Meeting Summary
The main objectives of this symposium were to explore the effect of light on individuals with hyperpigmentation disorders and acne, present the latest clinical research on the importance of photoprotection, and discuss the role of adapted photoprotection to improve patient adherence. Prof Passeron introduced the topic of hyperpigmentation by providing a brief background of pigmentary disorders and the mechanisms involved in ultraviolet (UV)B-induced pigmentation and the physiology of UVA pigmentation, and describing the latest findings from clinical studies that compared the effects of visible light and UVB on pigmentation and melasma. Dr Moyal presented the latest research on sun protection to prevent hyperpigmentation, focussing on the need for products to contain very high-level and well-balanced protection against UVA and UVB light, and discussed adherence, as well as how formulations can be adapted to meet patient needs by skin type, texture preference, and climatic requirements. Dr Moyal also presented the latest research on post-inflammatory hyperpigmentation (PIH) as a long-lasting sequela of acne, photoprotection to prevent drug-induced phototoxicity, and whether adapted dermocosmetics and photoprotection can be used to prevent acne outbreaks. Prof Trautinger provided an overview of the epidemiology, physiology, and interaction with light and presented studies regarding the effect that sunlight has on acne severity. Prof Trautinger also discussed why photoprotection is important for patients with acne, focussing on the phototoxic side effects of conventional acne treatment.
Photoprotection Needs for Patients with Hyperpigmentation Disorders
Professor Thierry Passeron
Pigmentary disorders affect ≤60% of the population, depending on the country and studies.1-3 It is one of the most frequent dermatological conditions across all phototypes1-3 (Fitzpatrick skin type determined by constitutional colour and exposure to UV radiation), with an impact on quality of life.4,5 Pigmentary disorders are more prevalent in dark-skinned individuals but can be observed in all phototypes.1-3 Accurate diagnosis is necessary to select the correct treatment and to assign effective photoprotection.
The colour of skin is determined by pigments, in particular: melanins, haemoglobin, and carotenoids. Melanins are composed of two main subtypes: eumelanins (photoprotective) and pheomelanins (not photoprotective and promote oxidative stress). When diagnosing a pigmentary disorder, it is important to determine whether it is vascular, owing to xeroderma, ochronosis, dyskeratosis, chromhidrosis, heavy metal deposition, exogenous pigments, or melanin hyperpigmentation.
More than 170 genes are involved in the control of human skin pigmentation. Exposure to UV light, particularly UVB, stimulates keratinocytes and activates downstream pathways that lead to an increase in melanin hormone production. The most important pathway is the alpha-melanocyte-stimulating hormone (a-MSH) pathway. UVA light pigmentation differs from that of UVB in that it does not confer a photoprotective effect.6 UVA light induces immediate pigment darkening, persistent pigment darkening, and delayed tanning;7 it has a deeper skin penetration compared with UVB (penetrates to the dermis and fibroblasts); and is known to cause oxidative stress.8 Photoprotection should have a UVA/UVB balance to prevent relapse of melasma.9 UVA is also suspected to play a key role in the late occurrence of actinic lentigines.
Studies of visible light exposure have demonstrated the role of visible light in skin ageing by a mechanism, at least in part, that involves inflammatory cytokines, the production of reactive oxygen species, and the activation of matrix metalloproteinases.10,11 However, it is the effect of visible light on hyperpigmentation that is of interest. Mahmoud et al.12 carried out a study of the effect of visible light compared with UVA radiation on healthy volunteers with phototypes IV and VI and demonstrated that visible light caused more intense and prolonged pigmentation than UVA1 radiation in darker phototypes (IV and VI) but had no effect on fairer phototypes (II).
