Abstract
Background and Aims: While patient blood management (PBM) and haemovigilance are different, they are both significant following evidence-based clinical transfusion. PBM is defined as the timely application of evidence-based medical and surgical concepts designed to maintain haemoglobin concentration, optimise haemostasis, and minimise blood loss in an effort to improve patient outcomes. The main aim is to manage patients such that transfusion is only used when the benefits outweigh the risks. Haemovigilance is the set of surveillance procedures covering the entire blood transfusion chain, to minimise the risk of any transfusion-related event to the donor as well as the patient.
In this study, the authors audited, critiqued, and measured their own performance regarding the establishment of PBM and haemovigilance at government sector hospitals of the Regional Blood Centre Karachi, Sindh, Pakistan.
Materials and Methods: A retrospective analysis of the 3.5 years since the establishment of Regional Blood Centre (RBC) Karachi and its associated hospital-based blood banks was conducted. Data were taken from Blood Bank Management Information System software and analysed on SPSS version 23 (IBM, Armonk, New York, USA) . The authors calculated the frequency of transfusion reactions and donor-related adverse events, and also calculated cross match to infusion (CT) ratio and transfusion index.
Results: Initially, the cross match to transfusion ratio was 15:1, but with time and management, at the end of the third year, the team achieved a CT ratio of 1.7:1.0 for different hospitals. Transfusion index was also calculated to be 0.2 at the start of 2020 and 0.8 at the end of 2022. Similarly, no transfusion reaction was reported for the first 1.5 years since RBC’s establishment, and in the later 2 years, 59 reactions were reported. No whole blood was issued, a maximum surgical blood ordering schedule was initiated, and a restrictive transfusion strategy was applied.
Conclusion: While there is still progress to be made, the authors were able to reduce wastage and subsequently suggest the idea of a restrictive transfusion strategy, so that the right blood component is given to the right patient at the right time.
INTRODUCTION
One-fourth of the global population is anaemic, and as the population is gradually increasing day by day, so does the number of anaemia cases. Anaemia causes an increased risk of morbidity and mortality, particularly in reproductive-aged females and children less than 5 years old. The insufficient and inappropriate treatment of anaemia worldwide has also increased social and economic expenditure, reducing technical productivity as output is lesser as compared to the input on anaemic patients.1 As far as hospitalisations are concerned, the risk and severity of anaemia are increased due to several causes such as iatrogenic blood loss.2
Blood transfusion, when not used appropriately, is a dangerous and unsafe procedure.3 However, the appropriate use of transfusion can be safe, effective, and save millions of lives. Unfortunately, in the author’s region, the usage of blood products is a major concern that has not been extensively acknowledged yet. This includes the liberal use of blood products, mismanagement of blood products inventory, the safety of blood products with regards to transfusion-transmitted infections, alloimmunisation, and the lack of health care professional knowledge regarding transfusion.
PBM is a patient-centred, systematic, evidence-based approach to improve patient outcomes by managing and preserving a patient’s own blood, while promoting patient safety and empowerment.4 It involves the timely, multidisciplinary application of evidence-based medical and surgical concepts aimed at diagnosing and appropriately treating anaemia. It also includes the management of coagulapathic bleeding, minimising surgical and iatrogenic blood loss, and supporting the patient while appropriate treatment is required. To summarise, the concept of PBM is to reject the standard code of belief and approach of blood product transfusion in every case.5
The term haemovigilance was extracted from the words hema (blood) and vigilance (surveillance).6 It is a procedure that covers the whole transfusion chain, from collection of blood and its components to monitoring recipients. The objective of haemovigilance is the continuous development of the transfusion chain through corrective and preventive actions to improve patient as well as donor safety, and minimise wastage. Ideally, hemovigilance systems cover the whole transfusion chain and analysis of adverse events and reactions related to blood donation and transfusion.7
Transfusion decisions for acutely ill patients presenting with multiple co-morbidities may become complex and require a more in-depth understanding to minimise risks of transfusion and to identify, treat, and report reactions for health and safety at both the individual and population levels.8
In this study, the authors tried to critique/audit their own performance over the past 3.5 years since the establishment of the RBC. Objective and subjective parameters were utilised to recognise their achievements in the government sector hospitals of Karachi, and to overview their shortcomings in order to rectify them.
