Meeting Summary
This 1-day meeting was held at the Austria Trend Savoyen Hotel, Vienna, Austria. The afternoon, chaired by Dr Hong Liang and Dr Rachel Bishop, consisted of a series of case presentations focussed on the treatment of ocular manifestations resultant of cystinosis, including the use of the novel gel-like formulation of cysteamine. Dr Inês Leal presented a series of four cases from the Hospital de Santa Maria, Lisbon, Portugal, illustrating the importance of early administration of treatment. Dr Giancarlo Iarossi presented a case highlighting the various examination techniques available to evaluate morphological and functional change during follow-up. Mr Susmito Biswas presented an interesting case of ocular cystinosis with concurrent congenital glaucoma, which brings a number of challenges. Dr Carla Ferreira presented two cases from the Hospital São João, Oporto, Portugal, that had two very different outcomes. Finally, Dr Eleonora Maria Soler Pava presented two cases from her clinic in Bogotá, Colombia, highlighting the good prognosis for patients when continual treatment is available.
Ocular Cystinosis: Clinical Experience in Adult Patients
Doctor Inês Leal
Case 1 reported a 28-year-old female patient diagnosed at the age of 25 years. During investigations for severe hypertension and renal failure during pregnancy the patient was sent to the ophthalmology department for exclusion of hypertensive retinopathy. Corneal crystals were found, suggesting juvenile nephropathic cystinosis, further confirmed by elevated levels of leukocyte cystine. The patient was prescribed systemic and topical cysteamine with visible reduction of corneal crystal deposition by slit lamp biomicroscopy observation 6 months after starting treatment (Figure 1). She is currently on haemodialysis awaiting a renal graft.
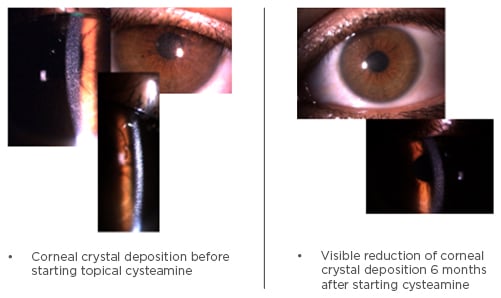
Figure 1: Reduction of corneal cystine deposition after 6 months of cysteamine treatment.
Case 2 detailed a 20-year-old male patient diagnosed with infantile nephropathic cystinosis at the age of 1 year. He has been on systemic and topical cysteamine since diagnosis, however there are continued corneal crystals despite years of therapy.
Case 3 described a 42-year-old male patient diagnosed with juvenile nephropathic cystinosis at the age of 41 years. After diagnosis, the patient began systemic and topical cysteamine. Although there has been no obvious decrease in corneal crystal deposition by slit lamp biomicroscopy observation, the patient reports a decrease in photophobia and foreign body sensation, and improved quality of life.
Patients 1, 2, and 3 have had continuous multidisciplinary follow-up since diagnosis. Despite having multiple keratic crystals, visual acuities remain normal and there are no other changes in the complete ophthalmological exam, with no crystals in the iris, angle, or retina.
Case 4 is a 42-year-old female patient diagnosed with infantile nephropathic cystinosis at the age of 2 years. This patient had no regular treatment or follow-up and only started topical cysteamine at the age of 40 years. The patient has bilateral end-stage corneal disease and is legally blind in both eyes.
Three patients have been switched from pharmacy preparation topical cysteamine to the gel-like formulation. The Ocular Surface Disease Index (OSDI) questionnaire1 was applied before the switch and 3 months afterwards. The OSDI is a validated questionnaire, which is available for ocular surface disease (OSD), specifically for dry eye, and is designed to provide rapid assessment of the symptoms related to OSD and their impact on vision-related quality of life. Answers are graded from 0 (none of the time) to 4 (all of the time). Total score is calculated using the (sum of scores for all questions answered) x 100 / (total number of questions answered) x 4. This questionnaire addresses items over the past week including: sensitivity to light; gritty, painful eyes; blurred vision and limitations in reading; driving at night, working on a computer; being uncomfortable in windy conditions and areas that are air conditioned etc.
While two patients had an improvement in OSDI score, OSDI deteriorated for one patient, although this patient was known to have poor adherence to therapy. Sensitivity to light, sore eyes, blurred vision, and poor vision were the most common complaints reported. All patients felt that the 1-week stability of this new formulation was more convenient and improved quality of life. One patient felt that the consistency of the gel formulation constrained the eye drop installation.
