The aim of this study was to compare the survival observed in patients with moderate-to-severe functional mitral regurgitation (FMR) and moderate-to-severe symptomatic heart failure (HF) treated with MitraClip® and the survival predicted by available HF scores: the Seattle HF Model (SHFM),1 the HF calculator of the meta-analysis global group in chronic HF (MAGGIC),2 and the Cardiac and Comorbid Conditions HF (3C-HF)3 score. From 2008–2015, 171 patients with moderate-to-severe HF received MitraClip at two institutions. Patients were stratified in two subgroups according to the aetiology into non-ischaemic FMR (n=64) and ischaemic FMR (n=107). We compared the observed survival with that predicted by these scores at different time points for the overall population and for the two subgroups.
We found that: i) the survival predicted by the SHFM and the MAGGIC scores were consistent with those observed after MitraClip, with a trend of higher observed survival compared to that predicted by the MAGGIC, ii) the survival predicted by the 3C-HF score was lower than that observed after MitraClip (Figure 1), and iii) the results were consistent in the subgroup analysis for non-ischaemic and ischaemic FMR aetiology, with non-ischaemic patients showing the highest observed survival rates compared to the 3C-HF scores (Figure 2).
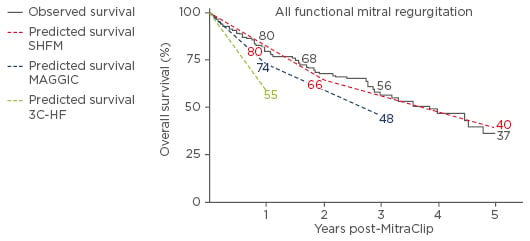
Figure 1: Kaplan–Meier analysis of overall survival compared to the predicted by the available HF scores in all FMR patients.
SHFM: Seattle Heart Failure Model; MAGGIC: meta-analysis global group in chronic heart failure; 3C-HF: Cardiac and Comorbid Conditions Heart Failure score; HF: heart failure; FMR: functional mitral regurgitation.
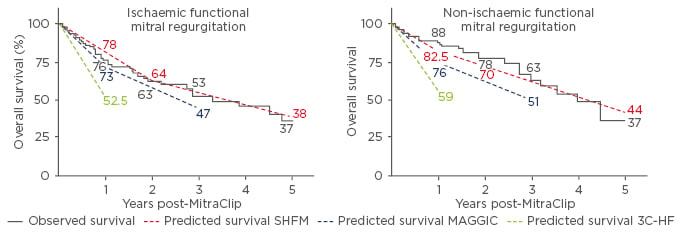
Figure 2: Kaplan–Meier analysis of overall survival compared to the predicted by the available HF scores in ischaemic (left) and non-ischaemic (right) functional mitral regurgitation patients.
SHFM: Seattle Heart Failure Model; MAGGIC: meta-analysis global group in chronic heart failure; 3C-HF: Cardiac and Comorbid Conditions Heart Failure score.
The SHFM and the MAGGIC scores are both validated in groups of patients without a predominance of severe MR and it is known that severe MR confers an increased risk of mortality.4 Therefore, we can speculate that the score would have underestimated the mortality and we expected that the observed survival would be lower than that predicted, because all patients included in our study were affected by severe MR. Instead, the observed survival after MitraClip was comparable with that predicted by the SHFM and MAGGIC scores, and therefore we can suppose that a certain benefit in terms of greater survival could have been conferred by the MitraClip procedure.
Considering that the 3C-HF score takes into consideration severe valve heart disease in the variables that contribute to outcome prediction, the observed survival after MitraClip is significantly higher than that predicted by the 3C-HF score and this can support the aforementioned hypothesis of outcome improvement after MitraClip, especially in non-ischaemic patients who seem to benefit the most from this procedure. Of course, a prospective, randomised, controlled trial is required to confirm these speculations.
In conclusion, the survival outcome of patients with FMR and HF, after the MitraClip procedure, was better than that predicted by the 3C-HF score and similar to that predicted by the SHFM and MAGGIC scores.