MATERIALS AND METHODS
In this retrospective analysis, the authors included all the donors as well as the patients they have treated over the past 3.5 years from January 2020–July 2023. A total of 81,066 donors were accepted at our centres at Sindh Government Qatar Hospital, Sindh Government Lyari General Hospital, and Dr. Ruth K.M. Pfau Civil Hospital Karachi, Pakistan. During this time, 186,767 blood products were issued, including packed red cells, platelets, fresh frozen plasma, cryoprecipitate, and pedi blood bags. Packed red blood cells accounted for 80,888 of products issues. The team calculated the cross match to transfusion (CT) ratio yearly, transfusion index yearly, transfusion reactions, and donor-related adverse events. Subjectively, they reviewed the maintenance of blood product temperature through data loggers, the maximum surgical blood ordering schedule, and the overall impact of their centre over the three government sector hospitals. All the data were analysed on SPSS version 23.
The formula used for calculating CT ratio was: number of units cross matched/ number of units transfused. Ratio of 2.0 or below was considered significant.9 The formula used for calculating transfusion index was: number of units transfused/ number of units cross matched. A value of 0.5 or more was indicative of significant blood usage.9
Formation of hospital transfusion committees was done at each hospital, chaired by the medical superintendent and constituting of a consultant haematologist, medicine and surgery faculty member, gynaecology and paediatrics faculty member, emergency department member, anaesthesia department member, and administrative department member, with anyone else added as needed. The meeting was called once every quarter or as required by the chairperson.
RESULTS
A total of 81,066 donors were recruited in Royal Blood Centre Karachi and its associated hospital based blood banks from January 2020–July 2023. The majority of them were males. Out of these donors, the team had 154 donors with donor-related adverse events (0.18%). Out of the donors who fainted, for most it was their first time donating and it was due to vasovagal shock. All these donors were well managed by the blood transfusion officer (physician) and none of the donors had any serious adverse event. The cause of adverse events is shown in Figure 1. The team received transfusion reaction reports from 59 patients, which is not significant as per the product issuance. Regretfully, they were unable to obtain any transfusion reaction reports prior to June 2021 due to inadequate training in this area. Most of the reactions reported were allergic, followed by febrile non-hemolytic transfusion reactions, as represented in Figure 2.
They calculated CT ratio per year, as shown in Figure 3. In 2020, the ratio was 15:1, and in 2023 a ratio of 1.7:1.0 was reported. The transfusion index was 0.2 at the beginning of the period, followed by 0.8 in the middle of 2023. The subjective analysis of this study will be conferred in detail in the discussion.
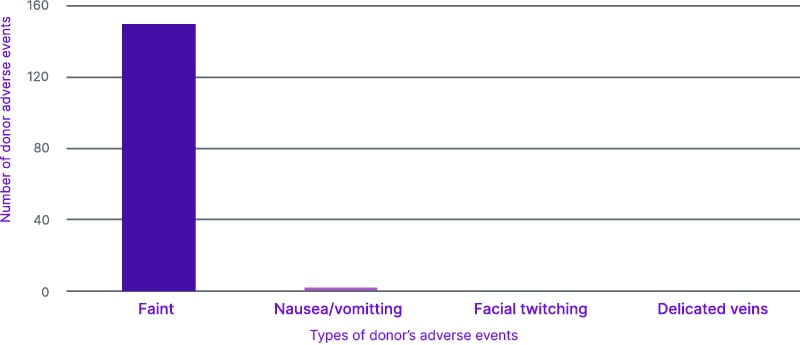
Figure 1: Donor adverse events.