Key Learning Points
- Nephropathic cystinosis-related cystine crystal accumulation in the eye may lead to end-stage corneal disease and poor visual prognosis if not promptly and continuously treated
- Early treatment with topical cysteamine may lead to better outcomes
- The new gel-like formulation is an alternative to conventional cysteamine eye drops
- Stability at room temperature is an important aspect for patients
- This formulation may improve quality of life, adherence, and ultimately the effectiveness of corneal depletion of topical treatment
- Although promising, this new formulation will require longer follow-up to evaluate efficacy and safety
Functional and Morphological Evaluation of Ophthalmic Pattern in a Young Patient Affected by Cystinosis
Doctor Giancarlo Iarossi
A female 13-year-old patient diagnosed with nephropathic cystinosis at the age of 3 years in Romania was reported. She did not receive treatment due to the lack of availability of cysteamine, and at initial observation presented with growth retardation, poor appetite, vomiting, dehydration, acidosis, and hypertension. A diagnosis of cystinosis was confirmed with leukocyte cystine level and ophthalmic evaluation, followed by genetic analysis, revealing a 57 KB deletion in the CTNS gene. The patient began treatment with cysteamine and had progressive decay of renal function; she has been on dialysis since February 2016 while awaiting a kidney transplant. The patient was on growth hormone therapy, as well as treatment for hypertension and hypothyroidism, and had mild photophobia, a best corrected visual acuity of 20/20, and was taking cysteamine gel-like drops four times a day.
Corneal crystals can be seen on anterior-segment optical coherence tomography (OCT) and Scheimpflug camera, which can provide a direct and objective measurement of the density or opacity of the cornea. However, in this patient, no relevant alterations were seen on topography or on using the aberrometric test, although some artefacts were present due to squinting. In addition, no relevant alterations were seen at the posterior pole and peripheral retina, and the macular OCT scan was within the normal range. To evaluate retinal function, the patient underwent flash Ganzfeld electroretinogram (ERG). The International Society of Clinical Electrophysiology of Vision (ISCEV) protocol was not applied, as pupil dilation may have been too difficult for the patient to tolerate; instead, photopic and mesopic stimuli were used, measuring the pupil diameter before and after the test. The response to photopic stimuli was normal, however there was a significantly reduced response to mesopic stimuli, indicating possible dysfunction of the peripheral retina.
This confirms that future studies are needed to better characterise the possible sites of retinal dysfunction in patients affected by cystinosis. During the Question & Answer (Q&A) session it was suggested that ERG may be a way to monitor function for patients in whom crystals cannot be seen on retinal evaluation. It was highlighted that aside from crystals there may be other mechanisms underlying the dysfunction, e.g. impairment of the mechanistic target of rapamycin (mTOR) signalling pathway.2 During the discussion, the need for standardised testing was raised; various types of tests and the frequency of application during follow-up were considered. The availability of more standardised tests is essential, as this will permit comparability between studies, which is particularly important when the patient numbers are so small.
Key Learning Points
- The presence of corneal crystals in this case did not affect visual acuity, causing only mild photophobia
- Long-term therapy with cysteamine (including gel-like drops) was effective in controlling symptoms and maintaining a relatively stable corneal condition over almost 10 years
- The presence of corneal crystals did not alter the aberrometric pattern in this case
- Despite a normal fundus appearance, alterations were observed on ERG suggesting early retinal dysfunction
- Further evaluation using the ISCEV protocol is needed
Cystinosis Case Presentation
Mr Susmito Biswas
The case was presented of a 5-year-old male, born at term following a normal delivery, with a history of infantile nephropathic cystinosis with elevated white blood cell cystine, growth delay, and renal Fanconi syndrome. He also presented with moderate-to-severe photophobia and one eye larger than the other. He was taking oral cysteamine bitartrate 200 mg four times a day, together with electrolyte replacement therapy and other treatments for retinal complications. He was not receiving any topical ocular medication at the time of referral. On examination, visual acuity was 6/6 in the right eye and 6/9.5 in the left eye. It was difficult to adequately assess for the presence of any relative afferent pupillary defect due to severe photophobia.
At presentation, the patient had increased corneal diameters (horizontal corneal diameter in the left eye was >13 mm), typical corneal, conjunctival and iris crystal deposition, and Haab’s striae. The anterior chambers were deep and there were no posterior synechiae. Intraocular pressures (IOP) were within the normal range, 13 mmHg in the right eye and 14 mmHg in the left eye, measured with Goldman applanation tonometry. Continued observation demonstrated stable visual acuity but increasing IOP. He received topical cysteamine 0.55% approximately three times daily and was commenced on anti-glaucoma treatment by latanoprost 0.005% and combined timolol 0.5% and dorzolamide 2.0%. During the course of follow-up, his IOP gradually increased to 40 mmHg in the left eye, and the patient underwent left diode laser cycloablation, which failed to sufficiently lower his IOP. He subsequently underwent left combined trabeculotomy with anti-metabolite (5-fluorouracil, 7.5 mg).
