BACKGROUND AND AIMS
The development of interventional cardiology is inevitably associated with increased dose of ionising radiation for the physician.1 Additionally, physiology-guided myocardial revascularisation is supported by both European and American experts,2,3 but these procedures may increase the total procedure time in addition to increased dose of ionising radiation for the physician.4 Therefore, the authors aimed this study to investigate the differences in dose of ionising radiation among fractional flow reserve (FFR), instantaneous wave-free ratio (iFR), and a novel minimally invasive FFR value computation method, quantitative flow ratio (QFR).
MATERIALS AND METHODS
In total, 134 patients who have undergone coronary angiography revealing intermediate lumen stenosis of 35–75% by visual estimation and for whom FFR, QFR, or iFR measurements were performed within 2020 have been prospectively included in this single-centre study. Dose area product (DAP) and fluoroscopy time (FT) were the parameters chosen for ionising radiation dose evaluation and comparison. Additionally, patient BMI was collected for unification. Statistical analysis was performed using software package SPSS 20.0® (IBM, Armonk, New York, USA). The chosen level of significance was p<0.05. Of all included functional assessment analyses, 48 were FFRs, 28 were QFRs, and 58 were iFRs. Mean BMI did not differ among groups: FFRs: 30.07, standard deviation (SD) ±6.26; QFRs: 27.14, SD ±4.61; and iFRs 29.75, SD ±5.05; p=0.08. BMI was moderately correlated to DAP (r=0.36; p<0.001). Mean FT and DAP for FFRs were 7.13 (SD ±5.82) min and 1928.63 (SD ±2137.21) cGy·cm2, respectively; for QFRs they were 2.44 (SD ±1.12) min and 923.12 (SD ±768.47) cGy·cm2, respectively; and for iFRs they were 6.50 (SD ±3.90) min and 1605.39 (SD ±1152.59) cGy·cm2, respectively. FT was almost double in FFRs and iFRs compared to QFR (p<0.001). Compared to FFR as a reference, DAP was half in QFR (p=0.012).
CONCLUSION
Since all currently available physiology assessment methods are equally accurate, reliable, and convenient on treatment decision-making, radiation safety aspects are one of the most important issues for further studies. QFR repeatedly shows promising results in significant ionising radiation dose reduction, resulting in shorter FT and DAP, irrespective of BMI; therefore it could become the method of choice in many clinical decision-making situations.
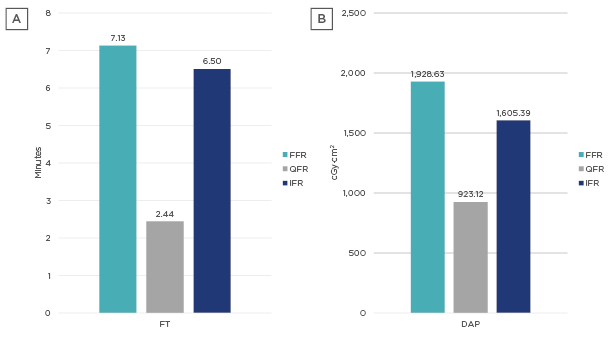
Figure 1: A) FT and B) DAP in FFR, QFR, and iFR procedure groups.
DAP: dose area product; FFR: fractional flow reserve; FT: fluoroscopy time; iFR: instantaneous wave-free ratio; QFR: quantitative flow ratio.








