Abstract
Background: Idiopathic uncal herniation in patients is a very rare phenomenon, with only two cases documented in the English literature.
Case Report: The authors report a previously fit and well patient in their 60’s who presented with a 12-month history of headaches and vomiting. On clinical examination, there was no focal neurology, and all cranial nerves were intact. MRI revealed an incidental finding of left uncal herniation, which was likely developmental. The patient was discharged from neurosurgery, with a plan for the GP to refer to neurology for the headaches and vomiting.
Discussion: A correct diagnosis of idiopathic brain herniation is important to avoid unnecessary invasive procedures. Herniation should be differentiated from other pathologies, including tumours, encephaloceles, and dural venous sinus thrombosis.
Conclusion: Incidental findings of uncal herniation remain an extreme rarity. Future research is required to guide management and prognostication in this select group of patients.
Key Points
1. Idiopathic uncal herniation remains an extremely rare and poorly researched phenomenon with unclear pathophysiology.2. Proper identification of idiopathic brain herniation is important to mitigate the need for unnecessary invasive procedures.
3. Incidental findings of uncal herniation should be managed conservatively.
INTRODUCTION
The uncus is a hook-shaped structure located on the most anteromedial aspect of the parahippocampal gyrus, which is part of the medial temporal lobe.1 Functionally, it is a part of the limbic and olfactory systems, and thus plays a putative role in olfaction, emotion, and memory.2
Uncal herniation is a sub-type of transtentorial herniation, characterised by medial and downward displacement of the uncus against the tentorial edge, compressing the midbrain and oculomotor nerve (cranial nerve III).3 This is an acquired, emergent condition that is usually caused by an underlying brain lesion or an expanding mass effect (e.g., traumatic brain injury, subdural haemorrhage, extradural haemorrhage, or intracerebral haemorrhage). Very rarely, uncal herniation may occur with minimal or unrelated symptoms without any discernible aetiology.4
To the best of the authors’ knowledge, there are only two reported cases of idiopathic uncal herniation in the current English literature.4,5 Given the extreme rarity and clinical significance, the authors present a case of an incidental finding of idiopathic uncal herniation diagnosed on MRI, with a brief review of the existing literature.
CASE REPORT
A patient in their 60’s presented to the Neurosurgical Outpatient Clinic of the Royal Stoke University Hospital (RSUH), Stoke-on-Trent, Staffordshire, UK, with a 12-month history of pressure in the neck radiating to the front of the head, with associated vomiting. They also reported pressure and pain in their right ear, and had been diagnosed with sensorineural hearing loss and tinnitus by their GP. They were prescribed a hearing aid, which improved their hearing but not their headaches.
In their background history, the patient was right-hand dominant and had recently retired and lived alone. They had never smoked but consumed alcohol on a social basis. Past medical history included obstructive sleep apnoea (for which they used a continuous positive airway pressure machine), hypothyroidism, hypertension, osteoarthritis, depression, gastro-oesophageal reflux disease, and insomnia. Their medications included: simvastatin, extended-release oxycodone, sertraline, omeprazole, levothyroxine, lisinopril, hyoscine, amitriptyline, bisoprolol, and a buprenorphine transdermal patch. They did not have any known drug allergies.
On examination, their Glasgow Coma Scale (GCS) score was 15/15, and their cranial nerves were intact. They exhibited normal tone and power in all four limbs and walked with a normal gait. Their BMI was elevated at 33.1.
An MRI head (Figure 1) demonstrated a left medial temporal lobe herniation across the medial tentorium that was indenting the left cerebral peduncle. Scattered white matter small vessel ischaemic changes were also noted, with no enhancing abnormality or tumour identified. The rest of the imaging appeared unremarkable. Following discussion at the neuroradiology multidisciplinary team meeting, the consensus was that the MRI appearance was in keeping with an incidental left uncal herniation. It was felt that this was likely to be a developmental anomaly, which could not account for their tinnitus and hearing loss. Subsequently, the patient was discharged from neurosurgery, with a recommendation for their GP to refer them to the neurology team for their headaches.
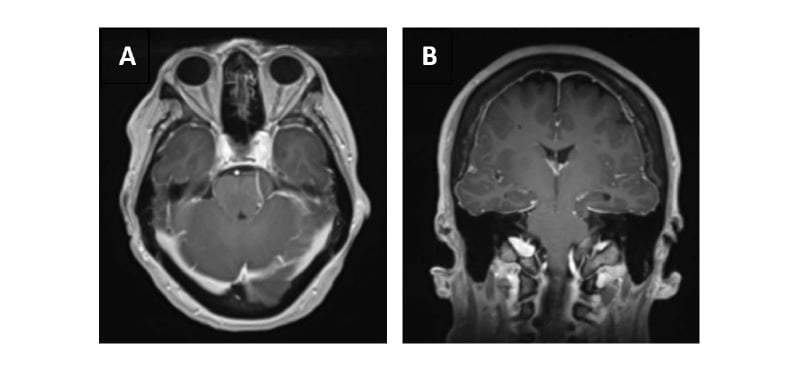
Figure 1: Gadolinium-enhanced T1-weighted MRI head showing a left medial temporal lobe herniation across the medial tentorium that is indenting the left cerebral peduncle.
A) Gadolinium-enhanced T1-weighted axial and B) coronal MRI head. White matter scattered small vessel ischaemic changes are noted as well, with no enhancing abnormality or tumour identified. Department of Radiology, Royal Stoke University Hospital, Stoke-on-Trent, Staffordshire, UK.
