the progression of the disease. Trichoscopy gives important diagnostic clues in scalp sarcoidosis, i.e., a reddish-orange discoloration of the skin associated with wide telangiectasia, but the histological examination remains indispensable to confirm the diagnosis. Finally, clinicians should always remember that a scalp involvement in sarcoidosis should require a systemic treatment, even if the disease at the level of another internal organ is stable.







