BACKGROUND AND AIMS
Endoscopic mucosal resection (EMR) has increasingly gained acceptance as a minimally invasive intervention for the treatment of duodenal lesions.1 Despite the overall good results, there can be significant morbidity associated with performing EMR in the duodenum. Data comparing hot- and cold-snare approaches in the duodenum are currently scarce.2,3,4 The authors’ aim was to assess the efficacy and safety of hot-snare EMR (H-EMR) versus cold-snare EMR (C-EMR) for the resection of non-ampullary duodenal lesions.
METHODS
A prospectively collected database of duodenal lesions treated using EMR at a single tertiary medical centre between 2010–2023 was performed. Patient demographics, lesion and procedure characteristics, outcomes, and adverse events were analysed using R statistical software. The lesion size and procedural time were analysed using the Mann-Whitney U test, while clinical outcomes were analysed using the Fisher’s exact test. Cost savings were calculated from the averted use of clips.
RESULTS
Seventy-one cases of non-ampullary duodenal lesions resected using the EMR technique were included (46 H-EMR; 25 C-EMR). Fifty-one lesions were resected en-bloc (31 H-EMR versus 20 C-EMR), while 20 lesions were resected in a piecemeal fashion (15 H-EMR versus 5 C-EMR). Similar demographics, lesion, and procedure characteristics were observed in both cohorts (Table 1). Technical success was 100%, and no delayed perforations occurred in either cohort. Lesions resected via H-EMR had higher rates of immediate perforation (2.2% versus 0%; p=1.0) and delayed bleeding (9.1% versus 0%; p=0.28) compared to C-EMR. Interestingly, recurrence rates were higher in the H-EMR arm (15.2% versus 8%; p=0.70). C-EMR technique achieved a crude cost saving from clips alone of 135 USD per patient compared to the H-EMR technique.
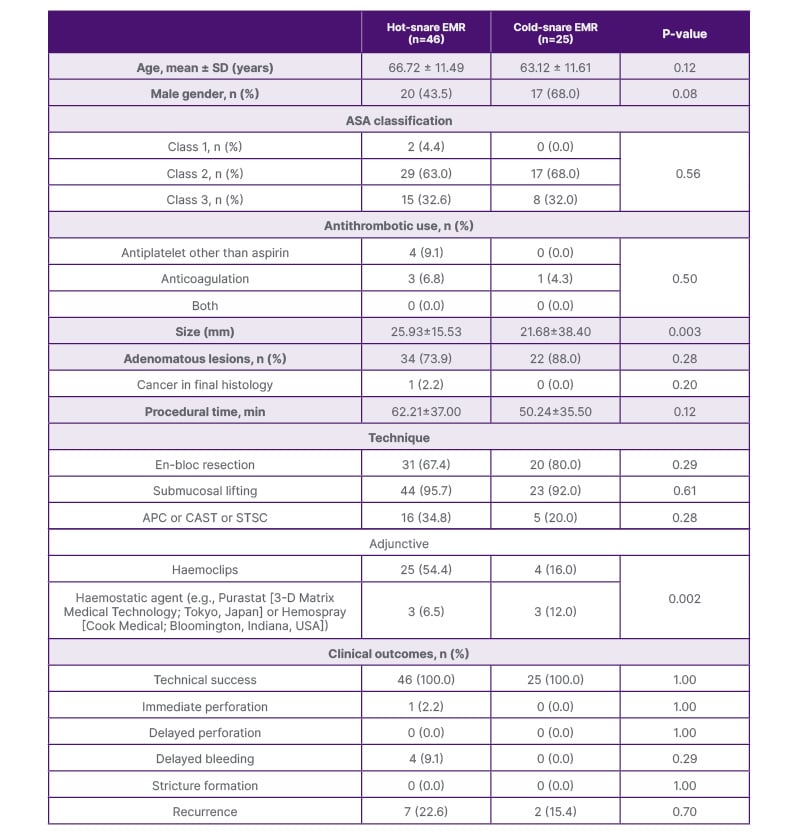
Table 1: Patient, lesion and procedure characteristics, and clinical outcomes.
APC: argon plasma coagulation; ASA: American Society of Anesthesiologists; CAST: Cold-forceps avulsion with adjuvant snare-tip soft coagulation; EMR: endoscopic mucosal resection; STSC: snare-tip soft coagulation.
CONCLUSION
While both cohorts demonstrated excellent technical success, there was a trend towards lower adverse events and recurrence rates, as well as cost savings, when C-EMR technique was used for non-ampullary duodenal lesions. The authors’ data consolidates previous findings and suggests an acceptable role of the cold resection approach in the duodenum. However, larger prospective comparative trials are warranted to bolster the present evidence and shape the state of the art.







