Abstract
Objective: To understand obstructive sleep apnoea (OSA) epidemiology and associated comorbidities in a Chest Unit in Hong Kong, and to better understand sleep referrals to enhance screening assignment.
Design: A prospective, observational case-series study from a Chest Unit in Hong Kong.
Subjects: Patients, aged ≥17 years old or older and referred to Wong Tai Sin Hospital for polysomnography, were recruited from the 15th of September 2022–31st of January 2023.
Methods: Demographic, anthropometric, and phenotypic characteristics were collected. Questionnaires (Epworth Sleepiness Scale [ESS], Patient Health Questionnaire-9 [PHQ-9]) were completed and polysomnography was performed on the following night. The presence of OSA was defined as apnoea–hypopnoea index (AHI) ≥5 events·h -1.
Results: A total of 303 patients were recruited. The prevalence of OSA amongst the referred patients was 91%, and ischaemic heart disease, diabetes, and hypertension accounted for 16.3%, 34.8%, and 63.4%, respectively. In addition, 43.4% of patients fulfilled the definition of depression according to their PHQ-9 score (≥5).
Conclusion: This observational study showed that the appropriateness of referrals for sleep tests was adequate, with 91% of patients having OSA. The majority of them are overweight or obese and presented with hypertension, diabetes, and mild depression, and excessive daytime sleepiness.
Key Points
1. This article showed that referrals for sleep study based on clinician’s knowledge were appropriate, with an accuracy of 91%.2. This case-series study tried to characterise the male and female phenotypes with obstructive sleep apnoea.
3. Primary care physicians should be aware of male and female clinical phenotypes for early diagnosis and intervention in order to lessen the burden on health outcomes.
INTRODUCTION
Obstructive sleep apnoea (OSA) is a complex and chronic disease characterised by loud snoring, daytime sleepiness, and witnessed breathing pause. It is defined by the American Academy of Sleep Medicine (AASM) as a decrease or complete cessation of airflow despite an ongoing effort to breathe,1 and it affects 4.1% and 2.4% of males and females in Hong Kong, respectively.2,3
Clinically, it is associated with the degradation of the quality of life, an increased risk of road traffic accident,4 and a detrimental effect on cardiovascular health. The pathophysiology consists of a repetitive collapse of the pharyngeal airway during sleep, leading to a transient interruption of airflow with hypoxia. It is accompanied by a central nervous system stimulation to restore upper airway patency and reoxygenation. Therefore, patients experience unrefreshing sleep with excessive daytime sleepiness due to fragmented sleep and hypoventilation.
Polysomnography (PSG) is the ‘gold standard’ to detect OSA;5 however, it is a limited and expensive test. The waiting time from referral to PSG is long. In particular, in the author’s locality, the waiting time from first consultation to PSG was 189.6 days in a teaching hospital, and in public settings the waiting time would be much more longer.6
Moreover, the referral for sleep test may not always be appropriate; the probability of making a referral for sleep apnoea can be influenced more by patient requests, regardless of physicians’ knowledge and attitudes toward OSA.7 Therefore, the use of screening questionnaire could clearly improve the prioritisation for referrals to sleep test. The STOP-BANG score, has a sensitivity from 81–86% to predict OSA in Hong Kong.8
At the Department of Tuberculosis and Chest, Wong Tai Sin Hospital, Epworth Sleepiness Scale (ESS), with an adequate reliability and validity, was mainly used to screen OSA.9 In addition, clinical presentation of OSA and depression may overlap. Signs and symptoms of fatigue, poor concentration, loss of interest, and insomnia can often be overlooked by clinicians as sleep apnoea symptoms. Among people with physician diagnosed OSA, the odds ratio for probable major depression was 2.4 among males and 5.2 among females.10 In their study, Garbarino S et al.11 showed that a pooled prevalence for depressive disorders was 35% in patients with OSA. In the author’s locality, Patient Health Questionnaire-9 (PHQ-9) is a valid tool to screen depression and has shown a sensitivity of 80% and specificity of 92%.12
OSA can also be associated with other comorbid conditions. A previous study showed that, in an OSA cohort, 34% of the patients had hypertension,13 32% suffered of diabetes,14 and 6.6% of ischaemic heart disease.14
The aim of this study was to assess the prevalence of OSA in patients referred for sleep test in a chest department and its related medical conditions. Furthermore, to aim to draw the phenotype of patients referred for sleep study.