A randomised controlled study of the pro-pigmenting effect of visible light at two distinct wavelengths (415 nm [blue-violet] and 630 nm [red]) in healthy volunteers with phototypes III and IV, demonstrated an increasing pigmentary effect with blue light and no pigmentary effect with red light (Figure 1).13 Results were determined by colourimetric measurements at 1 hour, 2 days, 8 days, 9 days, 15 days, and 22 days after exposure. Pigmentation was sustained for 22 days after exposure; therefore, to assess whether exposure had a long-term effect, volunteers were assessed at 3 months after exposure to reveal if pigmentation was present. Blue light was compared with UVB, which demonstrated pigmentation at 15 days after exposure to both wavelengths; however, 3 months after exposure, pigmentation was observed in those exposed to blue light but not to UVB. Histology revealed hypermelanosis with UVB and blue light, no significant melanocyte proliferation for blue light, and significantly higher keratinocyte necrosis, number of melanophages, and p53 activation in UVB exposure compared with blue light. Therefore, it can be concluded that the mechanism of pigmentation induced by visible light differs from the p53-induced mechanism of UVB pigmentation.
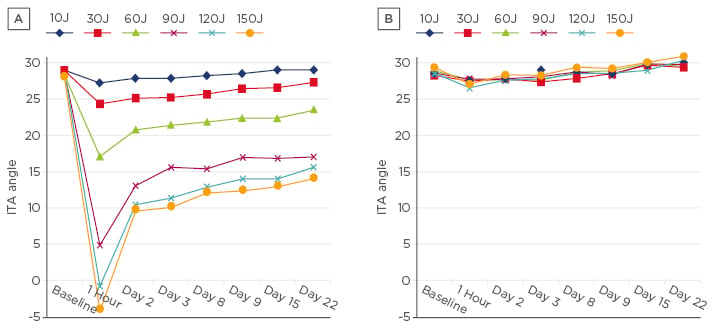
Figure 1: The effect of two wavelengths of visible light at multiple doses on individual typology angle, measured at time intervals after exposure.
A) 415 nm; B) 630 nm.
ITA: individual typology angle.
A prospective randomised study by Boukari et al.14 compared the effectiveness of UVA/UVB sun protection with UVA/UVB plus shorter wavelength visible light sun protection for the prevention of melasma relapse. Patients with melasma were assessed during 6 months of summer sun exposure and it was determined that fewer melasma relapses occurred in the group that used UVA/UVB plus shorter wavelength visible light protection than in those who used UVA/UVB protection. These clinical studies demonstrate the effects of visible light on pigmentation and on melasma. However, the impact of visible light on other pigmentary disorders is yet to be explored and is a topic for future research.
Towards a Broader Sun Protection for Patients with Hyperpigmentation Disorders
Doctor Dominique Moyal
Prevention of Pigmentation Induced by Ultraviolet A Light
Pigmentation is induced by UVA, UVB, and visible light, and effective sun protection should offer high-level and broad protection from UVA and UVB as a priority. In a comparative study, the effectiveness of products with the same sun protection factor (SPF) and a different UVA protection factor (UVAPF) was explored in a population of individuals with phototypes III and IV. The pigmentation protection factor was determined for each product. The UV source was representative of an average daily sun emission, with a higher UVA/UVB irradiance ratio compared with the UV source used for SPF determination (zenithal conditions).15 Patients were assessed 7 days after UV exposure (the time at which pigmentation is stable). Results demonstrated that, for the same SPF level, only products with a high UVAPF, a well-balanced UVA/UVB protection, and a SPF/UVAPF ratio <3 could prevent sun exposure-induced pigmentation (Table 1).
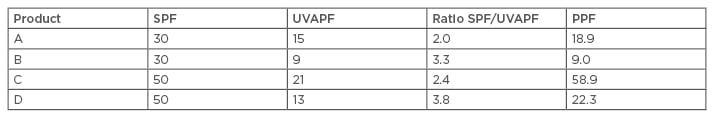
Table 1: Pigmentation protection factor determination.
PPF: pigmentation protection factor; SPF: sun protection factor; UVAPF: ultraviolet A protection factor.