After >10 years of follow-up, the patient is stable with a visual acuity of 6/6 in the right eye and 6/7.5 in the left. He has an established, but stable, glaucomatous field defect in the left eye and normal visual fields in the right eye. His IOP is 20 mmHg in each eye and he is currently taking ongoing treatment with latanoprost, combined timolol 0.5% and dorzolamide 2.0%, and topical cysteamine 0.55%.
This patient has dual pathology of both cystinosis and congenital glaucoma which posed several challenges; because both conditions present with photophobia, examination and IOP measurements can be difficult and fundus examination may be limited. The topical management of cystinosis can also be compromised by the need for multiple eye drops for other conditions (e.g. glaucoma, postoperative management) and other oral and systemic medications, all of which can challenge compliance. In this case, it was supposed that the dual pathologies were coincidental, however there are long-term changes that occur in the anterior segment with cystinosis that increase the risk of glaucoma, such as posterior synechiae formation, leading to iris bombé and acute angle closure, and progressive narrowing of the angle due to changes in the ciliary body, which can mimic plateau iris configuration (Figure 2).3

Figure 2: Angle closure over time in cystinosis.3
Reproduced with permission from [JAMA Ophthalmology. 2000. 118(10):1329-33]. Copyright©(2000) American Medical Association. All rights reserved.
It was highlighted that oral cysteamine treatment is not effective against corneal cystine crystal deposition. Topical cysteamine has been shown to reduce the accumulation of corneal crystals;4 however, it must be administered frequently and the stinging upon administration limits tolerability. A novel gel-based formulation of cysteamine administered four times daily has been shown to significantly reduce crystals in patients using a less frequent drop regime as measured with in vivo confocal microscopy (IVCM) scores after 3 months.5 The scores remained stable for up to 4 years, despite a reduction in the frequency of installation.5
During the Q&A it was noted that the increased corneal thickness in cystinosis can influence IOP measurement, possibly artificially raising the pressure.6,7 In addition, the composition of the cornea is not standard due to the presence of crystals, which may also influence the IOP due to altered corneal biomechanical properties, although this needs further study to corroborate. Annual anterior segment OCT was suggested as a way of monitoring for risk of narrow angle glaucoma development.
Key Learning Points
- Concurrent congenital and infantile glaucoma and ocular cystinosis present a challenge to ophthalmologists because of their similar clinical presentation and difficulties in performing examination
- Long-term glaucoma remains a challenge to correctly identify and treat
Ophthalmology Case Reports: A Journey Through Another Era
Doctor Carla Ferreira
The first case presented a 4-year-old girl sent from Belgium in 2001 with pulmonary valve stenosis, growth retardation, and proximal tubulopathy with chronic renal failure. On physical examination she had hepatomegaly and splenomegaly, and hypertension was noted. Further investigations revealed aortic valve stenosis, some haematological abnormalities (hypochromic microcytic anaemia, leukopenia, thrombocytopenia), urine sediment and biochemistry alterations, and osteopenia. Leukocyte cystine levels were 9.7 nmol hemicystine/mg protein. The patient was then referred to the ophthalmology department where photophobia was reported, visual acuity was found to be 6/10, and on biomicroscopy there were numerous iridescent crystals throughout the cornea; fundoscopy was normal. The patient was started on oral cysteamine and several supportive medications, however she died the following year while awaiting approval for growth hormone treatment and cysteamine eye drops.
The second case described an 8-month-old male investigated for failure to thrive and growth retardation in 2009. Fanconi syndrome, metabolic acidosis, hypophosphatemia, proteinuria, and glucosuria were all found, and his bone density was lower than expected for his age. Leukocyte cystine levels were 3.1 nmol hemicystine/mg protein. The patient was started on oral and topical cysteamine, electrolyte replacement, and indomethacin. When the patient was referred to the ophthalmology department, he was already receiving the cysteamine eye drops, and no symptoms were noted. Visual acuity was 8/10, biomicroscopy and fundoscopy were normal. At the age of 3 years, photophobia was reported, and at 6 years old, scarce iridescent crystals were noted for the first time. At the patient’s most recent appointment at the age of 7 years, he had photophobia, his visual acuity was 10/10, and objective refraction was +0.50 +0.50 x 90° (diopters). On biomicroscopy, the iridescent crystals in the cornea had disappeared; fundoscopy was normal.