MATERIALS AND METHODS
This prospective, observational case-series study was conducted at the Department of Tuberculosis and Chest, Wong Tai Sin Hospital from 15th of September 2022– 31st of January 2023. Ethical approval has been obtained from the Kowloon Central Cluster (KC/KE-18-0208/FR-3). Sources of the patient’s referrals were mainly from the Department of Medicine at Kwong Wah Hospital, Queen Elizabeth Hospital, Department of Otorhinolaryngology at Yan Chai Hospital, and the Department of Tuberculosis and Chest at Wong Tai Sin Hospital, Hong Kong.
For a 95% CI with 5% margin of error and with a disease prevalence of 4.1%, the sample size of the population of Hong Kong should be at least 61 patients. Most of the patients were referred for sleep test following symptoms of snoring and tiredness, while hypertension or obesity were not the main factors for referrals. All patients referred to the author’s Chest Unit who were aged ≥17 years and who did not have a known history of sleep disorders were consecutively recruited. Patients who were pregnant, in unstable conditions, on sleeping pills, or unable to fill out the questionnaires were excluded.
Patients who consented were invited to complete the two questionnaires (ESS, PHQ-9) on the day of admission prior to the sleep study. Patients with an ESS >10 were considered to have clinical daytime sleepiness.15 STOP-BANG is a score used to screen OSA. The total score ranges from 0–8, and patients can be classified for OSA risk based on their respective scores. The sensitivity of STOP-Bang score ≥3 to detect moderat-to-severe OSA is 93% and 100%, respectively.16
Anthropometric characteristics (BMI, neck circumference, and gender) were recorded. While demographic characteristics (hypertension, diabetes, and ischaemic heart disease) were retrieved from the clinical management system from hospital authority or directly from patients’ clinical notes. Level II-nocturnal PSG was performed using a Philips Respironics Alice 6 system (Philips Respironics, Murrysville, Pennsylvania, USA) in the sleep laboratory at Wong Tai Sin Hospital, Department of Tuberculosis and Chest. Recording comprised electroencephalogram channels, electrooculogram, and chin muscle electromyogram. An experienced sleep physician reviewed all the PSGs according to the AASM guidelines on sleep scoring.1 The severity of OSA was defined by the apnoea–hypopnoea index (AHI). Obstructive apnoea was characterised as complete cessation of airflow for at least 10 seconds. Hypopnoeas were characterised by a period of reduction of >30 % oronasal airflow for at least 10 seconds and associated with a ≥3% decrease of oxygen saturation and/or micro-arousal. The AHI is summarised as the sum of the total events per hour of sleep. OSA was defined using AHI as mild (5–15 events·h-1), moderate (15–30 events·h-1), and severe (>30 events·h-1).1 Patients were considered to have diabetes, hypertension, or ischaemic heart disease if they were on treatment prior to admission.
The Asian phenotype has a higher body and visceral fat associated with a lower BMI, and Asian patients develop OSA at a lower BMI than those who are Caucasian.17 Modifying the STOP-BANG cut-off BMI criteria to 30 kg·m−2 has improved the sensitivity without compromising specificity in OSA screening.17 The authors use the ‘modified’ STOP-BANG score, where the BMI of ≥30 kg·m−2 counts for one point.
On the day of admission, patients were asked to complete the ESS and the PHQ-9 questionnaires. The PHQ-9 is a nine‐item depression questionnaire. It is a self-report screening tool that identifies the presence and severity of depression. The severity of a depressive disorder can be divided into 5–9 (mild), 10–14 (moderate), 15–19 (moderately severe), and 20–27 (severe).18 Statistical analysis was performed using SPSS version 23 for Windows (SPSS Inc., Chicago, Illinois, USA) computer software.
Demographic data is presented with descriptive statistics. Continuous data that is normally distributed is presented as mean+/-SD and student T-test is used. A p-value <0.05 was set as statistically significant.
RESULTS
From the 15th September 2022– 31st of January 2023, 303 consecutive Chinese patients were enrolled and completed the questionnaires. Of these, 267 had OSA as defined by an AHI ≥5 events/hour. The prevalence of sleep apnoea amongst patients referred was 91%, whereas only 27 patients did not experience sleep apnoea. The mean age of referred patients with obstructive sleep apnoea was 55.81±12.51 years, 204 were male (73.9%) and 72 were female (26.1%). Of the patients, 71% had never smoked, 13.8% were active smokers, and 15.2% were ex-smokers. Ninety-six patients (34.8%) were diabetic, 45 patients (16.3%) had ischaemic heart disease, and 175 patients (63.4%) were hypertensive. The mean systolic blood pressure was 140.97±15.53 mmHg and the mean diastolic blood pressure was 87.23±11.78 mmHg. The mean BMI was 29.96±6.43 kg·m−2. The mean ESS was 10.73±5.04, while 43.5 % did not experience daytime sleepiness (ESS <10). At presentation, 41.7 % had mild-to-moderate excessive daytime sleepiness and 14.9 % had severe daytime sleepiness. The mean AHI was 40.429+/-24.23 event. hour-1, and the mean ‘modified’ STOP-BANG score was 4.86±1.52. ESS was 10.73±5.04 and the mean PHQ-9 was 5.13±4.5 and 43.4% of the sample had depression (defined as PHQ-9 ≥5).