The effectiveness of sun protection (Anthelios, SPF50+, UVAPF28, SPF/UVAPF=2.1) for the prevention of recurrence of melasma was studied in a trial of 185 pregnant women in Morocco.9 In women with phototypes II–V, 15% had a history of melasma, 6% presented with melasma at the start of the study, and 29% had facial PIH. Patients were monitored for the duration of their pregnancy with dermatological examination, Wood’s light examination, and colourimetric measurements at the beginning of pregnancy and at 3, 6, and 8 or 9 months. At the end of the study, five new cases (2.7%) of melasma were observed, compared to previous studies that demonstrated a 53% occurrence.16 At 6 months, clinical improvement was observed in 8 of the 12 patients affected by pre-existing melasma. Colourimetric measurements at 8–9 months revealed that 21% of patients had darker skin, 10% had identical skin colouration, and 69% had lighter skin than at enrolment. Overall, the occurrence of melasma decreased (preventative efficacy) and pre-existing melasma intensity was reduced (curative efficacy).
To confirm the results in another population, a study was carried out in 217 pregnant women in Korea with phototypes III and IV, using an Anthelios sunscreen (SPF50+, UVAPF30, SPF/UVAPF=2) for sun protection.17 Patients were followed up throughout pregnancy using colourimetric assessment, Melanin Index (Mexameter®, Courage + Khazaka Electronic, Cologne, Germany) and Melasma Area and Sensitivity Index (MASI) on the forehead, chin, and right and left malar. At the end of the study, 1% of women developed melasma with mild severity (MASI between 1.2 and 2.7) confirmed by colourimetric measurements. Overall, across the two studies it was confirmed that sun protection with high UVB and UVA broad protection (SPF/UVAPF=2) has preventative effectiveness against melasma.
It is known that UVA induces pigmentation through an oxidative mechanism, and to assess the value of using an antioxidant complex to prevent UVA-induced pigmentation a study of 20 individuals with phototypes III and IV was carried out. Patients were exposed to a single dose of long UVA at 50 J/cm2 on a non-treated area and on a treated area; the results, assessed using colourimetric measurements 24 hours after exposure, revealed significantly lower pigmentation induced by UVA on areas treated with antioxidant complex compared with untreated areas.
Prevention of Pigmentation Induced by Visible Light
Short wavelength visible light is known to cause pigmentation, and currently the only way to prevent visible light-induced pigmentation is by use of pigments such as iron oxides. To test the effectiveness of sun protection containing iron oxides, a trial comparing sun protection SPF60, SPF/UVAPF ≤2 with and without iron oxides was carried out. Ten patients with phototype IV (n=8) or V (n=2) were enrolled, each product was applied to a test zone, and one zone was untreated. Patients were exposed to visible light (400–700 nm) 30 minutes after application of sun protection, at doses ranging from 20–640 J/cm2. On Day 7, visual assessments and colourimetric measurements were carried out. Results revealed that pigmentation was significant but very low at visible light doses of ≤160 J/cm2; 160 J/cm2 was the minimal pigmenting dose. Test zones that were untreated demonstrated a high level of pigmentation (approximately -4 delta luminance at a visible light dose of 640 J/cm2), likewise test zones treated with sun protection and without iron oxides showed no difference with the untreated zones. Pigmentation of the test zones treated with sun protection containing iron oxides was significantly lower than its comparators.
Adapted Sun Protection for Improved Adherence
Sun protection strategies and formulations can only offer the expected protection if applied regularly in accordance with product recommendations. In a recent article18 it was shown that cosmetic elegance is the most important feature for consumers when considering sun protection, and should therefore be considered in the context of adherence, particularly for those who must use sun protection daily. Cosmetic elegance refers to a pleasant texture and easy-to-use formulation, which many high-level UVA/UVB products do not have. Adaptive formulations that are tailored to different skin types (such as oily or dry skin), different preferences and needs in texture (such as cream or ultra-light fluid), and different climatic conditions are necessary.