DISCUSSION
First, the authors considered whether the patient’s MRI findings were in keeping with their clinical presentation. Given the chronicity and lack of progression of their symptoms (intermittent, stable, episodic headaches associated with vomiting for almost one year); lack of focal neurological deficits on examination, in particular, no evidence of left-sided cranial third nerve palsy; and lack of other acute intracranial findings on imaging (e.g., mass effect or congenital malformation) that could contribute to herniation, it would be reasonable to label the left uncal herniation observed on imaging as idiopathic in nature, and therefore, likely a developmental anomaly.
Indeed, idiopathic brain herniation is an extremely rare finding, with a prospective study on idiopathic cuneus gyrus herniation showing a prevalence of just 0.73%.6 To date, the authors are aware of only 18 reported cases of idiopathic brain herniation in the English literature, of which, only two have been reported as idiopathic uncal herniation.
Yavarian et al.4 reported the case of a 46-year-old male who presented with a sudden onset right-sided facial nerve palsy, whose MRI revealed an uncal/parahippocampal gyrus herniation. Similarly, Ram and Sherry5 reported a case of a 40-year-old female with a long-standing history of chronic headaches which were associated with nausea, photophobia, diplopia, and dizziness since the age of 2 years. The patient’s MRI showed bilateral uncal herniation, greater on the right than the left, in the absence of any other intracranial abnormality.5 In both of these cases, there were no known specific triggers or history of head trauma, and detailed neurological examination did not reveal any focal neurological deficits.
The pathophysiology of idiopathic uncal herniation remains unclear. Some studies propose that localised dural and dural extension defects arising during meningeal embryogenesis may be responsible for focal brain parenchymal herniation.7 Others suggest that a wide tentorial incisura and angle of the tentorium cerebelli in relation to the tentorial incisura are risk factors for developing idiopathic uncal herniation.5 Meanwhile, the occurrence of chronic uncal herniation in the paediatric age group has been attributed to a negative pressure gradient created in the posterior fossa secondary to shunt placement or malfunction, as seen in children with Dandy-Walker syndrome or other large, cystic cavities in communication with the fourth ventricle.8
In recent years, research has supported the direct correlation between elevated BMI, percentage body fat, and raised intracranial pressure (ICP). Indeed, previous studies hypothesised that central obesity leads to raised intra-abdominal pressure, leading to poor venous return from the brain, and subsequently increased ICP.9 This may explain the incidental uncal herniation seen in the authors’ patient.9 Another possible cause could be use of the continuous positive airway pressure machine, which decreases systemic venous return by increasing intrathoracic pressure, leading to raised ICP.10 However, in both instances, the authors have not reliably explained why the raised ICP would only be unilateral rather than bilateral. Additionally, the authors do not routinely see uncal herniation in patients presenting with idiopathic intracranial hypertension.
In an acute emergent setting, uncal herniation requires prompt monitoring and reduction of the raised ICP, which may involve temporising medical measures or more definitive surgical decompression techniques.11 However, given its rarity, there is no consensus regarding how to manage incidental findings of brain herniation. For symptomatic uncal herniation, we need to address the underlying cause, such as idiopathic intracranial hypertension, shunt malfunction, or space-occupying lesion. If the uncal herniation is asymptomatic, adoption of a conservative approach should be considered.
In terms of complications, the authors wonder if chronic brain herniation is a poor prognostic marker. Naidich et al.12 concluded the same in a case series they reported, in which two of the seven paediatric patients diagnosed with chronic transincisural herniation died from further (unspecified) complications at the ages of 3 months and 4.5 years. Certainly, any significant uncal herniation may compress the surrounding vital brain structures. For example, compression of the oculomotor (cranial nerve III) nerve results in an ipsilateral oculomotor nerve palsy, which manifests as a ‘fixed dilated’ pupil and a ‘down and out’ pupil due to paralysis of the superior, inferior, and medial rectus muscles, and the inferior oblique muscle. Compression of the ipsilateral midbrain cerebral peduncle causes contralateral hemiparesis, while compression of the contralateral cerebral peduncle, due to extensive midline shift, causes a false-localising ipsilateral hemiparesis, also known as the Kernohan-Woltman notch phenomenon.13 Compression of the posterior cerebral artery leads to occipital infarction, resulting in homonymous hemianopia, if unilateral, or cortical blindness, if bilateral. Finally, if left untreated, uncal herniation progresses to central herniation, resulting in secondary brainstem haemorrhages (Duret haemorrhages), as well as abnormal respiratory patterns leading to respiratory arrest due to disruption of the ascending respiratory activating system.11
LEARNING OUTCOMES
Firstly, clinicians should recognise idiopathic and chronic uncal herniation to avoid misdiagnosis. Proper identification of idiopathic brain herniation is also important to mitigate the need for unnecessary invasive procedures, such as biopsies and surgeries. For example, the misinterpretation of a parahippocampal herniation as a medial temporal lobe lesion in a 41-year-old man who presented with right-sided trigeminal neuralgia resulted in unnecessary invasive surgical exploration, including a biopsy which revealed the findings of a normal brain.14
Secondly, idiopathic uncal herniation should remain a diagnosis of exclusion. Therefore, thorough history taking, clinical examination, biochemistry, and basic imaging should be performed to establish a specific cause first. In particular, it is important that clinicians are able to distinguish between herniations and mass lesions. MRI findings of a focal region of soft tissue signal intensity which is isointense compared to the adjacent brain parenchyma, and a lack of signal abnormality or contrast enhancement are useful characteristics in differentiating brain herniations from other pathologic masses.15
In conclusion, idiopathic uncal herniation remains an extremely rare and poorly researched phenomenon. Physicians are frequently compelled to intervene for these patients. Therefore, a thorough history and clinical examination are key to determining if the presenting symptoms are due to the radiological finding. For patients in whom the uncal herniation is an incidental finding, the authors would recommend a conservative approach to avoid unnecessary complications.