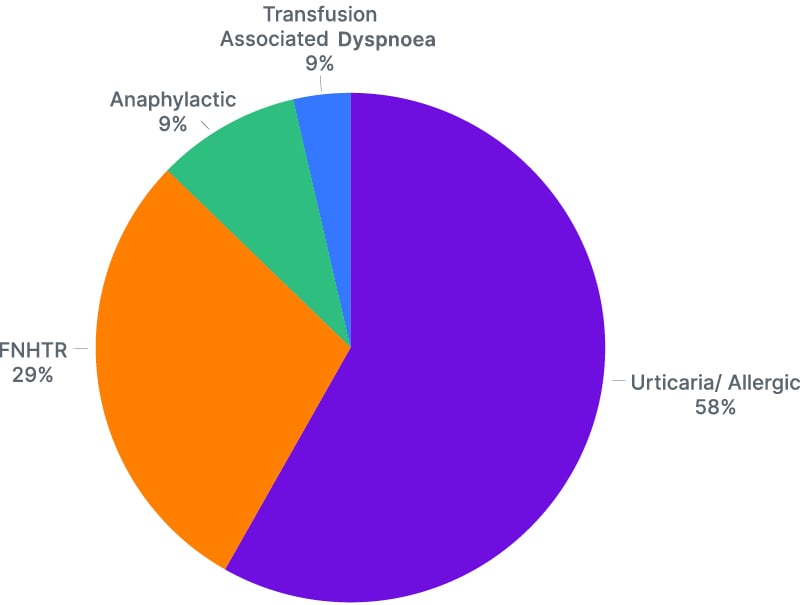
Figure 2: Transfusion reactions.
FNHTR: febrile non-haemolytic transfusion reaction.
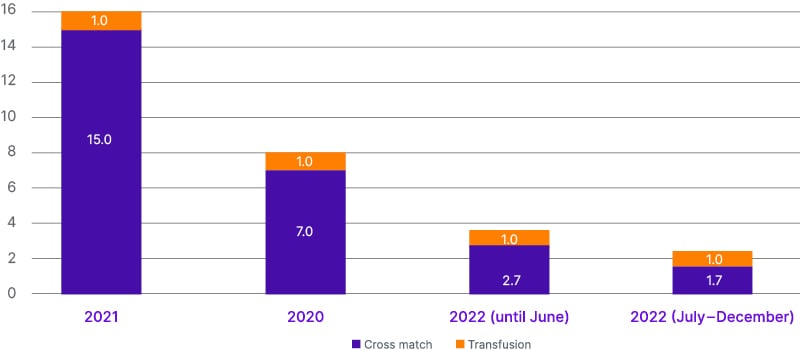
Figure 3: Cross match to infusion ratio annually.
DISCUSSION
Through this article, the authors aimed to critique and audit their performance with respect to PBM and haemovigilance. They were not able to find much data regarding these issues within their region; however, the World Health Organization (WHO) has recognised PBM as an urgent area of intervention due to excessive wastage and irrational use of blood and blood products.10 Ajay Gandhi et al.,11 published an article in India in 2021 regarding the current practices and feasibility in India regarding PBM. They established an interdisciplinary expert group from different fields of both private and government sector hospitals. They developed a questionnaire, consensus statements, and manuscript development. They used evidence and references from previous literature and worked on perioperative diagnosis and management of anaemia. Cases of high-risk bleeders were differentiated from low-risk bleeders, and a consensus on a multidisciplinary team approach in all such settings was made. These findings are contrary to this study because the authors don’t have any such guidelines or literature; however, on a personal level, the team tried to introduce the concept of a maximum surgical blood ordering schedule. This was challenging due to a lack of knowledge among the clinical practitioners. The maximum surgical blood ordering schedule identifies the number of units typically required by 80–90% of the patients undergoing a specific surgical procedure where transfusion is likely.