Currently, the patient still has some growth retardation, while haematology and biochemistry are normal. He was since diagnosed with lymphocytic thyroiditis. Leukocyte cystine levels are good, 0.37 nmol hemicystine/mg protein. He is currently taking cysteamine eye drops every 2 hours. It is unclear as to why the patient has photophobia when crystals cannot be seen on biomicroscopy; it was speculated that there may still be crystals that are undetectable and that confocal microscopy or OCT at the cellular level observation may be able to identify crystals. In the Q&A session, it was suggested that meningeal irritation from raised intracranial pressure may be a factor to consider in patients with unexplained photophobia.
Key Learning Points
- Early access to treatment may improve outcomes
- Symptoms of photophobia may still be experienced when the patient does not have crystals in the cornea on biomicroscopy
- This may be due to subclinical levels of crystals; more detailed imaging techniques may be useful to detect these crystals
Ophthalmology Case Reports
Doctor Eleonora Maria Soler Pava
The first case detailed was a male patient aged 2 years and 9 months. His mother had gestational diabetes and at birth he was macrosomic with hypoglycaemia. At 6 months old, he presented with hypokalaemia and was suspected to have renal tubular acidosis. By 8 months, he presented with a number of metabolic disturbances (including phosphaturia, glucosuria, hypokalaemia, elevated urine potassium, and metabolic acidosis) and Fanconi’s syndrome was diagnosed. Over the next 5 months he constantly presented with metabolic acidosis, electrolyte imbalances, and progressive nitrogen elevation. At 10 months he had his first ophthalmological exam, which was normal, and at 13 months he was diagnosed with Stage 5 chronic kidney disease. Genetic screening revealed he was a double heterozygote carrier of mutations c.18_21delGACT and c.1015G>A in the CTNS gene. Corneal crystals and an elevated optic nerve head were found in both eyes, and the patient was diagnosed with infantile nephropathic cystinosis.
He started treatment with oral and topical cysteamine at 15 months, together with several supplementary treatments. He had complications of hypoparathyroidism and anaemia. At the age of 2 years and 9 months the patient underwent a second ophthalmological exam; he had no symptoms of photophobia, dry eye, or irritation. He had good visual acuity and ocular motility was normal. On slit lamp biomicroscopy there was mild accumulation of crystals in both eyes, fundus examination was normal. Drusen were observed in the optic nerve head of both eyes on ultrasound. On OCT, crystals could be observed on the surface of the cornea but not the rest of the stroma. The patient was on cysteamine eye drops for 1 year and then had to stop for 3 months because of lack of availability of the medication. He has been on gel-like cysteamine drops for 2 months, one drop in each eye taken every 6 hours. On his last nephrology examination, he was found to have Stage 3 chronic kidney disease. His leukocyte cystine levels were still somewhat high (10.4 nmol hemicystine/mg protein), although his anaemia had improved and hypoparathyroidism was stable.
Obtaining authorisation for the medication from the insurance companies is difficult for patients in Colombia, and access to treatment can be irregular. In addition, patients may need to travel long distances and therefore getting access to specialists is difficult; there may be many undiagnosed patients. It may also be difficult to do the slit lamp exam and OCT when patients are very young.
The second case described a female aged 5 years and 1 month whose mother had gestational diabetes. She presented at 13 months with hypokalaemia and was diagnosed with renal tubular acidosis. At 17 months, she had her first ophthalmological exam due to a suspicion of Fanconi’s syndrome, which was normal. At 23 months, genetic screening found that she had a homozygous pathogenic duplication in p.Thr216Asn fsx226 in the CTNS gene. She was diagnosed with infantile nephropathic cystinosis and ophthalmological exams were performed every 6 months up to 3 years and 8 months of age; normal corneas were noted with no evidence of crystals.
An ophthalmological exam at the age of 3 years and 9 months revealed mild photophobia with no dry eyes or irritation. Visual acuity was 20/30 in both eyes. Ocular motility and fundus examination were normal, but corneal crystals were observed. The patient started oral cysteamine at 20 months and cysteamine eye drops at 4 years, used for 6 months. The patient has recently started cysteamine gel-like eye drops, administering one drop on each eye every 6 hours. The patient has mild photophobia, good visual acuity, and there is mild-to-moderate crystal accumulation in the cornea, with few crystals on the iris surface and the anterior capsule of the lens.
Key Learning Points
- Prognosis is good if a continuous supply of cysteamine eye drops is possible
- Difficulties with receiving access to medication and specialists may be an issue in some countries








