COVID-19 has revealed a pandemic of another kind: existing health inequities between population groups. We explore the role and responsibility of medical affairs teams in addressing imbalances and forging a fairer and more inclusive health landscape for the future
Isabel O’Brien
While pandemics were once safely absconded in sci-fi dystopia or high school history books, last year, a space was reclaimed in our reality. But what if COVID-19 was the louder, more visible cousin of another pandemic?
The virus has revealed systemic health inequities within society, so while the world is set on returning to normality, how can the pharmaceutical industry taper the return so that these inequities are addressed and prevented in the future?
Increased risk
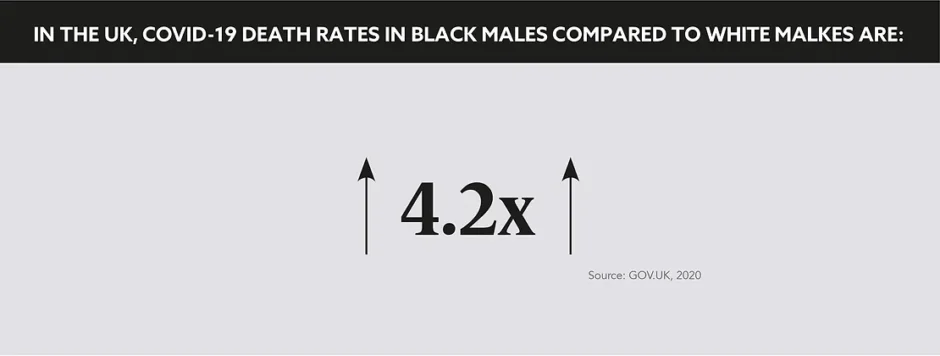
A report released last May by Public Health England revealed that people of Chinese, Indian, Pakistani, Other Asian, Black Caribbean, and Other Black origin had a 10–50% higher risk of fatality after contracting COVID-19 when compared to those classed as White British.
“Sadly, it was apparent from the early stages of the pandemic that some populations are at a much higher risk of experiencing a more severe disease course and death than other groups,” says Francois Gavini, Head of Evidence Generation Europe and Canada, Takeda.
Some populations are at a much higher risk of experiencing a more severe disease course and death than other groups
So while we must scrutinise societal and economic factors that increase the risk of exposure, with research showing that BAME (Black, Asian and Minority Ethnic) groups are more likely to live in urban, heavily populated areas and be occupying front-line jobs. Pharma has a duty to address another discriminating factor: the higher rate of comorbidities in these population groups.
“The pandemic has exacerbated the health inequities that vulnerable populations have been experiencing around the world,” confirms Sarah Jarvis, Global Lead Medical Affairs Practice, ZS Associates.
Higher comorbidity rates
We all remember the rolling news broadcasts of the early pandemic, urging those with conditions such as diabetes and hypertension to remain confined to their homes. What has become apparent since then is that contracting these diseases is far from a lottery.
Diabetes was listed as a pre-existing condition in only 18% of White ethnic group deaths, compared with 45% of Black groups, with deaths involving hypertensive disease ranging from 17% in the White ethnic group to 40% in the Black group. For reasons that must be uncovered, members of BAME communities markedly suffer with what the medical profession considers to be largely preventable health conditions.
However, behind this grim discovery lies an opportunity for change. Now that the disparity has been identified, the industry, and medical affairs in particular, must use their skills to investigate the causes of the imbalance.
What can pharma do?
“As the scientific and medical face of the pharma industry, it is the responsibility of medical affairs teams to work with physicians, researchers, and patient communities to disseminate the facts and bring about clinical change,” says Gavini.
These groups can pool their expertise in epidemiological studies, which are designed to decipher how often diseases occur in different groups of people and to unravel the factors that contribute to these differences.
“Medical affairs can drive research to provide additional epidemiological evidence and clinical insights into how such factors drive inequities in health outcomes for COVID-19,” says Gavini. Studies of this kind evaluate illness prevention strategies and can establish industry guidebooks for supporting patients in whom the disease has already developed.
Once gaps have been identified, disparities will need to be addressed with targeted, industry-led outreach initiatives. These should empower communities to reduce the rate of preventable comorbidities by improving overall access to health information and ensuring unique triggers are addressed on a population-by-population basis.
Trust is key
“MA organisations can become the trusted partner for BAME communities by using appropriate resources such as virtual trials or telemedicine to understand their core issues such as quality of life and existing comorbidities to address prominent needs within the community,” adds Jarvis.
While it is vital to understand how inequities are formed and immediately action rectifiers, this mission must also be forward-facing. Companies must establish long lasting bonds with BAME communities by ensuring their internal fabric is as diverse as the populations they serve.
“Establishing a close connection with BAME communities starts with ensuring that these less privileged communities are well-represented within the organisation itself, across their key external stakeholders (e.g. KOLs) and in their patient support programmes and activities,” says Jarvis. Looking inwards and adjusting accordingly will show a lasting commitment to improving health outcomes in the long-term.
While COVID-19 has revealed dramatic inequities, the industry now has the opportunity and to address imbalances and create a fairer, more inclusive outcomes. This is undoubtedly a secondary pandemic, a trend seen not just in the UK, but globally, and this prevalence must be tackled with as much aligned vigour and urgency as the COVID-19 virus.