BACKGROUND AND OBJECTIVES
The SARS-CoV-2 2019 pandemic has resulted in a rise in the need for intensive care units (ICU) and mechanical ventilation due to respiratory failure. There is little evidence available on the demographic features of patients in the ICU, as well as changes in respiratory support in the ICU for the management of chest diseases before, during, and after the pandemic. In this research, the team determined whether there was any change in the respiratory support and demographic features of ICU patients with respiratory failure.
MATERIALS AND METHODS
A retrospective observational cohort study was designed in a tertiary teaching respiratory ICU between January 1, 2017–December 31, 2023. Definitions of periods used include pre-pandemic: January 1, 2017–March 10, 2020; pandemic: March 11, 2020–May 5, 2022; and post-pandemic: May 6, 2022–December 31, 2023. During the study period, all patients accepted into the ICU were included in the study. Patient demographics, comorbid diseases, reason for respiratory failure, types of respiratory support (invasive and non-invasive mechanical ventilation, and high flow oxygen [HFO] nasal cannula), length of ICU stay, and mortality were recorded from ICU files. Joinpoint (National Cancer Institute [NCI], National Institutes of Health [NIH], Bethesda, Maryland, USA) and descriptive analysis were done.
RESULTS
Patient demographics and ICU data over the 7-year period were summarized (Table 1). Diabetes, chronic renal failure, and cardiovascular diseases increased in pandemic and post-pandemic periods. The proportion of patients in the ICU that are female (Figure 1A), as well as the rate of female mortality (Figure 1B), had a gradually increasing annual percent of changes (APC) of 2.5 from 2017–2023 (Figure 1A), and during the pandemic, this increased to an APC of 12.5 (Figure 1B). Mechanical ventilation (invasive and noninvasive) gradually decreased in pandemic and post-pandemic periods; whereas, HFO use increased. Mortality of patients had an APC of 11.49 after 2019.
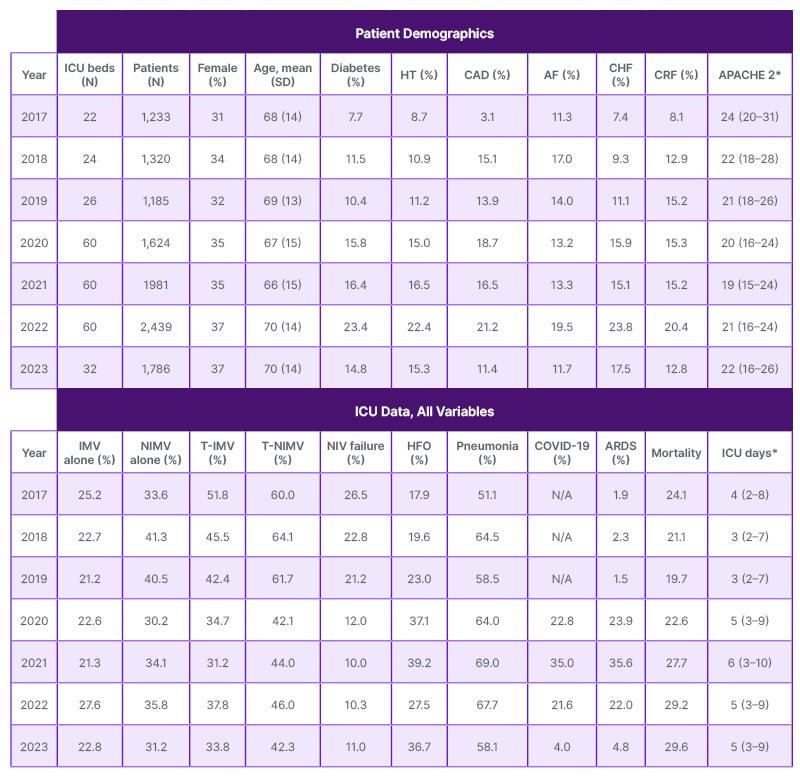
Table 1: Characteristics in pre-pandemic, pandemic, and post-pandemic years of Level 3 intensive care unit patients.
*Values median (25–75%).
AF: atrial fibrillation; APACHE 2: acute physiologic and chronic health evaluation 2; ARDS: acute respiratory distress syndrome; CAD: coronary artery diseases; CHF: congestive heart failure; CRF: chronic renal failure; HFO: high flow oxygen; HT: hypertension; ICU: intensive care unit; T-IMV: total invasive mechanical ventilation (IMV after NIVM or IMV alone); T-NIMV: total noninvasive mechanical ventilation (NIMV after IMV or NIMV alone).
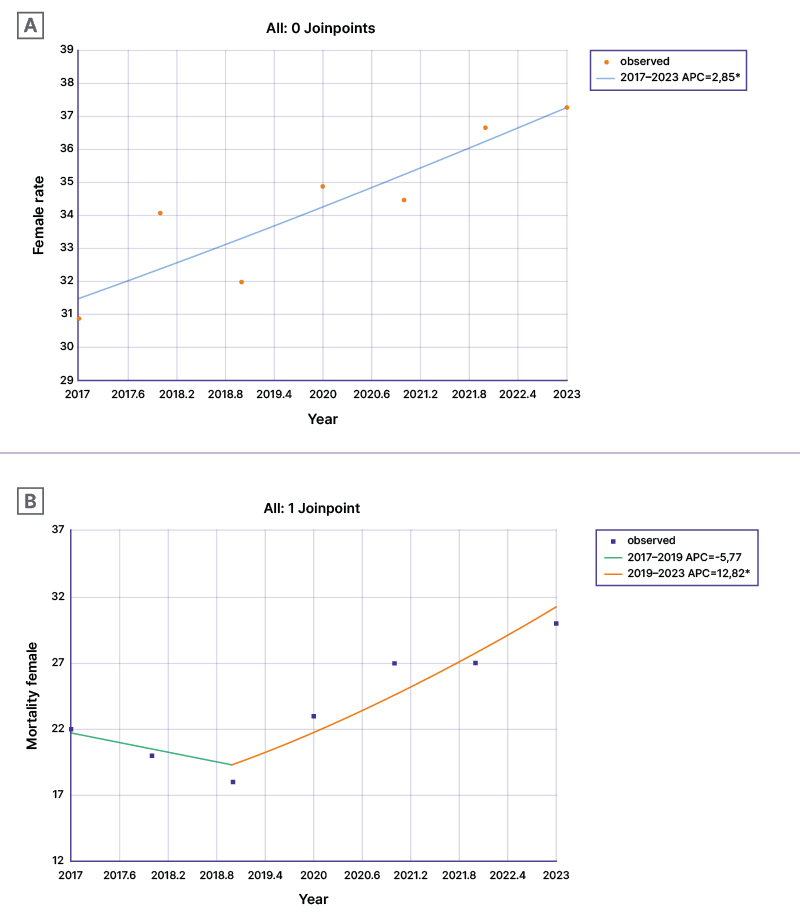
Figure 1A & 1B: Female mortality in the intensive care unit in pre-pandemic, pandemic, and post-pandemic periods.
*Indicates that the APC is significantly different from zero at the alpha=0.05 level. Test statistic and p-value not available for the empirical quantile method. Final selected model for Figure 1A is 0 Joinpoint and for Figure 1B is 1 Joinpoint. APC: annual percent change.
CONCLUSION
While the proportion of female patients in ICUs has increased over the years, and female mortality continues to increase during and after the pandemic, cardiovascular and renal diseases are more prominent post-pandemic. As HFO increased in use with the pandemic, a decrease in mechanical ventilation applications was seen, marking the most prominent difference in respiratory ICU during the pandemic.







