BACKGROUND AND AIMS
Thalassemia is a group of haemoglobinopathies characterised by the decrease or lack of β or α globin chain production haemoglobin (Hb).1 Minor thalassaemia has little to no symptoms since the other gene is capable of compensating for the anomaly; however, it represents a rare cause of resistance to erythropoietin (EPO) in patients with chronic haemodialysis (CHP) in multiple regions, particularly the Mediterranean region.2 As a matter of fact, patients on CHP affected by minor thalassaemia often take higher EPO doses to correct the anaemia even if all causes of EPO resistance are resolved;3 a recent Italian investigation indicated that EPO need in this population is almost double in comparison to other groups.4 EPO resistance can be secondary to the quantitative anomalies of the haemoglobin chain, notably Hb A2 and Hb F. Di Lorio et al.5 reported a positive correlation between the percentage of Hb A2 and EPO doses.5 Patients that had a Hb A2 >6% needed higher EPO doses and vice versa. The aims of this study were to evaluate the efficiency of different therapeutic means, erythropoiesis-stimulating agents (ESA) and blood transfusion (TS), aiming to correct the anaemia in CHP with minor thalassaemia; and to detect the correlation between quantitative anomalies in Hb chains and EPO resistance.
MATERIALS AND METHODS
This descriptive, multi-centre study involved eight patients on CHP affected by minor thalassaemia confirmed on electrophoresis of Hb at least 12 months prior, presenting with anaemia (Hb <10g/dL) and under-treatment by erythropoietic stimulating agents (ESA) ±transfusion, with a regular follow-up mainly of the Hb and ferritin. Statistical analysis of the data was performed through Excel using the correlation coefficient and SPSS using the p-value. A value <0.05 was considered as significant.
RESULTS
The average value of Hb was 7.35 g/dL; mean ferritin: 964±971 ng/L; and mean parathyroid hormone levels: 433±126 pg/mL. Electrophoresis was done for all patients with averages for Hb A: 96.2±1.7%; Hb A2: 3.43±1.41%; and Hb F: 0.35±0.45%. The authors noted that a decreased percentage up to null of Hb F fraction correlated with the lowest Hb levels. The main therapy in patients with anaemia was epoetin β; the average dose given to patients was 300 UI/kg/week, 326 UI/kg/week at 2 months, 233 UI/kg/week at 6 months, and 326 UI/kg/week at 12 months. Figure 1 illustrates the response to EPO during the maintenance phase. Darbepoetin α (μg/kg/s) was administered (depending on availability) to two patients out of eight. One of the two received a dose of 0.57 μg/kg/week for 8 weeks, the other one received a dose of 0.7 μg/kg/week for 8 weeks, with a different response in the two patients. Regarding TS, five patients in the series received a TS of an average of one red blood cell pellet every 3 months, given the poor clinical tolerance of the anaemia. Injectable iron was administered in two patients out of the eight ahead of the low levels of ferritin (<300 ng/L).
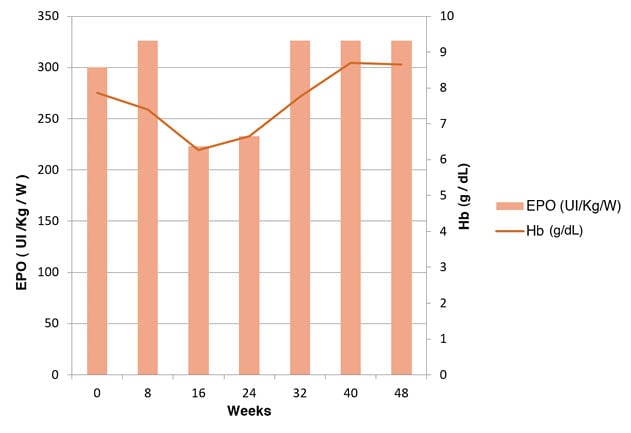
Figure 1: Erythropoietin doses and haemoglobin values during the maintenance phase.
EPO: erythropoietin; Hb: haemoglobin.
CONCLUSION
The presence of minor thalassaemia in CHP entails EPO resistance and a serious case of anaemia. In the authors’ study, the maximum EPO dose used was 500 UI/kg/week, reaching a value of 9.7 g/dL of Hb. ●