This assists the clinician in ordering the appropriate number of units of blood for their patient, and was the author’s first step in lowering the CT ratio from 15:1 to 1.7:1. Waheed et al.12 published an article in 2022 regarding the CT ratio of a private sector hospital. It was found to be 1.0:1.0 ratio using retrospective data, which contradicts this study’s findings of 2021 due to the authors working in government sector hospital. The huge amount of workflow at these hospitals means patients land usually in very critical condition with no transfusion medicine team in their departments. The authors conducted continuous medical education and awareness sessions, distributed pamphlets regarding the significance of blood and blood products, and posted posters in all the wards regarding perioperative anaemia management, the restrictive transfusion strategy, and managing anaemia without transfusion. Baig et al.13 in 2020 published an article from Lahore regarding CT ratio, which included government sector hospitals, and the CT ratio was found to be 3.3:1.0. An article from Iran by Alavi-Moghaddam et al.14 reported a CT ratio between 1.4–1.1 in 2014. It was also conducted in a government sector largest hospital of Iran; however, the findings are quite different from this study’s as the country’s transfusion services are quite well developed. The most significant thing Pakistan needs is the addition of transfusion medicine as a physician subspeciality. This will help physicians, and those associated with the ordering of blood products, to understand the significance, dangers, and proper utilisation of blood and its products, and implement the PBM programme more effectively.
Haemovigilance is also a concept that is not extensively discussed by transfusion authorities. The authors aimed to establish it at their local level in order to start a chain of haemovigilance provincially. As their blood bank is associated with three of the largest government hospitals of Karachi, it was quite challenging to maintain this cycle. Samukange et al.15 conducted research across 10 African countries and established, through grading and scoring, that haemovigilance in those countries was suboptimal. The authors of the current study also concluded that the haemovigilance system is underdeveloped; however, over the period of 3.5 years, the team made significant changes to the transfusion setup. Apart from managing the CT ratio and transfusion index, they also introduced a system of blood transport porters, 72 hours rule for cross match, 30 minutes and 4 hours rule of transfusion, maintenance of blood components temperature through transport containers (electronic) and data loggers, as well as doing regular quality control of blood products including the blood cultures. The team also didn’t issue a single whole blood after starting the transfusion service; whereas, the above-mentioned study reported the use of whole blood in many African countries. Demirağ and Hintistan16 published an article in 2020 regarding haemovigilance in nurses. They reported that nurses who had training in haemovigilance had higher frequency of performing better safety procedures than those who didn’t. The authors also recognised this difference since starting the transfusion services compared to now. For the initial 1.5 years, they were unable to get any of the transfusion reaction reported. With continuous training, education, distribution of transfusion reaction forms, and information on how to identify and report these reactions, the team managed to record 59 transfusion reactions over the next 2 years. Though it is still underreported, they took it as achievement, as there was no concept of these reactions before RBC’s establishment. The human resource team was very well trained regarding all these concepts, so 154 donor-related adverse events were reported. The majority of the donors were donating for the first time and had vasovagal shock. Along with a well-trained phlebotomist, the team also had blood transfusion officer (doctors) trained for managing these donors well. The introduction of doctors in the blood collection department was exclusively done by RBC in these government hospitals. The formation of active hospital transfusion committees and regular meetings helped to increase the confidence of the team through discussing and solving issues together. In Asia, Japan has a very good centralised national haemovigilance centre, and they published reports on national level.17 The national blood policy of India has also taken significant steps and established haemovigilance policy on a national level.18
The Pakistan government’s Safe Blood Transfusion Programme took a step making the national transfusion guidelines (2014–2020) and included haemovigilance to be a part of it.19 Their aim was to: “Develop a comprehensive and nationwide hemovigilance system to monitor, evaluate, and improve clinical transfusion practice.”19 This study was in order to evaluate the author’s own performance, as well as to make the authorities acknowledge the need for patient blood management and haemovigilance. Meybohm et al.20 published an article representing the bundle approach in patient blood management instead of individualised. It would be a feasible approach to manage patients and can be acquired on national/provincial level. The WHO has recommended a draft for developing an efficient haemovigilance system in developing countries and following in could be useful.21
CONCLUSION
Patient blood management and haemovigilance are two important indicators in clinical transfusion practice. The data from operating these two systems effectively can be used as a quality indicator for blood transfusion safety, efficacy, and significant utilisation, as well as aid towards evidence-based transfusion medicine. Though the author’s setup lacks many aspects of these, they achieved a remarkable difference over 3.5 years to make transfusion safer and better in government sector hospitals.