Photoprotection Needs for Patients with Acne
Professor Franz Trautinger
Overview of Acne
Acne is an inflammatory condition that is common in individuals aged 15–17 years old. In most people acne is relatively mild, however 15–20% develop moderate-to-severe acne. Acne is initially self-healing yet in a percentage of people it will continue into adult life.19 The pathophysiology of acne is well characterised despite the lack of an appropriate animal model, and is generally caused by the combination of inflammation, keratinisation of keratinocytes in the upper hair follicle, increased sebum production, and infection and colonisation with Propionibacterium acnes.20 When considering the interaction of electromagnetic radiation, whether it be UV, visible light, or infrared, and acne, it is important to think about whether there is a physical reaction and how deep it penetrates into the skin to interact with pilosebaceous units. UVA in particular can penetrate the deeper areas of the dermis and interact with pilosebaceous units. UVB can reach the epidermis and interact with keratinocytes and the upper area of the dermis.
Is Sunlight and Ultraviolet Light Good for Acne and Can it be Used as Treatment?
A popular misconception is that sunlight and UV light are good for acne and can be used as a treatment. In a study by Cafri et al.,21 college students were asked the reasons they used tanning beds, and a large number used them to treat acne. However, older studies, such as that by Gfesser and Worret,22 failed to demonstrate any significant variance between acne aggravation in the summer or winter months. A more recent study by Pascoe and Kimball23 surveyed doctors regarding the number of patient visits for almost-clear and moderate/severe acne throughout a year. Results revealed a minor seasonal effect, with a slightly higher percentage of patients presenting with severe acne in the winter months; however, the methods had many confounding factors (such as the number of visits was recorded instead of the number of patients).
Phototherapy for the treatment of acne has been studied in numerous trials with small patient numbers,24,25 and, although the evidence is poor, there seems to be no benefit from broad-band and monochromatic visible, UV, or infrared sources alone. There is some benefit if a photosensitiser is added, so photodynamic therapy with 5-aminolevulinic acid or methyl aminolevulinate might have an effect. However, when compared with conventional acne treatment, there is no superiority.24
Why Recommend Photoprotection for Acne?
Photoprotection should be recommended for patients with acne for three main reasons: to prevent skin cancer and photoageing, as in the general population; to protect patients with acne from the negative effects of treatment-associated photosensitivity, and to prevent long-lasting PIH.
Acne treatment conventionally includes topical and systemic retinoids, topical benzoyl peroxide (BPO), and systemic tetracyclines. Studies to assess the phototoxic effects of systemic retinoids have failed to demonstrate a photosensitising effect,26 which differs from experience in daily practice, and data on topical retinoids and BPO are limited. However, the package inserts and product characteristics recommend photoprotection.27-29 Systemic tetracyclines, most commonly doxycycline, are known to cause photosensitisation in ≤20% of patients,30-32 depending on the environment and behaviour of the patient. A study by Hasan et al.33 demonstrated doxycycline degradation with increasing exposure to UVA radiation, and Duteil et al.34 provided evidence that broad-spectrum photoprotection against UVA is especially important in protecting patients from phototoxic skin rash. Photoprotection is necessary to prevent PIH in all patient populations, particularly in individuals with darker skin in whom incidence can be ≤65% and treatment is unsatisfactory.35
In conclusion, all patients with acne should be counselled regarding appropriate photoprotection, and common myths surrounding acne treatment with sunlight should be addressed. Patients should be advised to avoid sunbathing and tanning beds, encouraged to wear protective clothing such as hats, and advised to wear broad-spectrum photoprotection, especially when photosensitising treatment is prescribed. Acne treatment, if topical, should be applied first, followed by photoprotection. The level of SPF should be based on the individual’s skin type, geographic location, and type of leisure activity. Patients should also undergo regular assessment of their acne and use of photoprotection should be reaffirmed.