Demographics/ Phenotypes by Gender
The overall male-to-female ratio for OSA was 2.8:1 (204 versus 72). Female patients were significantly older than male patients (58.40±10.96 years verses 54.89±12.91 years, respectively; p<0.05) and heavier (BMI 31.40±9.40 kg/m2 verses 29.45±4.91 kg/m2, respectively; p=0.02). Neck circumference in female patients, as expected, was smaller than that of males (38.01±3.78 versus 41.70±2.87, respectively; p<0.0001). Male patients tended to smoke more than female counterparts (17.6% versus 2.8%, respectively; p<0.05).
The presence of diabetes was similar between both genders, while males experienced a higher rate of hypertension and ischaemic heart disease ([/hl]Table 1[/hl]). As shown in Table 1, both groups presented with similar symptoms of snoring perception (80.9% for males versus 75% for females; p=0.28). Females perceived more tiredness than males (69.4% versus 55.9%; p<0.05).
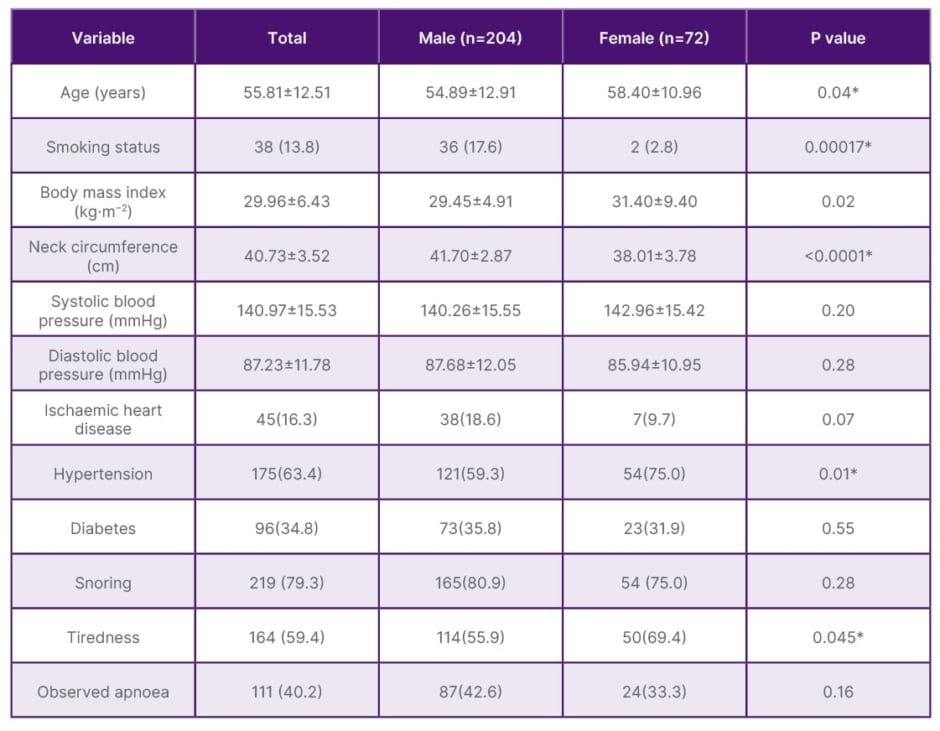
Table 1: Demographics/phenotypes of female and male obstructive sleep apnoea patients.
Data are presented as n (%) or mean ± standard deviation.
*Statistically significant.
N: number.
Sleep Parameters by Gender
As shown in Table 2, total sleep time and sleep efficiency of PSG were significantly better in male patients. The total AHI was similar between the two groups (41.49±23.48 /h for males verses 39.33±26.34 /h for females; p=0.5). Females tended to snore more than males (8.18±11.58% versus 13.41±17.57%, respectively; p<0.05). ESS was comparable amongst males and females (10.81±4.98 in males versus 10.50±5.23 in females; p=0.65). Table 3 shows the clinical phenotypes’ difference between genders.
