Acute kidney injury (AKI) is a global problem that occurs in the community and in the hospital, both in the intensive care unit (ICU)1 and outside this environment. The in-hospital mortality rate is ˜20–50%.2 AKI also increases the risk of chronic kidney disease (CKD) and end-stage renal disease (ESRD) and may result in damage to non-renal organs.
This was a retrospective study to evaluate the outcomes of patients admitted to a nephrology department with the diagnosis of AKI. Patients admitted to our service with a diagnosis of AKI, according to the Kidney Disease: Improving Global Outcomes (KDIGO) classification for 5 years, were evaluated. The following endpoints were evaluated in the follow-up period: progression to ESRD, all-cause mortality, in-hospital admission for stroke, acute coronary syndrome (ACS), or heart failure (HF). Data were collected from medical records. Patients without records or with an unknown serum creatinine value in the 12 months prior to this AKI episode, and those who needed treatment in the ICU, were excluded. Survival analysis was carried out by the Kaplan–Meier method and potential risk factors for ESRD by Cox regression.
We included 191 patients, 113 (59.2%) were male, the mean age was 73.83±12.49 years, and 137 (71.7%) patients had a history of CKD. Comorbidity distribution based on the Charlson comorbidity index was <3 points (n=22; 11.5%), 4–5 points (n=32; 16.8%), 6–7 points (n=59; 30.9%), and >8 points (n=78; 40.8%). The median length of stay was 12 days. Pre-renal AKI was assumed in 128 patients (67%), while intrinsic AKI occurred in 45 (23.6%), and post-renal AKI was seen in 15 (7.9%). In three patients (1.6%), the cause of AKI was undetermined. Thirty-three patients (17.3%) had AKI Stage 1, 11 (5.8%) had AKI Stage 2, and 147 (77%) had AKI Stage 3.
Renal replacement therapy (RRT) was needed for 124 patients (65%), 65 (34%) received only pharmacological treatment, and 2 (1%) needed surgery. At discharge, 107 patients (56%) had recovered renal function to the values they presented before the AKI episode, 41 (21.6%) presented serum creatinine levels above the basal values but without need of RRT, 25 (13%) evolved to ESRD, 16 (8.4%) died, and 2 (1%) had unknown outcomes. Four patients were lost to follow-up. Overall, the median survival time free of RRT was 74 months and 69 months (38.24–99.76) in the group of patients with a history of CKD; in patients without previous CKD, it has not yet been reached (p<0.05). The only factor associated with progression was history of CKD (hazard ratio: 2.37; 95% confidence interval [CI]: 1.23–4.56) (Table 1). The median survival time in this sample was 34 months (95% CI: 23.3–44.7) and the mortality rate was 18 deaths/100 patient-years. After the AKI episode, 22 patients (11.5%) had at least one hospital readmission for HF, 5 (2.7%) were rehospitalised for ACS, and 6 (3.1%) were readmitted due to stroke. The incidence of a composite cardiovascular endpoint of HF, ACS, and stroke, was 6 events/100 patient-years.
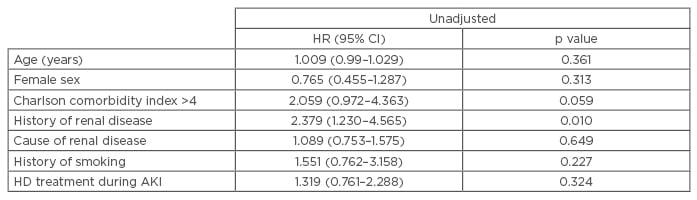
Table 1: Hazard ratio of possible factors associated to progression from acute kidney injury to end-stage renal disease.
HR: hazard ratio; CI: confidence interval; HD: haemodialysis; AKI: acute kidney injury.
The outcomes of the patients admitted in our service with AKI were different to those we find in the literature. We confirmed that patients with a history of CKD are prone to ESRD after an admission for AKI. The rate of admission for a cardiovascular event in our study was lower than that described in the literature because the median survival time of our patients was similar to the median survival time of a cardiovascular event.