Towards Adapted Sun Protection for Patients with Acne
Doctor Dominique Moyal
Tetracyclines and systemic retinoids as treatment for acne have been demonstrated to induce phototoxicity. Therefore, several clinical studies have been carried out to prove that sun protection can prevent such side effects. A study of 35 patients with acne treated with doxycycline or lymecycline compared the efficacy of the Anthelios sunscreen SPF50+ UVAPF28 with the vehicle (the excipient of the sunscreen, i.e. all ingredients except the UV filters) to prevent tetracycline-induced phototoxicity.34 Patients were exposed to UVA radiation on their backs, and the minimal phototoxic dose for each individual was determined. Patients were exposed to UVA doses of 0.75, 1.0, and 1.25 minimal phototoxic dose on areas treated with sunscreen or vehicle product, and assessed 24 and 48 hours after exposure for clinical signs of erythema and colourimetric measurements. Visual scoring (Figure 2) and colourimetric assessment revealed that minimal erythema appeared in areas treated with the sunscreen versus the vehicle product (differential colourimetric redness score of 1.5 versus 4.3, respectively, at 1.0 minimal phototoxic dose). A second study explored the effectiveness of a sunscreen SPF60+ for the prevention of phototoxicity in 26 patients with severe acne treated with isotretinoin. Patients’ acne was evaluated using the Cook Index (0–9 scale)36 at the start of the study and at the end of the summer season (4 months later). At the end of the season, the intensity of acne was reduced (mean Cook Index score: 2.6) compared with the start of the study (mean Cook Index score: 7.1) with no adverse effects. These results demonstrated that the use of effective sun protection was beneficial in avoiding the side effects of isotretinoin.
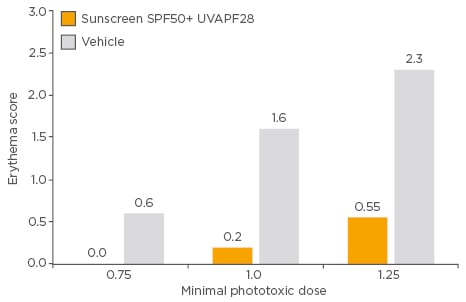
Figure 2: Erythema score after exposure to ultraviolet A radiation in patients treated with tetracycline, using a sunscreen SPF50+ UVAPF28 or vehicle product.
SPF: sun protection factor; UVAPF: ultraviolet A protection factor.
PIH is a common sequela of acne and can be long-lasting. An observational study carried out in >5,000 patients with acne (phototypes II [47%] and III [39%]) across 11 countries found that 76% of patients had residual colour marks that were erythematous, pigmentary, or both. A second observational study of 3,800 patients with acne was carried out and included patients with darker skin (phototype II: 40%, phototype III: 41%, phototype IV: 12%). It was determined that residual erythematous, pigmentary, or combined marks were present in 74% of patients. To explore whether there is a link between severity of acne and PIH, patients were stratified into mild acne and moderate acne groups and assessed for residual marks. More patients with moderate acne had residual marks (81.9%) than those with mild acne (57.5%). The results confirmed that PIH was common in patients with acne, especially in individuals with severe acne and with darker skin, and that photoprotection is important in preventing intensified pigmentation after sun exposure.
To explore whether adapted dermocosmetics and photoprotection can be used during the summer to avoid acne outbreaks, 337 patients who were at the end of local or systemic medical treatment were evaluated for acne outbreaks and severity. Patients with phototypes II–IV were included and prescribed an anti-acne dermocosmetic (Effaclar DUO+) and a sunscreen with SPF30 and UVAPF25 developed for oily skin (Anthelios AC) for 90 days during the summer. Acne evaluation was carried out at the start of the study and 90 days after beginning treatment. At baseline, 70% of patients had no or almost no lesions, 21% had low-level acne, and 9% had moderate acne, and at Day 90, 81% of patients had no or almost no lesions, 17% had low-level acne, and 3% had moderate acne, which corresponded with a significant decrease in acne severity (overall, 45% experienced a decrease in acne severity, 45% experienced no change, and 10% an increase).
In conclusion, PIH is often associated with acne and UVA has an important role in increasing hyperpigmentation, and photoprotection can potentially offset and prevent dermatological side effects of acne treatments. Acne can worsen with sun exposure, and prescription of photoprotection to and adherence from patients is insufficient. Photoprotection should provide high-level protection from UVA and UVB radiation, be non-comedogenic, and textures should be adapted to the needs of the patient.