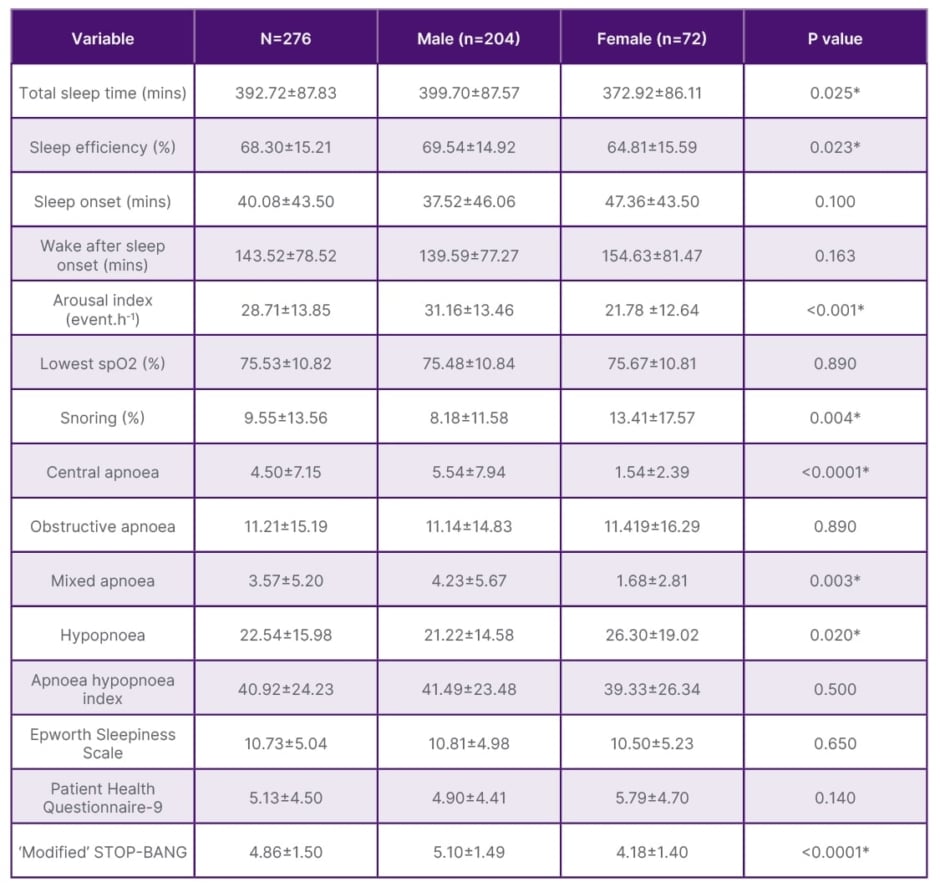
Table 2: Sleep parameters by gender.
Data are presented as n (%) or mean ± standard deviation.
*Statistically significant.
N: number.
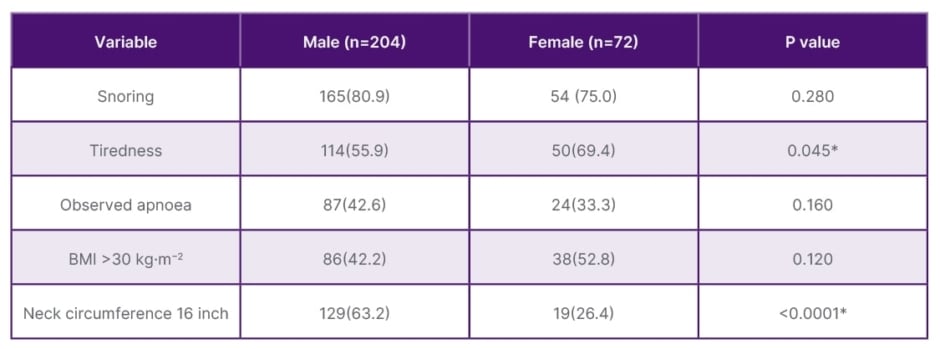
Table 3: Clinical phenotypes by gender.
Data are presented as n (%) or mean ± standard deviation.
*Statistically significant.
N: number.
DISCUSSION
To the authors’ knowledge, there were no recent local studies concerning the prevalence of OSA in patients referred for sleep study, and their phenotypes, in Hong Kong.
Despite that, the majority of referrals were based on clinicians’ knowledge of OSA or patients’ requests, without formal screening tests. In this cohort, the accuracy of referral was high (91%), and only less than 10% of the patients were inappropriately referred. The systematic use of screening tools (ESS, STOP-BANG score) may help the prioritisation of sleep tests according to symptom severity.
This cohort describes the demographic, clinical aspects, and polysomnographic parameters of OSA amongst the population of Hong Kong. First, obesity played a key role in the referral of OSA. The patients were obese with a BMI of 29.96±6.43 kg.m-2 in comparison with the general population, and there was no significant difference between males and females.
However, major differences characterised the phenotypes between males and females. The series showed that female patients with OSA were older, and that BMI was rather similar in both groups (p=0.2); although, the neck circumference in female patients is smaller than that of males. The mean total AHI were similar (p=0.5). The similar rate of sleep apnoea in both genders may be related to ageing and hormonal changes due to menopause in female patients, as oestrogen and progesterone play a protective role in females with OSA.19 The mean age of the female patients was 58.40±10.96 years, while 51 years is the average age of menopause in Hong Kong.20
There is an association between OSA and diabetes, and this cohort found that 34.8% of patients were diabetic. It is similar to a French cross-sectional study with 30.1% of patients with OSA.21
The prevalence of hypertension in the general population (patients aged 65–84 years old) of Hong Kong was 57.4%.22 However, these results showed a higher proportion, with 63.4% presenting with hypertension with a female predominance (p=0.01), attributable to a slightly higher BMI and sleep apnoea in the study. However, under treatment, the majority of them have a good control with a systolic blood pressure of 140.97±15.53 mmHg and diastolic blood pressure of 87.23±11.78 mmHg.
Ischaemic heart disease prevalence was lower than the Sleep Heart Health Study (16.3% versus 23.6%).23 The current results are consistent with the fact that the prevalence of ischaemic heart disease is lower in Chinese compared to Caucasian patients.24 In addition, 43.4% of patients fulfilled the definition of depression according to the PHQ-9 score (≥5) compared to 35%11 in the general population. Sleep apnoea can play a role in the perception of depression due to sleep disruption or hypoxemia.25
In terms of sleep duration, males significantly slept better than females, with a total sleep score 399.70±87.57 mins (p=0.025) and a sleep efficiency of 69.54±14.92% (p=0.023). However, compared to females, their sleep was more fragmented with an arousal index of 31.16±13.46 event/h (p<0.001). The authors supposed that sleep fragmentation was linked to nocturia as it was reported that males with OSA have a 1.5-fold increase in the risk of nocturia, but no significant relationship was found in females.26
Phenotypically, both males and females complained of snoring symptoms (80.9%); but, due to the different perception of symptoms between genders, females reported more tiredness and fatigue (p=0.045), although witnessed apnoea was similar (p=0.16). The study population showed mild excessive daytime sleepiness with an overall ESS of 10.73±10.73, with no difference between genders (p=0.65). Males presented with more central sleep apnoea than females (5.54±7.94 versus 1.54±2.39, respectively; p<0.0001) due to a higher prevalence in underlying ischaemic heart disease.27 Overall, both groups had some component of insomnia with sleep onset of 40.08±43.50 mins, but there is no significant difference (p=0.10).
In summary, the findings show that female and male patients have different OSA phenotypes. On average, female patients referred for sleep tests were older and had a higher BMI than their male counterparts. Despite a lower neck circumference, they tended to snore more than males, due to menopause and hormonal changes. Females tended to complain more about tiredness, and though not statistically significant, they have a longer sleep onset time. Those findings hinted that women can be misdiagnosed as having insomnia or depression instead of OSA. On the other hand, the results suggest that male patients are more likely to be smokers, younger, and have more underlying ischaemic heart disease and hypertensive disease.
Hence, primary physicians should be aware of different clinical phenotypes between males and females to make early diagnosis and intervention to lessen the burden in health outcomes.
LIMITATIONS
The current study has several important limitations. First, this study was conducted in a single centre; therefore, the number of patients recruited was rather small and results could not be generalised to the general population referred for sleep test. Another potential source of bias in the study is related to selection and recruitment; all the patients in this study have been referred by doctors, regardless of the pre-test screening questionnaire. It could therefore lead to an overestimation of the epidemiology.
In addition, time constraints precluded long-term follow-up and sleep questionnaire after continuous positive airway pressure titration and regular continuous positive airway pressure use in terms of symptoms control. Ideally, a longer follow-up period is needed to assess long term improvement of symptoms.
Nevertheless, this small cohort study is relevant in presenting the male-female distribution of OSA in the Chinese Hong Kong population, and may serve as a pilot investigation, shedding light on design and conduct for larger scale studies.
CONCLUSION
The cohort showed that the prevalence of patients referred for sleep tests is high, and referrals are generally appropriate. Phenotypically, patients are in their fifties, obese, and have hypertension, diabetes, and mild depression. Signs and symptoms of OSA differ due to gender features or perception, and physicians‘ awareness and intervention may reduce the adverse health outcomes.







